Cardiac rehabilitations
Cardiac rehabilitation programs (CR) are currently gaining popularity; their emphasis is on improving long-term outcomes and quality of life for patients with a history of ACS. Secondary prevention is most effectively provided through cardiac rehabilitation. CR programmes are no longer limited to the prescription of physical exercise but also include lifestyle changes, risk factor management, psychosocial care, and dynamic evaluations.
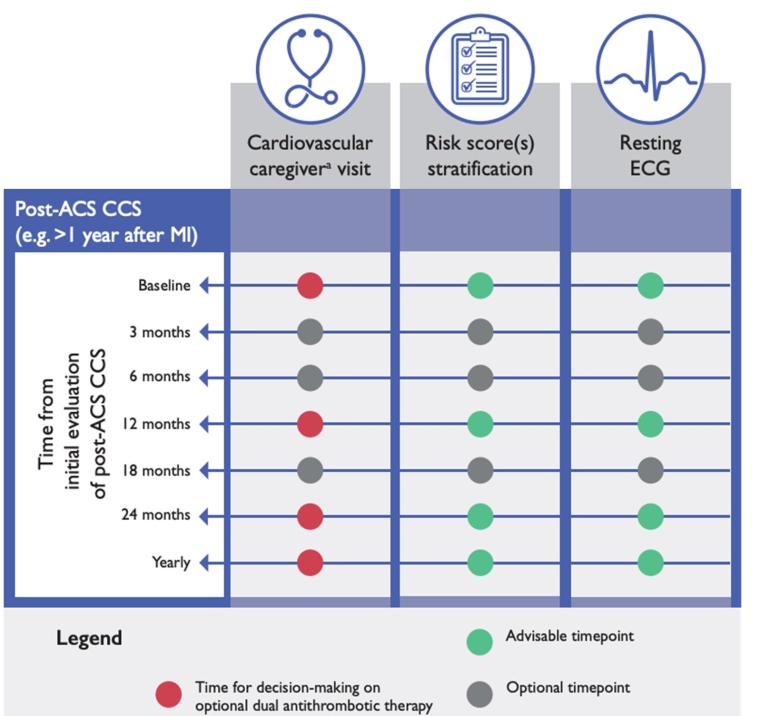
All ACS patients should participate in a comprehensive CR program, which should start as early as possible after the index ACS event [5]. CR may be performed in in-patient or outpatient settings, and take into account age, frailty, results of prognostic risk stratification, and comorbidities. In this program, the patient’s adherence to and persistence in treatment should be assessed. It is important to recognise that adherence has complex underlying psychological drivers, and therefore a whole-systems approach is mandatory.
Despite proven benefits [6], the rates of referral to, participation in, and implementation of CR programs are low [7].
Many patients adopt healthier lifestyles during CR but relapse to premorbid habits when returning to everyday life. Telerehabilitation may be an effective strategy to maintain a healthy lifestyle over time and can support or even partially replace conventional, centre-based CR. Telerehabilitation means rehabilitation from a distance, covering all CR core components, including telecoaching, social interaction, telemonitoring, and e-learning. Therefore, more research on the impact of telerehabilitation on outcomes is still needed, as are investigations into health and digital literacy in CR.
In addition to alternatives to CR, there is also a need for stronger endorsement of CR by physicians, cardiologists, and healthcare professionals [8]. It is also important to initiate and establish a strong partnership between patients and healthcare professionals as early as possible [8].
Lifestyle management
Lifestyle management is one of the cornerstones of comprehensive CR. Studies in secondary prevention settings indicate beneficial effects on prognoses [7]. Implementing healthy lifestyle behaviours decreases the risk of subsequent cardiovascular events and mortality and is an excellent and essential addition to secondary prevention therapy.
Resuming prior activities, including returning to work, engaging in personal and social activities, driving and travelling are important components of recovery after ACS. Offering adequate psychosocial and vocational support as required is an important part of comprehensive cardiac rehabilitation [9].
Treating risk factors is essential [9]:
- Tobacco abstinence is associated with a reduced risk of re-infarction (30–40%) and death (35–45%) after an ACS. Measures to promote cessation of smoking are therefore a priority after an ACS.
- A healthy diet and eating habits influence cardiovascular (CV) risk. Adopting a Mediterranean-style diet can help reduce CV risk in all individuals, including persons at high CV risk and patients with atherosclerotic cardiovascular disease (ASCVD).
- It is recommended to restrict alcohol consumption to a maximum of 100 ml per week (same limit for men and women)
- General physical activity recommendations include a combination of regular aerobic physical activity and resistance exercise throughout the week, which also forms the basis of recommendations for patients post-ACS. However, it is important to recognise that this daily physical activity does not replace participation in exercise-based CR.
- It is recommended that all patients have their mental well-being assessed using validated tools before discharge, with consideration of onward psychological referral when appropriate.
Impact on practice
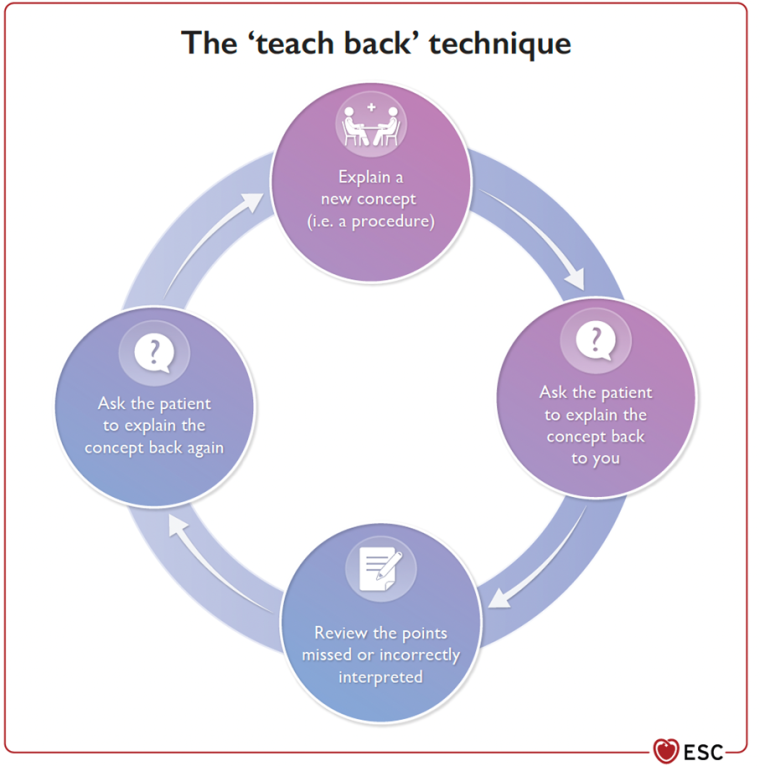
Rehabilitation is the cornerstone of secondary prevention after an ACS. Patient-centred care is essential and should be provided through therapeutic education rather than just patient information.