Key words
athletes, risk, sports, sudden cardiac death
Abbreviations
ACM: arrhythmogenic cardiomyopathy
AHA: American Heart Association
ARVC: arrhythmogenic right ventricular cardiomyopathy
CPVT: catecholaminergic polymorphic ventricular tachycardia
CRY: cardiac risk in the young
DCM: dilated cardiomyopathy
ERP: emergency response plan
HCM: hypertrophic cardiomyopathy
LQTS: long QT syndrome
SCD: sudden cardiac death
Impact on practice statement
Sudden cardiac death represents one of the most feared events in sports cardiology and may occur in athletes of all ages. Understanding the conditions which predispose athletes to SCD enables appropriate risk stratification and primary prevention. Adequate assessment of an athlete’s risk is not as straightforward as in non-athletic individuals and warrants additional consideration, as exercise can cause diagnostic challenges and further modulate the risk. We present insights from a quaternary care centre specialised in sports cardiology and inherited cardiac conditions.
Take-home messages
- Exercise-related cardiac events are commonly the result of quiescent cardiac conditions.
- Risk stratification in athletes is a multilayered process that requires a structured approach. It starts with accurate diagnosis of the primary underlying cardiac condition and is further refined by exercise.
- Risk appears to vary based on the athlete’s demographics and the sports discipline. Male sex, adolescent age and high-intensity interval sport may confer a higher risk.
- Clinicians should assess the risk in athletes based on objective findings and available literature. They should practice moderation when conveying this risk to the individual and be mindful of the athlete’s preferences.
- The discussion which ensues after risk stratification is nuanced, as there may be a number of different stakeholders involved who may influence the athlete’s decision to continue or not with participation in competitive sport.
Introduction
Exercise is beneficial in reducing overall mortality, cardiovascular risk, and the risk of developing various medical conditions. Moderate intensity physical activity is encouraged in all individuals, and at least to a certain point, it seems that at population level the relation between the amount of exercise and risk reduction for overall and cardiovascular mortality is linear [1]. However, vigorous and sustained exercise can sometimes lead to major cardiac events, predominantly in the context of pre-existing, often undiagnosed, heart disease. Premature death due to cardiac causes seems more prevalent in athletes, which is paradoxical, considering their outstanding physical condition [2]. Identifying individuals at risk for sudden cardiac arrest, diagnosing an underlying cardiac condition which might be worsened by strenuous exercise and preventing a tragic event from unfolding are some of the core principles of sports cardiology. For athletes to pursue their professional career safely, risk stratification is much needed. In some cases, in accordance with guidelines and existing data, discouraging competitive sports might be reasonable or even necessary for the safety of the individual. Nevertheless, exercise prescription in individuals with an established cardiac diagnosis is progressively becoming more liberal, as individuals may now participate in competitive sports after expert assessment, in the context of a shared decision-making model [3].
Causes of sudden cardiac death in athletes
Broadly speaking, the conditions that predispose athletes to sudden cardiac death can be separated into inherited, congenital or acquired conditions. Inherited and congenital conditions account for most of the events in the younger (≤35 years) age group, while acquired conditions, and, in particular, coronary atherosclerosis, predominates in older (>35 years) individuals [2]. Conditions represented in sudden cardiac death registries include cardiomyopathies such as hypertrophic cardiomyopathy (HCM), arrhythmogenic cardiomyopathy (ACM) and less frequently dilated cardiomyopathy (DCM), ion-channelopathies such as long QT syndrome (LQTS) and catecholaminergic polymorphic ventricular tachycardia (CPVT), accessory pathways (Wolf-Parkinson-White), aortopathies, valvular disease, coronary artery anomalies, atherosclerotic coronary artery disease and myocarditis [4].
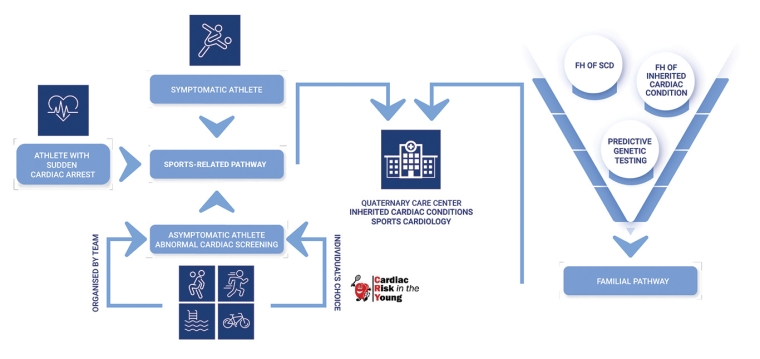
How athletes may come to our attention (entry points)
Athletic individuals often come to the attention of a cardiologist for the suspicion of an underlying cardiomyopathy, channelopathy or aortopathy. This can occur in a variety of clinical scenarios, which differ in terms of approach to diagnosis and management. Moreover, making the distinction between a potentially early clinical phenotype of a hereditary cardiac condition and a sports-induced adaptation can be challenging and demands extensive knowledge and experience. The sustained elevation of cardiac pressure and volume loads associated with regular exercise promote a series of electrical, structural and functional adaptations, collectively termed “athlete’s heart”. The nature, or magnitude of change varies by sporting discipline, ethnicity, age and sex and can overlap with mild phenotypes of conditions associated with arrhythmias and SCD. This scenario can be even more challenging in individuals over 35 years of age, where athletic adaptations, acquired cardiovascular diseases and inherited cardiac conditions or cardiac congenital abnormalities may overlap, further complicating the clinical presentation.
Common entry points for athletes and athletic individuals include:
- Athletes can present with concerning symptoms, such as exertional dyspnoea, chest pain, palpitations or syncope. Syncope, particularly when it coincides with effort, is the most concerning symptom, as it is highly likely to signal a malignant cardiac condition. In rare instances, athletes may be referred after they experienced a sudden cardiac arrest. However, symptoms may be masked and the athlete may report only a reduced exercise tolerance, which translates into the inability to perform in their physical activity as well as they used to. Importantly, this might not be reported only by the athlete, but by fellow members of their teams or the team coach. Athletes possess a considerable degree of physical fitness which translates to considerable reserves. Therefore, symptoms due to an underlying cardiac condition may occur late and may be more subtle compared to more sedentary patients.
- Request for further evaluation after attending a cardiac screening session commonly organised in the context of participating in competitive sport. In most countries there are no nationally implemented cardiac screening programmes and screening is organised by respective teams, sporting governing bodies or charitable organisations. Notable exceptions include Italy, the United States of America, Israel and Japan where national screening programmes are in place. Most screening programmes include history, commonly in the form of a questionnaire, physical examination and a resting 12-lead ECG. Athletes may be referred for further evaluation due to the presence of previous symptoms that cause concern, a family history suggestive of an inherited cardiac condition or due to an abnormal ECG, as per the international criteria for electrocardiographic interpretation in athletes consensus statement [5].
- Another scenario involving asymptomatic individuals may arise when further assessment is required after a 1st degree relative (index case or proband) has been diagnosed with an inherited cardiac condition or experiences sudden cardiac arrest or death. This is not specific to athletes, nor it is related to their sports activity. The diagnostic approach may differ slightly for athletes, as the sports-induced adaptations may resemble the phenotype of the condition under investigation. In situations in which the index case also harbours a pathogenic or likely-pathogenic genetic variant, predictive testing can be offered to the athlete, after genetic counselling in an experienced cardiogenetic clinic. Genetic counselling in such instances may be more challenging and requires additional expertise, as the result may impact the athlete’s career, even if they do not display the phenotype [6].
Figure 1. Entry points for athletes requiring cardiac evaluation and risk stratification.
FH: family history; SCD: sudden cardiac death
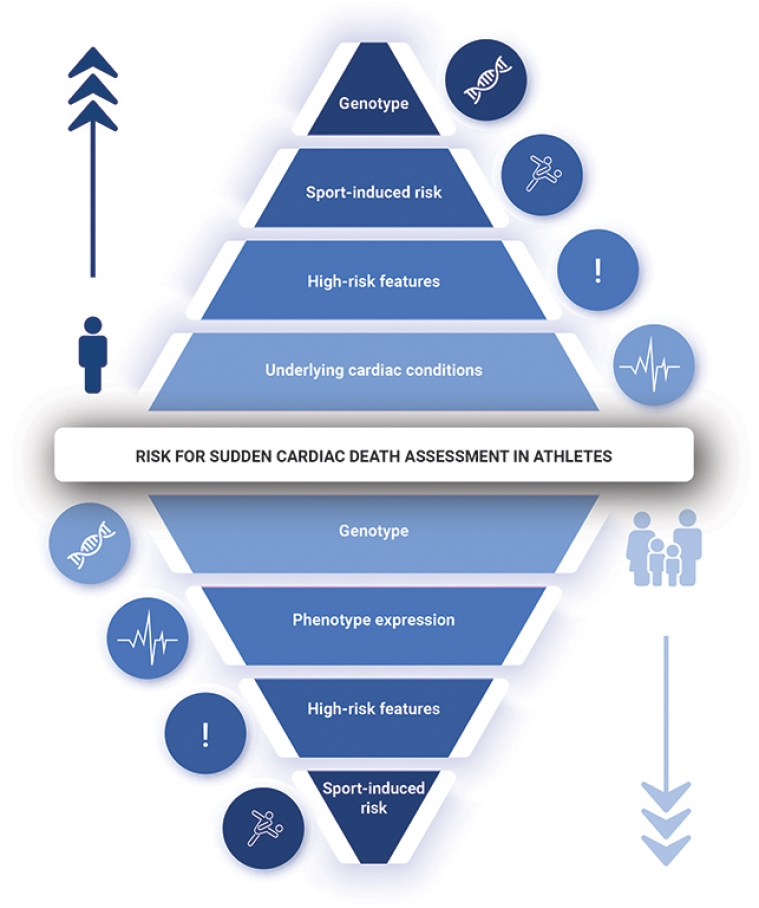
Principles for assessing an athlete’s risk
The general principles for assessing an athlete’s risk are very similar to those for the general population but one has to account for the effect of exercise. Moreover, the initial approach depends on what prompted the athlete’s referral (Figure 2). Central to risk assessment lies the confirmation of a diagnosis of a cardiac condition. As a general rule, the clinical phenotype, including the presence of symptoms, remains paramount to risk stratification in athletes. It is important, however, to understand the pitfalls and limitations of the investigations employed and the diagnostic criteria utilised. Caution should be exercised when labelling athletes with a condition, particularly when the phenotype falls within a grey area, where it is difficult to differentiate between athletic adaptation or an early phenotype of a disease. In these cases, close surveillance at regular intervals and dynamic risk assessment may be warranted.
Genetic testing may contribute to the diagnosis and risk assessment of athletes. Particular genotypes, such as DSP, TMEM43, LMNA or FLNC, which are associated with ACM, have a propensity for high arrhythmic risk that can pre-date the structural abnormalities and may be exacerbated by high volume and intensity of exercise. Similarly, in certain channelopathies such as CPVT and LQTS, risk assessment and exercise prescription is influenced by the genotype. Contrarily, in conditions such as HCM and Brugada syndrome, risk assessment relies mostly on phenotype expression and identifying high-risk features [6].
Figure 2. Risk for sudden cardiac assessment in athletes. The approach differs depending on the clinical scenario. The individual, sports-related, approach is shown in the upper part of the picture, while the familial pathway is pictured in the lower part of the picture.
Determinants of risk
As there are no dedicated risk score calculators for predicting SCD in athletes, formal risk assessment relies on the guideline-enforced risk score calculators for the underlying cardiac condition. When translating the results to athletes, caution should be exercised. Firstly, the risk score calculators for various cardiomyopathies, such as the European Society of Cardiology HCM Risk-SCD, the American Heart Association HCM SCD Calculator, the 2019 Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) Risk Calculator, and the LMNA-risk ventricular tachyarrhythmias calculator, did not include elite or competitive athletes in the study population. Hence, the risk might be underestimated in athletes. Reassuringly, however, when the performance of the ARVC Risk Calculator was evaluated in a cohort of 176 athletes, the study concluded that athletic status at diagnosis did not appear to have incremental prognostic value over the risk calculator and that the ARVC Risk Calculator can be used accurately in athletic patients [7]. It also appears that the risk is not homogeneous in athletes. Several factors, such as sex, age, ethnicity or type of sport can alter the risk for SCD beyond the perceived risk of the underlying condition [2]. SCD has been reported more frequently in young, male, black, basketball players in the United States, while football appears to lead in sports-related SCD in Europe [2]. Even though these observations might be reflective of the popularity of the sporting disciplines in various countries, it highlights that sports that are based on high-intensity interval exercise, also known as stop-and-go sports, may confer a higher risk for major cardiac events. Regardless of the type of physical activity, sustained and vigorous exercise might precipitate ventricular arrhythmias in the context of dehydration, electrolyte imbalance and hyperthermia.
Table 1. Features during an athlete’s evaluation that may indicate elevated risk.
| Investigation | Feature that may modify risk depending on underlying condition |
|---|---|
| Family history | Sudden premature death (<40 years), including unexplained drownings, road traffic accidents, epileptic seizures Aortic dissection |
| Symptoms | Unheralded syncope Exertional chest pain |
| ECG | Excessive QT prolongation; QTc ≥500 ms Conduction tissue disease Multifocal/Polymorphic ventricular ectopy |
| Exercise tolerance test / CPET | Exercise-induced symptoms Abnormal haemodynamic response to exercise ST-segment elevation/depression Paradoxical QT prolongation with effort Exercise-induced complex arrhythmia (Polymorphic/multifocal premature ventricular contractions, non-sustained or sustained ventricular tachycardia) |
| 24h Holter ECG tape | Complex arrhythmia (Polymorphic/multifocal premature ventricular contractions, non-sustained or sustained ventricular tachycardia) High grade or complete AV block |
| Echocardiography | Degree of wall thickness LV outflow tract obstruction Degree of cardiac chamber dilatation Degree of systolic impairment LV/RV regional wall motion abnormalities Mitral valve prolapse, mitral annular disjunction Degree of ascending aorta dilatation Excessive atrial dilatation |
| CMR | Presence and volume of late gadolinium enhancement indicative of fibrosis Presence of myocardial inflammation |
| Genetic test | Certain genotypes might pose a significant risk or interfere with the athlete’s activity even in carriers (genotype positive, phenotype negative): Channelopathies: RYR2, KCNQ1, KCNH2 Cardiomyopathies: DSP, PKP2, JUP, DSG, TMEM43, LMNA, FLNC |
AV: atrioventricular; CMR: cardiovascular magnetic resonance; CPET: cardiopulmonary exercise testing; ECG: electrocardiogram; LV: left ventricular; RV: right ventricular
Risk mitigating strategies
Risk mitigating strategies can be enforced for both primary prevention, as well as secondary prevention. It is beyond our aim to describe the medical and device strategies already established by guidelines for the prevention of SCD. There are several risk mitigating strategies in athletes which encompass different action levels:
- General considerations: the impact of dehydration and electrolyte imbalance should be always accounted for. Athletes should be educated to replenish their electrolytes while exercising by using sports drinks or electrolyte effervescent tablets. Exercising in particularly hot environments increases the risk for hyperthermia, particularly for non-acclimatised athletes.
- Establishing a “safe zone”. It is advisable to perform exercise tests with protocols tailored to the athlete’s training regime, as athletes might reach heart rates exceeding 85% of their maximum predicted heart rate while training. Functional tests should aim for higher thresholds in athletes to adequately assess the arrhythmia burden. Furthermore, athletes should do a training session while fitted with an ECG monitor. Depending on the results, athletes might be advised to restrain their exercise in order to not exceed a certain heart rate beyond which ventricular arrhythmias occur more frequently.
- Creating a safer environment for the athlete at risk. Even for athletes deemed at low risk, it is advisable to prepare them and their team for the “worst case scenario” in which sudden cardiac arrest occurs. Teammates, coaches and staff should know about the athlete’s condition, be aware of how a sudden cardiac arrest may manifest and be trained in CPR. A documented emergency response plan (ERP) should be in place incorporating the use of an automated external defibrillator (AED). Sometimes, athletes may train on their own or in remote locations. It is advisable that individuals at risk be accompanied by someone or share their real-time location with a person they trust and who can act accordingly in case of an event. In exceptional cases, wearable defibrillator vests can be offered.
- One important aspect which should be discussed with the athlete, whether in primary or secondary prevention, is that device therapy should not be understood as a risk mitigating strategy in itself, as it does not affect the course of the disease. Device therapy can be lifesaving for individuals at high or very high risk, but if high-intensity exercise is a trigger for malignant ventricular arrhythmias, such as in CPVT, LQT or ACM, then it is necessary to refrain from competitive sports.
Patient-oriented message
The risk of SCD in athletes usually relates to an underlying heart disease that the athlete may be born with or acquire during their career. It can be hard to quantify, as evidence is fairly limited, and it is therefore important that athletes with heart disease are assessed in centres with expertise in sports cardiology. Although we have tools which we can use to quantify the risk in different conditions, these tools may underestimate the risk in the context of competitive sport. Even athletes deemed at low risk have a risk which may exceed that of the general population. Hence, the decision relating to participation in competitive sport should include an honest discussion with the athlete and include all mitigating measures to reduce the risk, including an ERP.
Conclusion
Risk stratification in athletes with established or suspected heart disease is a complex process that requires the amalgamation of several factors including the risk of the underlying heart disease based on comprehensive clinical and genetic evaluation, the athlete’s demographics and the sporting discipline. Decisions about participation in sport should incorporate all possible mitigating measures and an honest discussion with the athlete in the context of a shared decision model.