Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) patients as well as genotype positive/phenotype patients are recommended to avoid high intensity and competitive sports according to the European Society of Cardiology guidelines based on an increased risk of sudden death and deleterious effect on the myocardium.1–3
On the other hand, these patients should not be excluded to the clear benefits of low-to-moderate physical activity and cardiologist with expertise in cardiomyopathies should provide exercise prescription adapted to the underlying cardiac condition but also to patients’ goals. This brief article is aiming to help regarding this challenging issue.
Baseline assessment
Tailored exercise prescription should always start from a baseline assessment of the severity of the disease with a special attention to arrhythmic risk. Previous history of syncope, frequent ventricular ectopies (> 500/24h), significant structural involvement (i.e: right ventricular systolic dysfunction, or fibrosis) and exercise-induced complex ventricular arrhythmias are identified risk factors: in the presence of them only low or very low intensity exercise could be prescribed. In the opposite, Moderate-intensity exercise can be considered in patients with very low arrhythmic risk.2 In the gray zone, exercise testing can help especially for patients planning to engage in moderate or intense physical activity beyond recommendations. Careful clinical and rhythmic evaluation and follow-up remain mandatory for such patients. Despite evidence about the role of sport in ARVC is mostly based on enriched PKP2 cohorts, recommendations are extensive to other ARVC cases irrespective of the genetic substrate.
Type and Quantity of Exercise
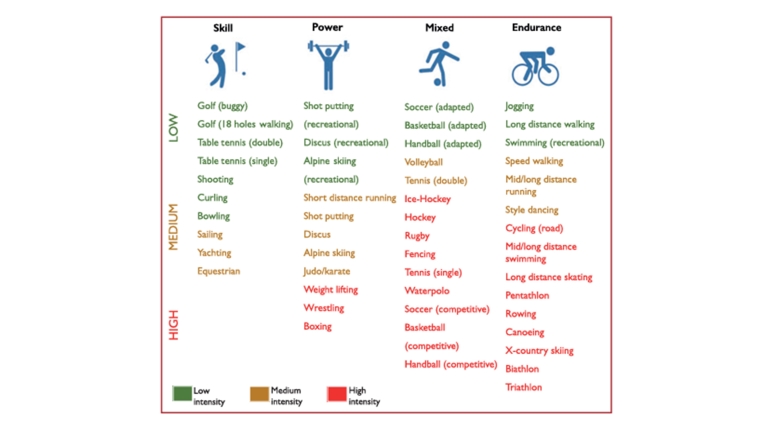
Sports intensity is difficult to define due to many variables involved such as age, skill or competitiveness. Nevertheless, ESC Sports Guidelines propose a classification for different disciplines that can serve as a starting point. In addition, maximum heart rate during exercise can also indicate the intensity. Overall activities that keep maximum heart rate under 55% of predicted by age (220 –age) are considered low intensity.2
Sporting discipline in relation to the predominant component (skill, power, mixed, and endurance) and intensity of exercise. Extracted from 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Pelliccia et al. 2020
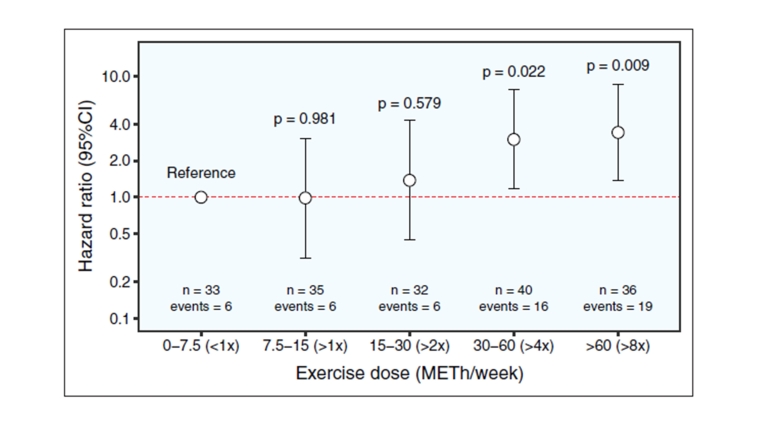
Beyond intensity, it’s important to keep in mind that the cumulative number of hours of exercise seems to be a predictor of arrhythmic events.4 Consequently, a prudent recommendation emerges, advising against engaging in very frequent exercise sessions, even when characterised by low intensity, due to their potential association with an increased risk of arrhythmic events.
Dose-dependent association of exercise dose and sustained ventricular arrhythmia risk. Extracted from Integrating Exercise into Personalized Ventricular Arrhythmia Risk Prediction in Arrhythmogenic Right Ventricular Cardiomyopathy. Bosman et al. 2022.
Tailoring Recommendations to Individual Patient Profiles
Exercise recommendations must be tailored to the individual patient's profile, recognizing that a one-size-fits-all approach may not be appropriate.
Encouraging Sedentary Individuals:
For patients who lead a sedentary lifestyle or engage in minimal physical activity, the focus should be on encouraging and gradually introducing low-intensity exercises. Initiating activities like brisk walking or light stretching can be a positive first step.
Moderating High-Intensity Activities:
Patients already engaging in high-intensity exercise should be counselled on moderation. Adjustments in frequency, duration, or intensity may be necessary to minimize the risk of triggering arrhythmias.
Consideration of Patient Goals in Exercise Recommendations
Recognising that each patient may have unique goals and expectations from engaging in physical activity is paramount. Prior to prescribing exercise, healthcare providers should engage in a thorough discussion with the patient to understand their motivations and desired outcomes.
Health Improvement:
Some patients may prioritize overall health improvement. In such cases, low-to-moderate intensity exercises that focus on cardiovascular fitness, flexibility, and balance, such as walking, yoga, or swimming, could align well with these goals.
Social Engagement:
For individuals seeking social interaction, recommending group activities like group fitness classes, cycling clubs, or recreational sports can contribute to both physical and social well-being.
Stress Reduction and Relaxation:
Patients aiming to manage stress and promote relaxation may find activities like tai chi, gentle yoga, or meditation beneficial. These practices not only cater to cardiovascular health but also emphasize mental well-being.
Examples of exercise prescription for ARVC patients
Taking all the previous considerations we provide a list of low-intensity exercise prescriptions for patients with ARVC.
- Walking and Hiking:
- Frequency: At least 150 minutes per week.
- Conditions: Avoid dehydration and sloping routes.
- Swimming:
- Frequency: Two to three times per week.
- Conditions: Controlled pools with adequate supervision.
- Recreational Cycling:
- Frequency: Two to three times per week.
- Conditions: Flat terrains.
- Yoga and Stretching:
- Frequency: Two to three times per week.
- Conditions: Avoid dehydration
- Low-Intensity Aerobics:
- Frequency: Three times per week.
- Conditions: Well-ventilated spaces.