Take-home messages
- Common cardiovascular complications may lead to loss of independence and a higher degree of frailty and may predispose patients to or facilitate new falls.
- After hip fractures and subsequent hip surgery, there should be a focus on avoiding geriatric complications (delirium, worsening of sarcopenia due to immobilisation).
- After hip fracture and surgery, there should be a focus on avoiding worsening of pre-existing cardiovascular diseases.
- After hip fracture and surgery there should be a focus on avoiding cardiovascular complications that may be associated with surgery.
- The careful management of such a risky and challenging period may favour a complete recovery.
Introduction
Ageing is closely related to multimorbidity and frailty. The global population is getting older, and it is calculated that between 2015 and 2050, the proportion of the world's population over 60 years of age will nearly double, from 12 to 22% [1]. Therefore, managing successful ageing has become a front-line goal for healthcare systems given the large expenditures associated with chronic diseases in terms of economic and social problems that can fall on families and caregivers.
Falls and hip fractures are events that can have dramatic consequences in older adults. Perioperative adverse cardiac events in older patients with hip fractures are associated with perioperative and post-discharge mortality, with major adverse cardiovascular events being the leading cause of death with a high – 20 to 40% – one-year mortality rate in older patients with hip fractures [2-5]. The geriatric evaluation of patients hospitalised for hip fractures has been associated with cost-saving and reduced 1-year mortality [6]. Recently, a Clinical Consensus Statement from the European Society of Cardiology (ESC) pointed to the specific needs, regarding the prevention and management of the frequent cardiovascular complications, in older patients undergoing hip orthopaedic interventions [7]. This statement complements the 2022 ESC Guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery [8]. A few crucial points on peri- and post-operative care discussed in the recently published clinical consensus statement [7] are summarised in the present report, with a comment on patient/caregiver perspectives.
It is advised to consider the following points in patients admitted with hip fracture:
- previous cardiovascular diseases that may be responsible for falls (alone or as a concomitant factor);
- previous cardiovascular diseases that may increase surgical risk and favour cardiovascular complications;
- frailty evaluation;
- evaluation of the risk of major geriatric complications that may jeopardise clinical outcomes (e.g. post-operative delirium).
Previous cardiovascular diseases that may be responsible for falls and/or increase surgical risk
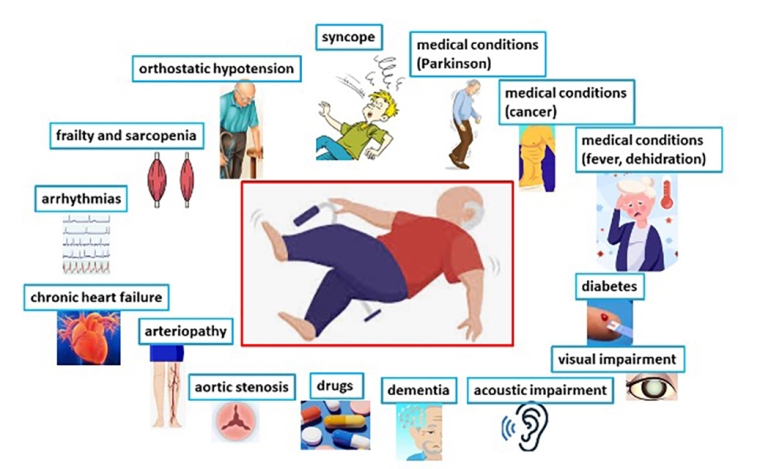
Cardiovascular diseases are connected to falls and the subsequent need for hip surgery after fractures (Table 1, Figure 1).
Cardiovascular diseases that may be responsible for falls.
- Syncope
- Orthostatic hypotension
- Arrhythmias
- Aortic stenosis
- Chronic heart failure
- Peripheral artery disease
Factors that may be responsible for – or favour – falls in older patients
- Frailty
- Dementia
- Visual deficits
- Vestibular dysfunction/Balance impairments
- Diabetes
- Non-cardiovascular diseases (cancer, etc.)
- Acute diseases (infections, fever, prolonged lack of food and liquids)
- Drugs
Figure 1. Medical conditions associated with falls.
It is important to identify the potential cause of falls in order to avoid perioperative and late consequences of underlying cardiovascular diseases. Similarly, it is relevant to identify chronic or acute cardiovascular diseases that may occur in patients with a hip fracture.
The decision to intervene in severe or unstable cases of ischaemic or valvular heart disease (e.g. coronary revascularisation or valve replacement procedure) prior to hip surgery must be weighed against the risks of delaying surgery >24-48 hours after multidisciplinary discussion. The risk of surgical bleeding in patients undergoing percutaneous coronary interventions for which dual antiplatelet therapy will be required has to be considered in acute ischaemia.
Although unfavourable event rates seem to be higher in patients undergoing hip fracture repair when aortic stenosis is left untreated, when time-sensitive, high-risk/intermediate-risk non-cardiac surgery is required in the presence of a low-risk valve procedure, the Heart Team is recommended for evaluation of the valve replacement [7,8]. In a systematic review of 16 studies involving 25,349 patients, delaying surgery for >48 hours was associated with increased mortality, whereas accelerated (median 6 hours) as compared to standard care (24 hours) surgical timing did not show any difference in short-term mortality or incidence of complications [9,10].
Evaluation of frailty
Frailty is a condition characterised by reduced functional reserves and increase vulnerability to stressors (11). The ESC consensus document on frailty in cardiology advises that patients ≥70 years be screened and assessed for frailty as well as for any acute or chronic cardiovascular disease [11]. When an acute stressor such as an interventional procedure or surgery is performed in patients, the clinical outcomes are worse in vulnerable patients than in robust patients. Sarcopenia and osteosarcopenia – reduced muscle and bone mass and reduced quality of the same – are key aspects of frailty and, of course, are closely related to impaired mobility, falls, fractures, and disability, as well as perioperative and post-discharge orthopaedic problems.
Various tests are used to screen and assess the various domains (i.e. medical, physical, cognitive, and social domains), of frailty alone or that include a multidimensional evaluation. The evaluation of the physical response is relevant. Several tests in this domain, such as tests that require walking or rising from a chair, are not feasible for patients with hip fractures. Advised alternatives are handgrip strength, measured using a portable dynamometer, muscle mass, evaluated with imaging (computed tomography), and the patient’s self-reported status of disability and vitality (i.e. the Clinical Frailty Scale) [7]. Other tools may be used to assess cognitive function, social support, and nutrition status.
“De-frailing”, which includes multifaceted interventions through reinforced action on physical weakness, cognitive impairment, anaemia and malnutrition, was reported to be achievable in frail older adults during short-term hospitalisations for acute cardiovascular diseases [12]. Therefore, a multicomponent intervention, early mobilisation, and rehabilitation or prehabilitation (when feasible) is advised in older patients who have undergone surgery [7,11].
Evaluation of the risk of major geriatric complications that may jeopardise clinical outcomes (post-operative delirium)
Delirium is characterised by an acute and fluctuating course, inattention, altered levels of consciousness, and evidence of disorganised thinking [13]. Delirium is the most common complication in patients with hip fractures, occurring in 28 to 50% of patients [14]. Many conditions, including advanced age, cognitive impairment or dementia, functional (physical, vision, hearing, or frailty) impairment, cardiovascular disease, cumulative comorbidities, and central nervous system disorders, as well as precipitating factors such as major surgery, systemic illness or organ dysfunction, metabolic abnormalities, and drugs have been associated with delirium [15].
Assessing physical performance, in addition to cognitive function, can help identify high-risk patients for delirium [16]. The focus on delirium should be aimed at avoiding or contrasting the conditions that favour the onset of delirium (see below and Table 2 for patients/caregivers’ perspective).
Table 2. Avoid conditions associated with risk of delirium.
-
- Encouraging an appropriate environment, reduce acoustic noise when visiting, especially at bedtime and at night.
- Help setting up an appropriate care setting, with environmental aids (calendar, clock).
- Help providing aids for sensory impairment when needed (glasses, acoustic aids).
- Help being involved as family members and/or caregivers by supporting cognitive aspects.
Post-operative phase
As a caregiver, soon after discharge of the patient from hospital:
-
- Support the rehabilitation programme.
- Encourage movement to avoid sarcopenia.
- Provide an adequate environment at home (no carpets, avoid stairs when possible, provide logistical tools, e.g. in the bathroom, to help the patient get up using the strength of his arms).
- Provide appropriate shoes.
- Intensify support during the first weeks after discharge (provide meals, providing walking assistance at home if the patient is able to move).
- Focus on diseases and conditions that can determine new falls (orthostatic hypotension, arrhythmias, ensure adequate hydration and nutrients…) highlighting to the patient the importance of paying attention to potential related symptoms.
- Consider digital health technology.
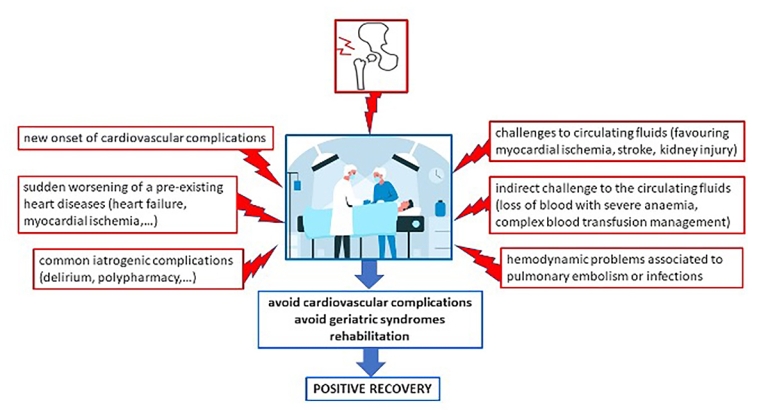
It is advised to consider the following points in the acute operative phase and the early postoperative period:
- Several challenges may jeopardise the cardiovascular system during the acute operative period, particularly in older and vulnerable patients, who have undergone hip surgery (Figure 2), including:
- new onset of cardiovascular complications
- sudden worsening of a pre-existing heart disease (heart failure, myocardial ischaemia, etc…)
- challenges to circulating fluids (favouring myocardial ischaemia, stroke, kidney injury, etc…)
- indirect challenge to the circulating fluids due to various factors (relevant loss of blood with severe anaemia, complex blood transfusion management)
- haemodynamic problems associated to pulmonary embolism or infections
- common iatrogenic complications due to polypharmacy
Beyond haemodynamic concerns, anaesthesia must be individualised based on patient characteristics, avoiding a prolongation of the operating period, with careful dosing of drugs to reduce the risk of postoperative delirium. Some of the most effective strategies in the early diagnosis and management of delirium are screening on a daily schedule, extending the visitation periods by relatives and friends, and a multicomponent intervention. The latter includes the monitoring of vital and laboratory parameters, focusing on the hydration/oxygenation of the patient, immobilisation, bladder catheters, bowel function, sleep, pain control, the creation of an appropriate environment with reduced acoustic noise, especially at bedtime and at night, and environmental aids (calendar, clock). This approach has been shown to reduce the incidence of delirium by 40% compared to standard care [17].
The major concerns during perioperative care are the management of thromboembolic therapies that pre-date the fall and surgery, the risk of thromboembolism and the management of cardiovascular thromboembolic complications of surgery. The recently published 2025 consensus document on hip surgery, the 2022 ESC Guidelines on non-cardiac surgery, and the 2019 ESC Guidelines on pulmonary embolism [7,8,18] deal with these in greater detail. In particular, according to the consensus on hip surgery [7], it is advised to avoid unnecessary delay for time-sensitive hip surgery and any ongoing treatments with antiplatelet agents should not delay surgery. It is advised to delay elective hip surgery to 1 month after elective percutaneous coronary intervention and 3 months after an acute coronary syndrome to safely interrupt P2Y12 inhibitor treatment. It is advised to continue perioperative single antiplatelet therapy in patients with prior percutaneous coronary intervention without excessive perioperative bleeding risk. Interruption of Non–vitamin K antagonist oral anticoagulants (NOAC) treatment depends on NOAC type and renal function according to general guidelines. Interdisciplinary judgement about perioperative interruption and post-operative continuation of antithrombotic therapy in patients at high risk of bleeding and/or high risk for thrombotic events should be shared between surgeons and cardiologists. Thromboprophylaxis with NOACs or low-molecular-weight heparin is advised, according to risk up to 35 days, and careful prescription of post-operative venous thromboembolism prophylaxis, as early as possible, post-operative mobilisation and a short hospitalisation are considered essential in limiting the risk.
Restoring mobility and independence to the basic functions of daily life and treating the complications and medical problems that may occur after surgery are the main objectives of a structured rehabilitation intervention. These are essential steps to achieving positive results after the difficult period of hip fracture and subsequent surgery. Individualised plans for rehabilitation may be executed in a residential and/or ambulatory setting. Both cardiovascular disease and frailty may influence expected goals and measured outcomes and should be considered in a modern rehabilitation programme after hip surgery. After discharge, both caregivers and patients should be alert to and participate in avoiding orthostatic hypotension which can lead to new falls. The possible occurrence of, or the worsening of symptoms related to atrial fibrillation and heart failure decompensation must be promptly recognised. The general management of frailty is particularly relevant in the early period after discharge [7]. This is based mainly on nutrition, physical exercise, and cognitive and emotional support. Moreover, the suggested points that need to be considered in the general management of frailty are particularly relevant after hip surgery. These are: a cardiac rehabilitation multicomponent programme, a focus on environmental aspects to reduce falls (such as avoiding architectonic barriers at home, carpets, etc), a review of potentially inappropriate polypharmacy and a reduction in hospitalisation periods when needed. Self-care should be encouraged (but intensified through external support when needed, such as after an acute event or in the case sensory impairment) and actions at a community level should be taken if the individual or family level of support is inadequate. The help of potential new interventions from eHealth technologies can be incorporated as well. Increased support in the weeks after returning home may allow the patients to achieve a better and more stable recovery.
Patient/caregivers-oriented message
Patients and caregivers should be involved in the pathway towards recovery. The objective is to reach the same level of independence the patients had before their fall and hip surgery, ideally within a few weeks after discharge (Table 2). This can be obtained by avoiding geriatric and cardiovascular complications during the peri-acute phase of the hospital stay and the optimisation of post-operative care.
Conclusions
Prevention and proper management of cardiovascular complications in the pre-operative and post-operative period, together with careful support of specific geriatric needs and frailty, can promote a positive outcome of older patients after hip surgery.