Take-home messages
- Inclisiran is a twice-yearly injection inhibiting PCSK9 with similar potency compared to evolocumab/alirocumab. Improved compliance is the major benefit compared to actual biweekly treatment.
- Bempedoic acid is the first oral non-statin related drug, reducing LDL and acting via a pathway that does not provoke myalgia.
- Omega-3/EPA are used in patients with high TGs (although their benefits are independent of TG reduction) and have shown benefit in reducing cardiovascular hard endpoints, including cardiovascular death.
Keywords
new drugs, statin myalgia, compliance issues, non-LDL lowering hypolipidaemic treatment
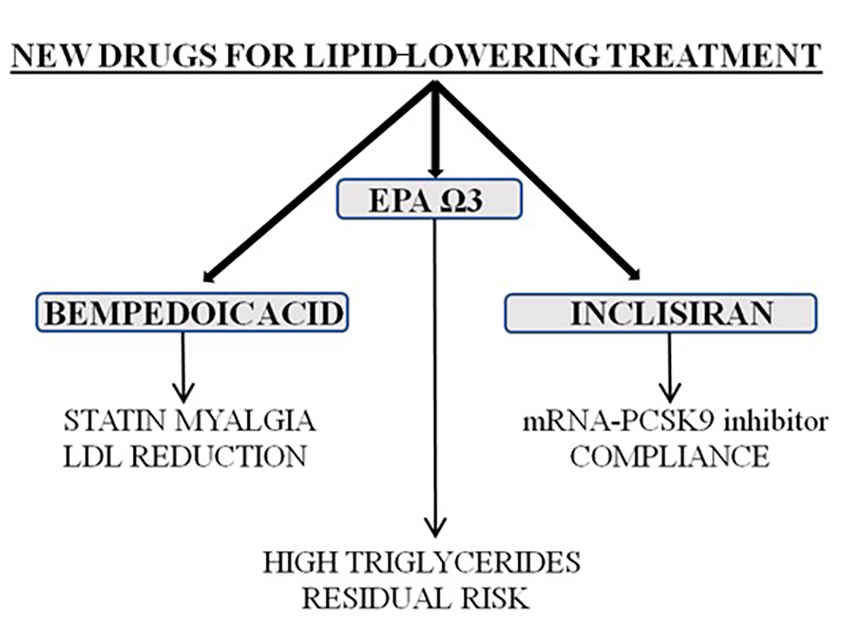
Figure 1. New lipid-lowering treatments.
EPA: eicosapentaenoic acid; LDL: low-density lipoprotein; mRNA: messenger ribonucleic acid; Ω3: omega-3; PCSK9: proprotein convertase subtilisin/kexin type 9.
Introduction
Guidelines over the last decades have tended to agree that a crucial point in hypolipidaemic treatment is the significant reduction of low-density lipoproteins-cholesterol (LDL-C). Although our pharmaceutical armamentarium is very good at the moment (the combination of statin-ezetimibe-proprotein convertase subtilisin/kexin type 9 [PCSK9] can reduce LDL cholesterol [LDL-C] levels by 85%), new drugs are emerging through the different pitfalls of current drugs.
Inclisiran
With the broad availability of statins and ezetimibe in generic form, and proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors being prescribed more often with fewer barriers in the majority of European health systems, the real “Achilles’ heel” of lipid-lowering therapy is compliance. A significant portion of patients dislike taking drugs, and all epidemiological studies show that, for every pill that we add to a patient’s treatment, compliance diminishes significantly. The combination in a single pill of simvastatin or atorvastatin or rosuvastatin with ezetimibe was of significant help to this recurrent problem. The administration of PCSK9 inhibitors, e.g., alirocumab/evolocumab every two weeks, is still a problem in this respect. The introduction of inclisiran is a significant step in improving compliance, especially if the VICTORION-2 PREVENT study provides positive results.
Inclisiran is the first-in-class of PCSK9 inhibitors, and is a double-stranded, small interfering ribonucleic acid (siRNA) therapy for lowering LDL-C. It mimics the body's natural silencing mechanism of gene expression (ribonucleic acid [RNA] interference), cleaving the messenger RNA (mRNA), encoding the protein PCSK9, increasing the number of LDL-C receptors on the hepatocyte surface, and thus increasing LDL-C clearance from the circulation.
Inclisiran is conjugated to the ligand triantennary N-acetylgalactosamine carbohydrates (GalNAc) for liver-targeted action and binds specifically to asialoglycoprotein receptors (ASGPRs), which are highly expressed on hepatocytes, resulting in rapid endocytosis. After endocytosis, inclisiran is slowly released from the endosome into the hepatocyte cytoplasm and then binds to an RNA-induced silencing complex (RISC), activating the body's natural method of RNA interference, which regulates the production of the PCSK9 protein. The siRNA (i.e., inclisiran)-RISC complex catalytically cleaves and degrades many copies of the PCSK9 protein mRNA, thereby preventing its expression and allowing more LDL-C receptors to remain on the hepatocyte surface in order to remove excess circulating LDL-C. [1,2,3].
Inclisiran has been evaluated in three pivotal, randomised, double-blind phase 3 studies, ORION-9, ORION-10, and ORION-11, in a total of 3,660 randomised participants. ORION-9 enrolled patients with clinical or genetic evidence of heterozygous familial hypercholesterolaemia (HeFH) and LDL-C ≥100 mg/dL, while ORION-10 and ORION-11 enrolled patients with atherosclerotic cardiovascular disease (ASCVD) and LDL-C ≥70 mg/dL. Additionally, the ORION-11 study also included patients with an ASCVD risk equivalent (type 2 diabetes, HeFH, or a 10-year risk of a cardiovascular event of ≥20% as assessed by the Framingham Risk Score for cardiovascular disease [CVD] or equivalent) and LDL-C ≥100 mg/dL.
The results of these studies confirm that twice-yearly dosing with inclisiran achieves marked and sustained LDL-C reduction of up to 52% compared with placebo in patients with elevated LDL-C, despite maximally tolerated statin therapy (with or without additional lipid-lowering therapy). In addition, it was reported to be well tolerated, with a safety profile shown to be comparable to placebo, except for mild and transient injection site reactions [4,5].
Recently, long-term inclisiran data from the ORION-8 phase 3 open-label extension trial were also announced, demonstrating consistent efficacy, safety and tolerability beyond 6 years, in patients with high cardiovascular risk and elevated LDL-C [5].
The effect of inclisiran in cardiovascular (CV) risk reduction is being evaluated in two dedicated ongoing CV outcomes trials: ORION-4 and VICTORION-2 PREVENT.
VICTORION-2 PREVENT is a phase 3 clinical trial which will include 15,000 patients with established CVD who will receive inclisiran 300 mg versus placebo and will be followed up for 6 years. This study will evaluate not only the effects of inclisiran on lipid parameters but also the occurrence of major adverse cardiovascular events (major adverse cardiac events [MACE]; i.e., non-fatal myocardial infarction [MI), non-fatal stroke, CV death, urgent coronary revascularisation), as well as all-cause death.
The ORION-4 trial aims at evaluating the 5-year occurrence of MACE in approximately 15,000 participants with pre-existing ASCVD, randomised to either inclisiran sodium 300 mg (every 180 days) or matching placebo. The primary endpoint of this phase 3 trial includes coronary heart disease (CHD) death, myocardial infarction (MI), fatal or non-fatal ischaemic stroke and an urgent coronary revascularisation procedure, whereas the composites of CHD death, MI or CV death represent secondary outcomes [4].
In summary, inclisiran has been shown to act selectively on hepatocytes and at a very early stage, which provides a great efficacy profile with stable and sustained reduction of excess circulating LDL-C and an equally good safety profile with only 2 doses per year [6].
Bempolic acid
Bempedoic acid comes as a solution for patients who have statin intolerance and barriers to the prescription of PCSK9 inhibitors.
Bempedoic acid (8-hydroxy-2,2,14,14-tetramethylpentadecanedioic acid; ETC-1002; Esperion Therapeutics, Ann Arbor, MI, USA) is a first-in-class small molecule inhibitor of ATP citrate lyase (ACLY), a key enzyme that supplies a substrate for cholesterol and fatty acid synthesis. ACLY is essential for growth and development, such that homozygous knockout (Acly−) in mice is embryonically lethal, indicating non-redundancy during development. By inhibiting ACLY, bempedoic acid induces LDL receptor upregulation and stimulates the uptake of LDL particles by the liver, which contributes to the reduction of LDL-C concentration in the blood.
Bempedoic acid, administered orally once a day, is quickly absorbed in the small intestine, and has a half-life ranging from 15 to 24 hours. It is a prodrug that is activated by very long-chain acyl-CoA synthetase 1, an enzyme that is synthesised only in the liver. Even though bempedoic acid acts on the same pathway as statins (3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors), the lack of the activating enzyme in skeletal muscle may prevent the muscular adverse effects associated with statins. For this reason, bempedoic acid may represent a novel treatment to reach LDL-C goals for statin-intolerant patients |7].
A number of phase 2 and phase 3 randomised controlled trials (RCTs) are already available, showing encouraging effects of bempedoic acid treatment on LDL-C.
Bempedoic acid is currently available in the majority of European countries, either as monotherapy or in combination with ezetimibe.
A systematic review and meta-analysis of bempedoic acid, which included 10 randomised clinical trials (n=3,788 patients) comprising 26 arms (active arm [n=2,460]; control arm [n=1,328]), confirmed that bempedoic acid significantly reduced total cholesterol (by 15%), non-high-density lipoprotein cholesterol (by 18.2%), LDL-C (by 22.9%), low-density lipoprotein particle numbers (by 20.7%), apolipoprotein B (by 15.2%), and high-sensitivity C-reactive protein (hsCRP; by 27%), while negatively affecting serum levels of high-density lipoprotein (HDL) cholesterol (−5.8%) and HDL particle numbers (−3.2%) [7].
The CLEAR Outcomes trial [8-10] showed that bempedoic acid improves long-term CV outcomes and effectively reduces LDL-C compared with placebo among patients who have either established ASCVD or are at high risk for it, and who are intolerant to statin therapy.
The goal of the trial was to compare the safety and efficacy of bempedoic acid compared with placebo among patients with or at high risk for CVD and who were intolerant of statin therapy.
Patients were randomised in a 1:1 fashion to either bempedoic acid 180 mg (n=6,992) or placebo (n=6,978) once daily. All patients were statin intolerant. Patients who were receiving a very low average daily statin dose without unacceptable adverse effects could be enrolled. Other lipid-lowering therapies were permitted, including PCSK9 inhibitors administered as monotherapy or in combination. 70% of patients were on secondary prevention and the mean baseline LDL-C was 139 mg/dL.
Principal findings
After a follow up of 40.6 months, the primary outcome, 4-component MACE (non-fatal MI, non-fatal stroke, coronary revascularisation, or CV death) for bempedoic acid compared with placebo was 11.7% vs 13.3%, hazard ratio (HR) 0.87, 95% confidence interval (CI): 0.79-0.96; p=0.004).
The secondary outcomes for bempedoic acid compared with placebo demonstrate a reduction in the 3-component MACE (non-fatal MI, non-fatal stroke, CV death): 8.2% vs 9.5% (p=0.006) of fatal or non-fatal MI (p=0.002) and coronary revascularisation (p=0.001). No muscular disorder was noted (15.0% vs 15.4%) although a significant increase of hyperuricaemia, gout and cholelithiasis were reported. There were no changes in haemoglobin (Hb)A1c or glucose levels with bempedoic acid in those without diabetes at baseline.
The results of this trial indicate that bempedoic acid improves long-term CV outcomes and effectively reduces LDL-C compared with placebo among patients who have either established ASCVD or are at high risk for it, and who are intolerant to statin therapy. These are very promising findings and extend our current armamentarium of lipid-lowering therapies [11].
EPA
Although LDL-C continues to be the primary target, and the majority of drugs aim to reduce it, the last years have seen the revival of omega-3 in the form of pure eicosapentaenoic acid (EPA). After years of trial failures when an EPA-docosahexaenoic acid (DHA) combination was used, a large study (REDUCE-IT) [12] that used 4 g of pure EPA (as in the JELIS [13] trial in the past, but with 2 g) showed a significant CV benefit independently of LDL-C reduction. (A link to the Podcast &Video with Prof. Drexel: Podcast: V15C4 & Video: V15C6 will be inserted here).
The REDUCE-IT trial showed that the use of EPA 2 g twice daily was superior to placebo in reducing TGs, CV events, and CV death among patients who had high TGs and either known CVD or those at high risk for developing it, and who were already on statin therapy with relatively well controlled LDL-C levels.
Study design
In the REDUCE-IT study, 8,179 patients with established CVD or age >50 years with diabetes and ≥1 additional risk factor, a fasting TG level from 135 to 499 mg/dl and LDL-C levels from 41 to 100 mg/dl were randomised in a 1:1 fashion to either EPA (2 g twice daily with food; n=4,089) or a matching placebo (n=4,090). Randomisation was stratified by primary versus secondary prevention, use of ezetimibe, and geographical region. The mean age was 60.4 years, 28% were women, and the mean follow-up was 4.9 years. A total of 70.7% patients were on secondary prevention; 94% were taking moderate- or high-intensity statins, and 6.4% ezetimibe. Diabetes was present in 59%.
Principal findings
The primary CV outcome of CV death, non-fatal MI, stroke, coronary revascularisation, or unstable angina for EPA versus placebo was 17.2% vs 22.0% (HR 0.75, 95% CI: 0.68-0.83; p<0.0001).
The secondary outcomes for EPA compared with placebo demonstrate a reduction in TG levels at 1 year (−39.0 mg/dl vs 4.5 mg/dl). CV death or MI, all MI and revascularisation significantly decreased (p<0.001). All-cause mortality was reduced from 7.6% to 6.7% (p=0.09). No serious adverse bleeding events were noted; atrial fibrillation was more frequent in the active group (5.3% vs 3.9%).
Total and recurrent event analysis
Of these events, 55.2% were first primary events. Total (first and subsequent) primary endpoint event rates were reduced to 61 from 89 per 1,000 patient-years for EPA versus placebo, respectively (rate ratio [RR] 0.70, 95% CI: 0.62-0.78; p<0.0001). The first occurrence of a primary composite endpoint was reduced with icosapent ethyl (IPE) versus placebo (HR 0.75, 95% CI: 0.68-0.83; p<0.0001), as was the second occurrence (HR 0.68, 95% CI: 0.60-0.78; p<0.0001). Similar effects were noted for key secondary endpoints.
The benefit of EPA versus placebo was maintained across the baseline EPA level tertiles (<20 mcg/ml, 20-34 mcg/ml, >34 mcg/ml) for the primary and key secondary endpoints. The median baseline EPA level of 26.1 increased by ̴400% at 1 year and was sustained up to 5 years in the IPE arm (p<0.0001), while it remained more or less unchanged in the placebo arm. On-treatment EPA levels correlated with the primary endpoint, key secondary endpoint, and most other CV endpoints. The benefits noted were beyond those that could be explained by the degree of TG or other biomarker changes such as LDL-C, HDL, or hsCRP.
Interpretation
The use of EPA 2 g twice daily was superior to placebo in reducing TGs, CV events, and CV death among patients who had high TGs and either known CV disease or who were at high risk for developing it, and who were already on statin therapy with relatively well controlled LDL-C levels. Results were consistent among patients with diabetes and those with prior MI, and across the spectrum of kidney function. Rates of revascularisation and MI (all types) were lower, while atrial fibrillation/flutter and bleeding were higher with EPA.
These are very interesting findings and follow on the heels of several negative trials with n-3 fatty acid supplementation, which has a higher dose of purified EPA (4 g/day) than what was tested in other clinical trials. This is one of the first non-LDL-C targeted trials to show a CV benefit.
Table 1. New drugs and indications.
INCLISIRAN
-
-
Adults with primary hypercholesterolaemia (heterozygous familial and non-familial) or mixed dyslipidaemia, as an adjunct to diet:
- in combination with a statin or a statin with other lipid-lowering therapies in patients unable to reach LDL-C goals with the maximum tolerated dose of a statin
or
- alone or in combination with other lipid-lowering therapies in patients who are statin-intolerant, or for whom a statin is contraindicated.
-
BEMPEDOIC ACID
-
-
Adults with primary hypercholesterolaemia (heterozygous familial and non-familial) or mixed dyslipidaemia, as an adjunct to diet:
- in combination with a statin or a statin with other lipid- lowering therapies in patients unable to reach LDL-C goals with the maximum tolerated dose of a statin
or
- alone or in combination with other lipid-lowering therapies in patients who are statin-intolerant, or for whom a statin is contraindicated.
-
EPA
Adult statin-treated patients at high cardiovascular risk with elevated triglycerides (≥150 mg/dL [≥1.7 mmol/L]) and:
-
- established cardiovascular disease
or
-
- diabetes and at least one other cardiovascular risk factor.
EPA: eicosapentaenoic acid; LDL-C: low-density lipoprotein cholesterol
Impact on practice
- In patients with compliance issues, inclisiran on top of a statin-ezetimibe combination can provide significant improvement when administered twice a year.
- Bempedoic acid in a single-pill combination with ezetimibe could be very helpful for patients who present with statin-related-myalgia or who are afraid of being considered statin intolerant and thus refused medication.
- Omega-3/EPA are prescribed in secondary prevention patients with high TGs, but their benefit in reducing CV death is independent of their anti-TG action.