Take-home messages
- Anthracyclines, HER2-therapies and fluoropyrimidines may exert asymptomatic left ventricular dysfunction, overt heart failure, acute coronary syndromes, and rhythm disturbances.
- A tailored surveillance during treatment according to baseline CV risk is recommended for early detection of cardiovascular toxicity and a prompt treatment of its complications.
- Chest pain, coronary vasospasm and acute coronary syndromes can occur within days of fluoropyrimidine exposure. Risk factors include pre-existent coronary disease, but it may occur even in normal coronary arteries.
- Strict control of cardiovascular risk factors is recommended during all cancer pathways of care.
Patient-oriented message
- Most common anticancer therapies may have a toxic effect on the cardiovascular system, causing heart failure, anginal pain, or arrhythmias.
- Correction of cardiovascular risk factors and a healthy lifestyle, combined with a clinical and instrumental surveillance, appropriate to the level of risk, are key elements in preventing these complications.
- In case of their occurrence, early diagnosis and timely treatment make it possible to manage them without leaving lasting consequences.
Impact on practice statement
During cancer treatments, strict control of cardiovascular risk factors is pivotal to prevent the development, in the first instance, or reduce the incidence of toxic effects on the cardiovascular system.
According to baseline cardiovascular risk, a tailored clinical and instrumental surveillance, including trans-thoracic echocardiogram and cardiac biomarkers, is recommended for early detection of cardiovascular toxicity and a prompt treatment of its complications.
Anthracyclines
Cardiotoxicity monitoring
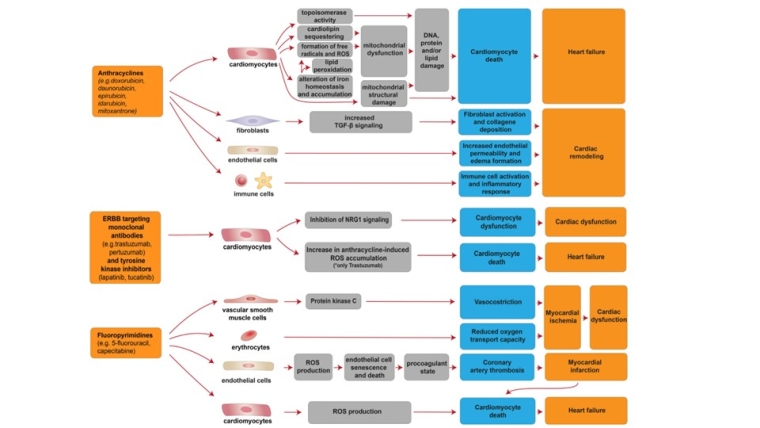
Anthracyclines remain the cornerstone of treatment for many solid and haematological malignancies, but they also are the chemotherapeutic drugs most usually associated with a cardiotoxic impact [1-4]. The specific mechanisms of anthracycline cardiotoxicity still remains unclear, and are likely multifactorial (Central illustration).
Central illustration. Cellular and molecular mechanisms of the cardiotoxic effects exerted by anthracyclines, ERBB targeting monoclonal antibodies and tyrosine kinase inhibitors, and fluoropyrimidines. Modified with permission from Morelli et al [1]. Morelli MB, et al. Cardiotoxicity of anticancer drugs: molecular mechanisms and strategies for cardioprotection. Front Cardiovasc Med. 2022;9:847012.
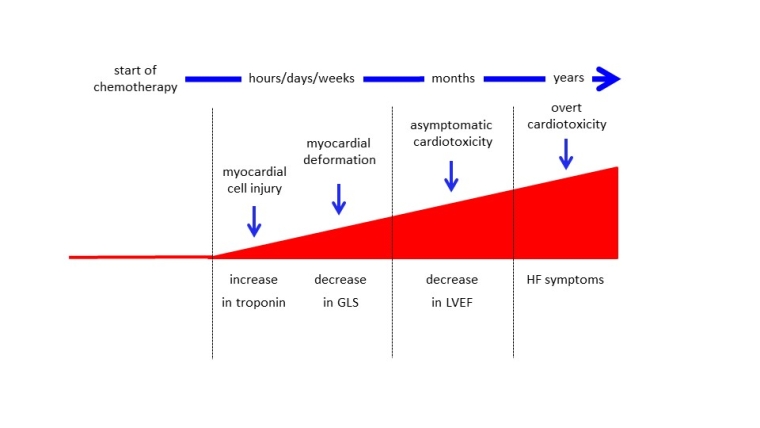
Anthracycline-induced cardiotoxicity (AIC) is most likely a continuous phenomenon that begins with myocardial cell injury, detectable only by dosing circulating biomarkers, followed by asymptomatic left ventricular ejection fraction (LVEF), which, if ignored and not treated early, progressively leads to symptomatic heart failure (HF) (Figure 1). Regardless of oncological prognosis, the emergence of anthracycline-cardiomyopathy may significantly impact the quality of life and survival of cancer patients [5].
Figure 1. Schematic representation of cardiotoxicity progression: the continuum phenomenon hypothesis. Modified with permission from Cardinale et al [5] Cardinale D, Biasillo G, Cipolla CM. Curing Cancer, Saving the Heart: A Challenge That Cardioncology Should Not Miss. Curr Cardiol Rep. 2016;18:51.
GLS: Global longitudinal strain; LVEF: left ventricular ejection fraction; HF: heart failure
Cardiotoxicity induced by anthracyclines can be diagnosed during an asymptomatic phase. Recent research using a large (n=2,625) unselected population scheduled to get anthracycline therapy revealed that careful monitoring of LVEF following chemotherapy allowed nearly all (98%) cases of cardiotoxicity to be recognised within the first 12 months of follow-up [6]. The majority of patients with AIC (81%) were asymptomatic, and AIC was identified during routine LVEF echocardiographic examinations. Moreover, early therapy with angiotensin-converting enzyme (ACE)-inhibitors (enalapril) and beta blockers (carvedilol or bisoprolol) normalised cardiac function in the majority of instances (82%). However, only 11% of patients with renormalised LVEF exhibited complete recovery, i.e., the same LVEF value as before the initiation of anthracyclines, whereas the final LVEF value in 71% of patients remained below the baseline value.
These results demonstrate that this strategy is insufficient for diagnosing reversible cardiotoxicity, possibly because left ventricular compensating mechanisms are already exhausted [2]. In contrast, evidence of a normal LVEF did not eliminate the possibility of developing heart dysfunction in the future.
Utilising cardiac biomarkers, a novel strategy for the early diagnosis of preclinical cardiac injury has been proved to be a successful alternative [7]. Troponins and natriuretic peptides (NP) are the most extensively researched biomarkers for AIC. In addition to imaging techniques, troponins and NP (BNP, NT-proBNP) may be useful in identifying people at risk for AIC. This method is minimally invasive, cost-effective, and does not rely on operator-dependent imaging techniques. Troponins appear to be better able to detect early myocardial injury, whereas NP appear to be better able to detect asymptomatic cardiac dysfunction that occurs later. Notably, regular troponin tests and early treatment with ACE-inhibitors have proven to be highly beneficial in reducing cancer therapy-induced cardiac dysfunction and related cardiac events in individuals with elevated troponin levels [8].
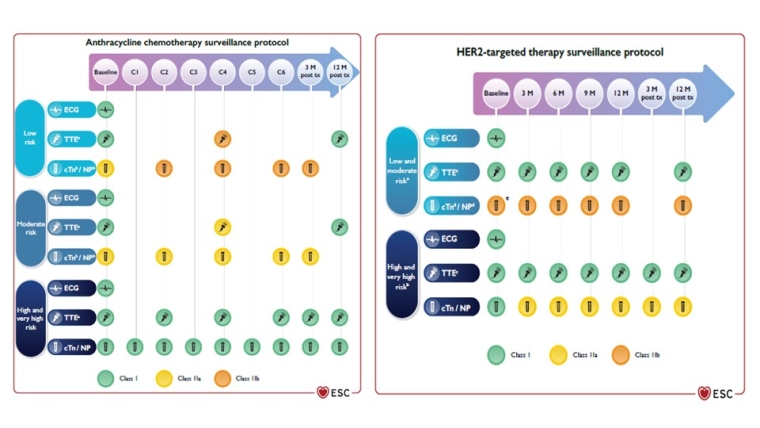
Very recently, troponins and NP were added to the field of cardio-oncology and their use was recommended in the guidelines [3,4,7]. In the recent publication of the first version of the ESC Guidelines on cardio-oncology, an integrated approach to biomarkers and cardiac imaging for monitoring cardiotoxicity in anthracycline-treated patients is suggested [4]. Figure 2 outlines the recommended monitoring protocol during anthracycline therapy based on cardiovascular risk at baseline (for more details on baseline risk evaluation see Volume 2, February edition of CardioPractice :
- Risk Stratification and prevention strategies in cardio-oncology
- End of term evaluation and management of cancer patients at the end of therapy - video
- End of therapy risk assessment and management - part 1
- Cardiovascular toxicity risk stratification and preventive strategies - video
Clinical evaluation in conjunction with troponins, NP, and transthoracic echocardiography (including 3D-LVEF and global longitudinal strain, if available) can identify symptomatic and asymptomatic AIC with a reasonably good negative predictive value.
Figure 2. Cardiovascular toxicity monitoring in patients receiving anthracycline chemotherapy or human epidermal receptor 2-targeted therapies according to patient’s baseline cardiovascular toxicity risk. Reproduced with permission from [4]. Lyon AR, et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur Heart J. 2022;43:4229-361.
cTn: cardiac troponins; ECG: electrocardiogram; HER2: human epidermal receptor 2; NP: natriuretic peptides; TTE: transthoracic echocardiogram
As the majority of AIC cases occur within the first year after chemotherapy [6], examinations at 6 and/or 12 months post-chemotherapy should also be considered [3,4].
Treatment of anthracycline-induced cardiotoxicity
Recent research indicates that cardiomyopathy due to AIC may actually be reversible [2]. The efficiency of ACE-inhibitors and beta blockers was prospectively evaluated in 201 patients with AIC; an inverse association was discovered between the time interval between the end of chemotherapy and the onset of HF therapy in terms of LVEF improvement [9]. It appears that AIC is in fact not irreversible, but that its reversibility is dependent on early diagnosis and timely treatment. Contrariwise, close monitoring permits early detection of AIC and timely treatment with HF medications, resulting in the majority of cases, in normalisation of LVEF linked to a concurrent decrease in cardiac events.
A greater improvement in cardiac function was observed in patients receiving a combination of ACE-inhibitors and beta blockers than in those receiving either treatment alone. This emphasises the importance of always considering and attempting a treatment based on the combination of these two types of medicines in all patients developing AIC [6,9].
However, it has been questioned for many years whether the use of ACE-inhibitors and beta blockers, as advised by cardiologic recommendations worldwide, might be applied to this particular clinical context with comparable long-term benefit. In addition, the asymptomatic nature of AIC is a crucial point of discussion. [6,9]. So far, only monitoring programmes for HF symptoms have been proposed, and the management of AIC has mostly centred on the symptomatic patient. The question of whether or not to treat asymptomatic patients with left ventricular dysfunction detected by routine screening tests has been highly debatable, until today.
Just recently, the ESC's new Cardio-Oncology Guidelines finally stated that patients with symptomatic and asymptomatic AIC should be treated according to the worldwide guidelines in the same manner as the general HF population [4].
HER2-targeted therapies
Cardiotoxicity monitoring
Human epidermal growth factor receptor 2 (HER2)-targeted drugs have significantly enhanced the recurrence rates and survival of patients whose tumours overexpress this receptor [10]. Several anti-HER2 medications are now available, and others are under development: trastuzumab and pertuzumab (monoclonal antibodies), trastuzumab-emtansine (monoclonal antibody coupled to a chemotherapeutic drug), trastuzumab-deruxtecan (monoclonal antibody conjugated to a topoisomerase I inhibitor), and the tyrosine kinase inhibitors lapatinib, neratinib, and tucatinib. Unfortunately, it is known that anti-HER2 therapy might cause asymptomatic or overt LVEF decline (Central illustration).
Unlike anthracycline, cardiotoxicity induced by anti-HER2 agents often occurs during and not after treatment. Consequently, its occurrence can result in long-term suspension of medication, potentially leading to incomplete treatment and a rise in recurrences [11].
Left ventricular function surveillance based on LVEF (and GLS when available) is indicated at baseline and every 3 months during therapy in patients receiving HER2-targeted medications (Figure 2) (4,12). Similar to the monitoring throughout anthracycline treatment, a surveillance tailored to the patient's cardiovascular toxicity risk at baseline is recommended. Patients initiating trastuzumab alone, trastuzumab and pertuzumab, trastuzumab emtansine, or oral HER2-targeted treatments should undergo imaging at the same frequency [12].
Patients with increased troponin values are more likely to develop trastuzumab-induced cardiotoxicity and are less likely to recover from cardiac dysfunction, despite adequate HF therapy [7]. Detectable high sensitivity cardiac troponins I (hs-cTnI) at 3 months after the commencement of anthracycline-containing therapy followed by trastuzumab in patients with HER2+ early stage breast cancer may predict ensuing development of left ventricular dysfunction [7].
However, monitoring troponins does not appear to be useful for detecting cardiotoxicity following treatment with trastuzumab without anthracyclines. Overall, the evidence suggests that troponin levels rise more frequently during the initial administrations of trastuzumab and then declines as treatment continues. This would suggest that the increase in troponin is related to delayed myocardial damage caused by earlier chemotherapy with other cardiotoxic medicines, rather than direct damage caused by trastuzumab, which likely works as a precipitant. In accordance with this concept, among 251 breast cancer patients, troponin increased exclusively in those previously treated with anthracycline and trastuzumab, whereas no increase was detected in patients treated with trastuzumab alone [13].
During trastuzumab therapy, NP (BNP, NT-proBNP) may detect new, asymptomatic left ventricular dysfunction with greater sensitivity than troponin [7].
Treatment of cardiotoxicity induced by HER2-targeted agents
The clinical prognosis of HER2-targeted drug-induced cardiotoxicity appears less severe than that of anthracyclines: cardiac function often improves after HER2-targeted drug withdrawal and the initiation of HF treatment [13]. In the past, individuals with HER2-targeted drug-induced cardiotoxicity were not treated uniformly, and there have been no prospective randomised trials assessing the role of medical HF therapy. Current recommendations focus mostly on the continuation/withdrawal/resumption of HER2-targeted medications based on the LVEF value of the patient. Several algorithms have been proposed, but their validity must be confirmed in large, prospective, long-term research [3,12,13]. Case series are the only available evidence for the use of ACE-inhibitors and beta blockers in this therapeutic scenario.
In clinical practice, therefore, the decision to employ these drugs to treat patients with an asymptomatic fall in LVEF may vary from case to case and is largely dependent on the personal clinical experience of cardiologists and oncologists. The new ESC Cardio-Oncology Guidelines [4] recommend initiation of heart failure therapy in moderate to severe asymptomatic and in symptomatic cancer therapy-related cardiac dysfunction (CTRCD) induced by HER-2 therapies.
Notably, in the majority of cases following the initiation of therapy with ACE-inhibitors and beta blockers, the resumption of trastuzumab is not necessarily followed by a new development of left ventricular dysfunction or HF, allowing the continuation of this important cancer therapy without compromising the patient's cardiac status. Troponin, by identifying people at a higher risk for developing trastuzumab-induced cardiotoxicity, could assist in those selecting patients who are less likely to recover from cardiac dysfunction and who require more intensive surveillance and a more intensive HF treatment [3,12,13].
In patients with evidence of cardiotoxicity during HER-2 inhibitor therapy, a targeted cardio-oncological approach that includes assessment of cardiac biomarkers at each cycle and strict LVEF monitoring could positively influence the oncological management of patients after resumption of the drug, reducing the potential for adverse cardiovascular effects and improving outcome [11].
Fluoropyrimidines
Cardiotoxicity monitoring
Fluoropyrimidines are antimetabolite drugs and include 5-fluorouracil (5-FU), applied as intravenous continuous infusion or bolus, and the oral prodrug capecitabine. They are a major cornerstone of many solid tumours involving the head, neck, gastrointestinal tract, bladder, and also advanced breast cancer as well as a standard treatment of advanced colorectal cancer. However, fluoropyrimidines are the second most common agents causing cancer therapy-related cardiovascular toxicity (CTR-CVT) ranking after anthracyclines and occur in 1-19% of exposed patients.
The predominant clinical presentation most common includes acute chest pain, myocardial infarction, acute cardiomyopathy with heart failure, or ventricular arrhythmias and, less frequently, cardiogenic shock or sudden death [14]. Angina pectoris frequently occurs early within days after fluoropyrimidine administration and may lead to electrocardiogram (ECG) ST changes with troponin elevation, causing interruption of the cancer treatment. Myocardial infarction can occur also in patients without previous coronary disease and normal coronary arteries [15].
The mechanisms of 5-FU-induced CTR-CVT are multifactorial (Central illustration), especially vascular toxicity with coronary vasospasm and coronary endothelial dysfunction, but also direct myocardial toxicity or inflammatory response with myocarditis, and Takotsubo cardiomyopathy [16]. Impaired vasodilation of vascular smooth muscle may be generated by endothelial injury and lead to a procoagulant state.
The risk of CTR-CVT in fluoropyrimidines is increased in cancer patients with pre-existing coronary disease or cardiac comorbidity [3,4,17]. Hypercholesterolemia, hypertension and smoking have also been related to increased risk [17, 18]. Strenuous physical activities can also trigger ischemia or ventricular arrhythmias [19].
At baseline, cardiac risk should be assessed before starting 5-FU or derivatives (Table 1) [3,4]. All modifiable cardiovascular risk factors, such as elevated lipids, glucose levels or blood pressure should be aggressively and promptly treated according to the current ESC guidelines for patients undergoing and post-fluoropyrimidine treatment.
Table 1. Recommendations for baseline risk assessment and monitoring during fluoropyrimidine therapy. Reproduced with permission from [4]. Lyon AR, et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur Heart J. 2022;43:4229-361.
- Baseline cardiovascular (CV) risk assessment and evaluation—including:
- Blood pressure (BP) measurement
- ECG
- Lipid profile
- HbA1c measurement
- SCORE2/SCORE2-OP or equivalent
- is recommended before starting fluoropyrimidines.
- Class: I
- Level: C
- A baseline echocardiogram is recommended in patients with a history of symptomatic cardiovascular disease (CVD) before starting fluoropyrimidines.
- Class: I
- Level: C
- Screening for coronary artery disease (CAD) may be considered in patients at high and very high risk of CAD before fluoropyrimidines.
- Class: IIb
- Level: C
*Prompt control of modifiable cardiovascular risk factors is strongly recommended.
BP: blood pressure; CAD: coronary artery disease; CV: cardiovascular; CVD: cardiovascular disease; ECG: electrocardiogram; HbA1c: glycated haemoglobin; SCORE2: Systematic Coronary Risk Estimation 2; SCORE2-OP: Systematic Coronary Risk Estimation 2—Older Persons; SCORE2 (<70 years) or SCORE2-OP (≥70 years) CV risk stratification: <50 years: low risk <2.5%, moderate risk 2.5% to 7.5%, high risk ≥7.5%, 50–69 years: low risk <5%, moderate risk 5% to <10%, high risk ≥10%; ≥70 years: low risk <7.5%. moderate risk 7.5% to <15%, high risk ≥15%
Imaging screening for ischaemia may be considered in situations with clinical suspicion or symptoms of coronary disease, with coronary CT or nuclear myocardial perfusion imaging, stress echocardiography/cardiac MRI, as available, prior to the start ‒ without delaying the initiation of the chemotherapy ‒ to rule out obstructive coronary disease [4].
During fluoropyrimidines treatment, ECG should be performed if any cardiac symptoms or angina occur, followed by troponin measurement, echocardiography for new wall motion abnormalities, as well as coronary CT where indicated. Holter monitoring can detect arrhythmias during therapy.
Treatment and management of cardiotoxicity induced by fluoropyrimidines
In acute coronary syndromes or chest pain with or without serum troponin increase, discontinuation of 5-FU or derivatives and exclusion of severe coronary stenosis by CT or coronary angiography are mandatory. Treatment of acute myocardial infarction should follow the current ESC guidelines. Monitoring should be implemented when severe cardiac symptoms occur, in order to detect any potentially lethal ventricular arrhythmias.
A rechallenge may be considered in individual cases after multidisciplinary discussion, with cardiac monitoring and prophylactic long-acting nitrates and calcium channel blocker therapy [4].
Rechallenge Strategies may include fluoropyrimidine dose reduction or modified schedules with short 5-FU infusions, concomitant anti-ischaemic medication, and avoiding physical effort. Lipids, hypertension and other risk factors should be strictly controlled.
Other simultaneous cancer therapies leading to increased vascular toxicity and coronary atherosclerosis risk should also be considered, as possibly additive in the context of fluoropyrimidines (Table 2).
Table 2. Cancer treatments that predispose to acute coronary syndromes and vascular toxicity. Reproduced with permission from [4]. Lyon AR, et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur Heart J. 2022;43:4229-361.
- Accelerated atherosclerosis and plaque rupture
- Associated treatments:
- ADT (GnRH agonists)
- ICI
- Nilotinib
- Ponatinib
- Radiation therapy
- VEGFi
- Vasospasm
- Associated treatments:
- Bleomycin
- Fluoropyrimidines
- Taxanes
- VEGFi
- Vinca alkaloids
- Associated treatments:
- Coronary thrombosis
- Associated treatments:
- Alkylating agents (cisplatin, cyclophosphamide)
- Erlotinib
- ICI
- IMiD (lenalidomide, thalidomide)
- Monoclonal antibodies (VEGFi, anti-CD20)
- Nilotinib
- Platinum chemotherapy
- PI ponatinib
- VEGFi
- Associated treatments:
ADT: androgen deprivation therapy; GnRH: gonadotropin-releasing hormone; ICI: immune checkpoint inhibitors; IMiD: immunomodulatory drugs; PI: proteasome inhibitors; VEGFi: vascular endothelial growth factor inhibitors.
Close cardio-oncology follow-up and collaboration in any CTR-CVT during fluoropyrimidines is necessary to avoid severe or lethal complications and in order to find the optimal cancer therapy for these patients.