Take-home messages
1. Two AMVP phenotypes are linked to ventricular arrhythmias: AMVP with severe degenerative mitral regurgitation (DMR) and AMVP with severe myxomatous disease irrespective of DMR severity.
2. AMVP phenotypic characterisation relies on imaging tools. Repolarisation abnormalities, when present, must draw attention.
3. Mitral annular disjunction is frequent at MVP diagnosis and is associated with ventricular arrhythmia occurrence but does not have excess mortality with the first years of diagnosis.
4. Ventricular arrhythmia development in MVP is progressive over time.
Impact on practice statement
- When diagnosing MVP, it is important to consider an AMVP phenotype.
- MVP diagnosis requires a 24h Holter-ECG arrhythmia assessment.
- Repeated arrhythmia monitoring is required for AMVP phenotypes without severe ventricular arrhythmias at index monitoring.
Abbreviations
AMVP arrhythmic mitral valve prolapse
DMR degenerative mitral regurgitation
MVP mitral valve prolapse
SCD sudden cardiac death
VA ventricular arrhythmia
VT ventricular tachycardia
Introduction
Since the first mitral valve prolapse (MVP) description based on auscultatory findings, reports on outcome have alternated between descriptions of few complications [1] and case reports of sudden cardiac deaths (SCD) [2] unexplained by any other obvious conditions. The issue of MVP outcome long remained undefined until population-based studies accounting for MVP heterogeneity at baseline suggested that MVP without “significant” degenerative mitral regurgitation (DMR) or left ventricular (LV) dysfunction is a benign condition [3], an assertion confirmed in large cohorts. However, literature on MVP has been peppered with case reports of patients who suffered occurrence of SCD and were found to be carriers of isolated, apparently uncomplicated, MVP.
It is clearly established that patients with MVP with no/trivial DMR, as a group, have a normal life expectancy [3], confirmed by autopsy series showing no excess MVP representation among cases of otherwise unexplained SCD. Thereafter, the prognosis of isolated MVP with no or mild DMR has generally been considered benign. However, the cohort studies have also revealed heterogeneous MVP outcomes, dominated by DMR severity and LV dysfunction [3] raising the possibility of small subsets that may be at risk among MVP patients without significant DMR, which may not be detectable among large cohorts or autopsy registries.
This debate was recently reignited by a small case series of “malignant” bileaflet MVP patients with little DMR, who presented with resuscitated cardiac arrest and completely negative enquiries for other SCD causes, including genetic testing.
Furthermore, patients with MVP, flail leaflet and significant mitral regurgitation (MR; grade 3-4) but without symptoms or LV dysfunction were noted to have twice the SCD risk as the general population [4]. However, questions remain as to whether SCD occurred with or because of MVP; whether an MVP patient subset could be defined as being at high-risk for arrhythmias, but still small enough so as to be compatible with the overall benign outcome of MVP occurring with none, or mild DMR. This difficult question of causality, in the absence of a definite clinical trial, was thus approached based on the association of MVP phenotype with ventricular arrhythmias.
A retrospective cross-sectional study of patients who had recovered from cardiac arrest with no other potential cause than MVP, underscored a common phenotype characterised clinically by frequent syncope/presyncope, morphologically by severe myxomatous disease with marked redundancy and mitral annular disjunction (MAD) and electrocardiographically by frequent ST-T changes and arrhythmias originating from the mitral complex [5]. Furthermore, a cohort study of patients with MVP in whom arrhythmias were quantified by Holter monitoring suggested a similar association between the severity of ventricular arrhythmias and severe mitral myxomatous disease (often but not exclusively bileaflet MVP) with marked leaflet redundancy and frequent MAD detected by echocardiography, as well as frequent ST-T abnormalities [6]. Finally, among these coherent data, MAD detected by magnetic resonance imaging was associated with ventricular arrhythmias [7]. Furthermore, myocardial fibrosis detected by MRI was found to be strongly associated to the arrhythmic phenotype [7]. These coherent data, confirmed in meta-analysis, suggested a definite arrhythmic MVP (AMVP) phenotype that would affect a small subset of patients with MVP at concentrated high-risk.
The arrhythmic mitral valve prolapse phenotypes
AMVP is defined per guidelines as the combination of MVP (with or without MAD), with frequent and/or complex ventricular arrhythmia, in the absence of any other well-defined arrhythmic substrate (e.g., primary cardiomyopathy, channelopathy, active ischaemia, or ventricular scar due to another defined aetiology), regardless of MR severity [8]. This overt AMVP “at-risk” for SCD may be preceded by phenotypes not yet associated with overt arrhythmias but “at-risk” for developing malignant arrhythmias.
Accordingly, two phenotypes can be identified:
- AMVP due to severe degenerative mitral regurgitation
Patients with MVP and severe MR showed high-risk of excess mortality including excess SCD compared to the general population [4], irrespective of valvular morphology. Atrial arrhythmias, reduced LV systolic function and severe heart failure symptoms are associated with an increased SCD risk, but even without such risk factors, MVP with at least moderate to severe MR yields excess mortality [9] and SCD, with double the incidence compared to the general population [4]. Surgical MR correction in observational cohorts tends to markedly reduce ventricular arrhythmic events [10], and SCD rates [4], and restores life expectancy by reducing overall mortality [9]. - Arrhythmic MVP with severe myxomatous disease irrespective of DMR
The overall survival of the MVP subset without severe MR or LV dysfunction, is overall equivalent to that of the general population [3]. However, patients with severe myxomatous disease with marked redundancy, excess leaflet length/thickness and MAD, irrespective of DMR severity, are prone to develop arrhythmia over time. This phenotype requires careful interpretation of imaging and can also be demonstrated by MRI [7], which additionally measures the severity and location of myocardial fibrosis. A small percentage (9%) present with high-risk arrhythmias (ventricular tachycardia [VT] >180 bpm), while presentation with frequent extrasystole or slower non-sustained VT is more frequent and sustained VT is quite rare. Patients with presyncope or syncope are at particular risk of life-threatening ongoing arrhythmias and should undergo prompt monitoring of long duration. These patients often also present with inferior ST-T changes and premature ventricular complexes generally originating from the mitral complex. This small subset may need consideration for therapy, involving mitral repair (with significant DMR) and/or implantable cardioverters. While patients without overt arrhythmia and this phenotype are at risk of developing arrhythmias in the future, this outcome may take years to develop. In and by itself this phenotype is not an indication for therapy but rather for repeated/extended cardiac monitoring. Hence, even in this at-risk AMVP subset, the clinical context is quite heterogeneous and warrants careful identification of MVP arrhythmic complications.
AMVP evaluation: clinical and imaging tools
Syncope
Syncope is uncommon (2-3.6%) in unselected subjects with MVP [11] but is reported in 35% of MVP patients with malignant arrhythmias or SCD. Furthermore, in a large MVP cohort, syncope was more frequently reported with documented severe ventricular arrhythmias [6]. Therefore, syncope and particularly unexplained syncope, markedly raises the concern for malignant arrhythmias. Palpitations and chest pain are frequent but in similar proportions in MVP with and without ventricular arrhythmias [6,8].
Electrocardiography
Electrocardiographic repolarisation abnormalities, such as T-wave inversion (TWI) at rest, often in inferior and lateral leads, are independently associated with AMVP and ventricular arrhythmias [6]. These repolarisation abnormalities are thought to be linked to abnormal stretch of papillary muscles and adjacent myocardium and/or locally disturbed repolarisation [8].
Echocardiography
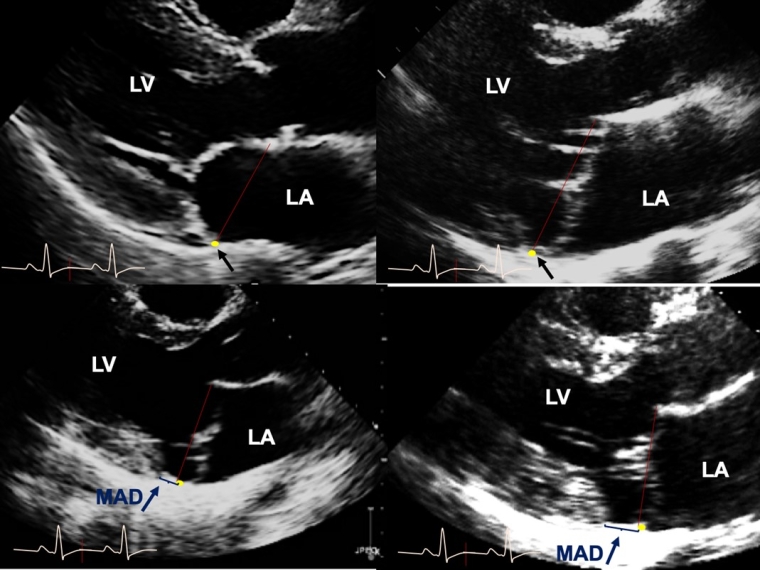
Echocardiographic morphologic features of AMVP are severe myxomatous degeneration, defined by thick and redundant leaflets with multisegment bileaflet MVP and MAD [5,6,12] (Figure 1). Importantly, bileaflet MVP, quite prevalent among patients with MVP, is not independently an SCD trigger in large cohorts or population-based studies [3]. Conversely, MAD with MVP is independently linked with ventricular arrhythmias at diagnosis or develops during follow-up [10]. Whether MAD distance predicts more frequent arrhythmias is unclear as are MAD-associated arrhythmia mechanisms, although myocardial fibrosis is often noted with longer MAD and hypothesised as causative.
Figure 1. Mitral valve prolapse and mitral annulus disjunction by transthoracic-echocardiography.
(Upper-row left) The transthoracic echocardiographic long-axis view in end-systole displaying normal mitral valve without MVP, (upper-row right) with myxomatous bileaflet MVP but no MAD, and myxomatous MVP with MAD of 4 mm length (lower-row left) and of 12 mm length (lower-row right). The red line characterises the mitral annular plane, the yellow dot with single black arrow the insertion of the posterior mitral leaflet mitral annulus and the single blue arrow MAD.
LA: left atrium; LV: left ventricle, MAD: mitral annulus-disjunction; MVP: mitral valve prolapse
Reproduced with permission from Eur Heart J 44(33): 3121-3135.
Cardiac magnetic resonance imaging
Cardiac magnetic resonance imaging (MRI) is useful for arrhythmic risk stratification of MVP, due to its unique ability to identify focal myocardial fibrosis using late gadolinium enhancement (LGE). Overall, fibrosis is common in MVP (28-37%) [13], and is usually located adjacent to the mitral annulus in the basal left ventricular wall including papillary muscles, inferolateral and inferior walls [14] (Figure 2). Despite the lack of a large cohort assessing LGE in AMVP, multiple studies have suggested an association between LGE at the mid-wall of the papillary muscles or patchy mid-wall non-ischaemic fibrosis in the LV infero-basal region, and complex ventricular arrhythmias [13]. While fibrosis location within the mitral apparatus (papillary muscles and peri-annular region) is considered to be pathophysiologically associated with arrhythmia in MVP, the diffuse interstitial fibrosis particularly involving the basal segments appears to be a precursor of established replacement fibrosis seen by LGE. Additionally, MRI can identify MAD [7], yet even by this method the link between MAD extent and ventricular arrhythmias remains ill-defined [7]. However, the coherence of echocardiographic and MRI findings definitely points towards the importance of MAD in the development of these arrhythmic complications.
Figure 2. Mitral valve prolapse and mitral annulus disjunction by cardiac MRI.
(Upper-row left) Cardiac MRI 4 chamber view of a 66-year-old male with near-syncope and sustained VT, normal coronaries, MVP and moderate MR. Note the yellow arrow displaying the insertion of the posterior leaflet on the mitral annulus in mid-diastole. (Upper-row right) Long-axis view in end-systole displaying with bileaflet MVP with MAD and (lower-row left) basal inferior-lateral fibrosis by LGE. Note the mitral annular plane characterised by the red line, the posterior mitral annulus by the yellow single arrow, MAD length by the double blue arrow and fibrosis by the single red arrow. (Lower-row right) Short-axis view after LGE shows fibrosis located in the papillary muscles (single red arrows).
LGE: late gadolinium enhancement; LV: left ventricle, MAD: mitral annulus disjunction; MR: mitral regurgitation; MRI: magnetic resonance imaging; MVP: mitral valve prolapse
Reproduced with permission from the figures of Eur Heart J 44(33): 3121-3135.
Computed tomography scan
Computed tomography (CT) scan can be useful to detect MAD, and its extent to P1 and P3 scallops of the posterior leaflet, by taking advantage of its high spatial resolution although it is hindered by lower temporal resolution compared to echocardiography. The three-dimensional datasets obtained with CT can be useful in assessing the anatomy of fibrous areas of the mitral apparatus and mitral calcifications, important for mitral valve repair [15].
Positron emission tomography
Positron emission tomography (PET) MRI imaging of the AMVP demonstrates subclinical myocardial inflammation coexisting with areas of myocardial fibrosis in patients with severe degenerative MR, even in asymptomatic patients. This seminal research warrants further investigation to establish its independent role in the arrhythmic trigger and overall incremental prognostic value in AMVP outcome [16].
Mitral annular disjunction: physiopathology, imaging diagnosis and prognostic implication
MAD is a functional alteration of the mitral anatomy whose annulus normally involves different attachments for anterior and posterior leaflets. The annulus supporting the anterior leaflet is part of the heart’s fibrous core in continuity with the fibrous trigones and the aortic annulus. It is highly fibrous and not prone to disjunction from its attachments. Conversely, the annulus portion, supporting the posterior leaflet while occupying 2/3 of the circumference, is much thinner and is implanted in the ventricular myocardium while supporting the base of the posterior mitral leaflet and the fibrous end of the left atrial wall. Thus, the mitral annulus ensures electric isolation of atrium/ventricle, provides mechanical support for the posterior leaflet and allows appropriate coupling of atrial to ventricular systole [17].
Confusion arises from definitions of annular disjunction, alternatively reported as microscopic, of limited extent and present in almost all individuals [18], larger but also present in most normal individuals [19], to macroscopic and part of the slippage associated with myxomatous degeneration of valvular/annular tissue [10]. It is the latter definition which is retained clinically.
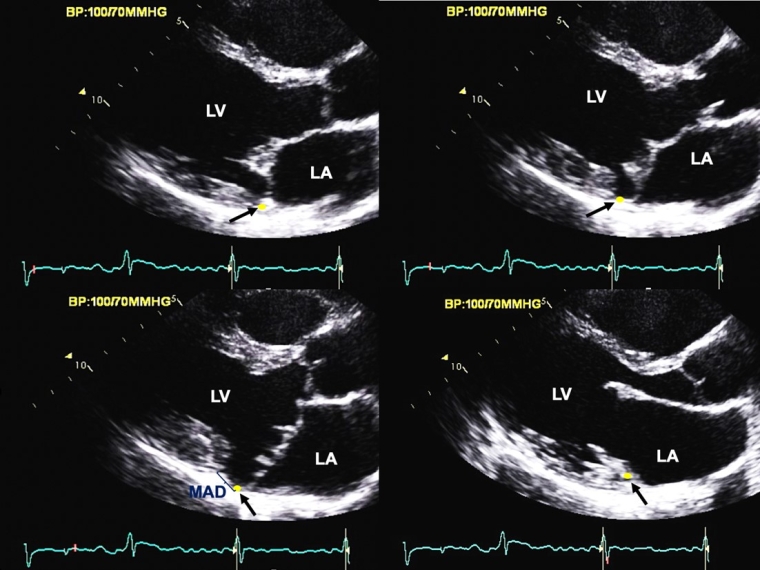
MAD, in the clinical setting, is characterised by macroscopic detachment of the mitral annulus supporting the posterior mitral leaflet from adjacent ventricular myocardium [20]. Hence, MAD is associated with partial loss of mechanical annular function which is dependent on its normal ventricular myocardial attachment while electrical isolation of the left atrium/ventricle is maintained [10,21]. MAD is predominantly observed at the insertion site of the posterior physiologic leaflet, extending laterally variably under all scallops but preferentially under the P2 scallop. MAD is not uniformly observed in MVP, detectable by echocardiography in approximately 1/3 of patients [10]. While MAD has been hypothesised as causing MVP, its inconsistent presence argues in favour of MAD and MVP being variable consequences of myxomatous degeneration. Diagnosis requires high spatial/temporal resolution imaging, in long-axis views by transthoracic echocardiography [22] or MRI [7] through dynamic frame-by-frame analysis with careful examination of mitral annulus position [8] (Figure 3). MAD depth measurement begins at the posterior leaflet insertion site on the annulus/left atrial wall, and ends at the detached LV myocardium in systole [7,23]. MAD may occur in any form of MVP, but is most common in advanced myxomatous degeneration with bileaflet MVP, with longer, thicker and redundant leaflets, larger mitral annulus, independent of all other characteristics [7,10]. The term “curling” is used to refer to the deformation of the posterior leaflet assumed to remain attached to the ventricular myocardium but we find it a misnomer as the annulus is almost completely detached from the myocardium with MAD [24]. Emerging data suggest that tricuspid annulus disjunction may coexist with MAD [25].
Figure 3. Frame-by-frame analysis of the mitral apparatus by transthoracic echocardiography in a parasternal long-axis view within the entire cardiac cycle.
(Upper-row left) The yellow dot with the single black arrow characterises the position of the posterior mitral annulus in early systole and (upper-row right) mid-systole. Note the prolapse of the mitral leaflets appearing in mid-systole, more pronounced on the posterior leaflet, and the absence of posterior annular disjunction yet. (Lower-row right) Late systole view showing bileaflet MVP with MAD (single blue arrow) defined as a detachment of the posterior mitral annulus (yellow dot/single black arrow) from the adjacent LV myocardium. (Lower-row right) Early diastole view showing restored continuity between the insertion site of the posterior leaflet on the mitral annulus and the LV myocardium, emphasising the necessity of image-by-image analysis of the mitral valve for MAD measurement in end systolic view after identification of the insertion of the posterior MV leaflet in early systole.
LV: left ventricle, MAD: mitral annulus disjunction; MV: mitral valve; MVP: mitral valve prolapse
Reproduced with permission from the figures of Eur Heart J 44(33): 3121-3135.
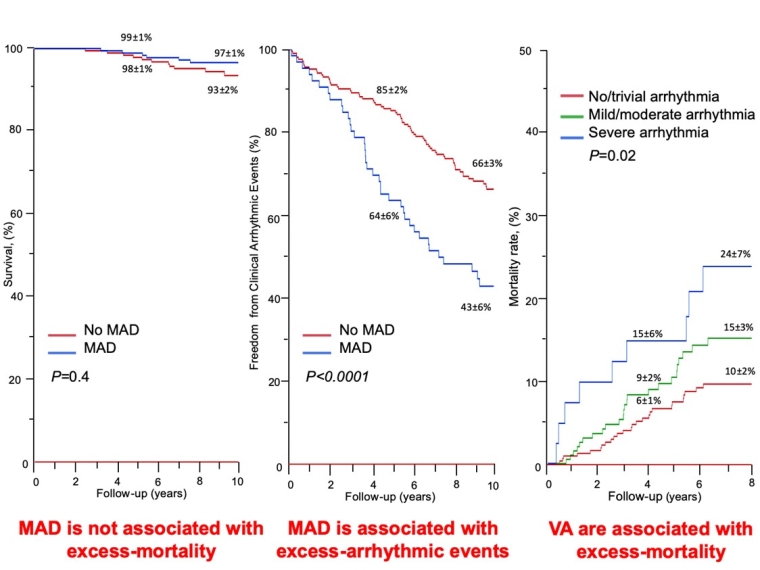
Physiologic consequences of MAD include an LV remodelling, to a greater extent than that justified by DMR, irrespective of age [7,10,26]. This association is understood as consequential to the de-anchoring of the LV myocardium from the roots of the mitral annulus, raising concerns for permanent consequences from MAD on the LV. Potential explanations for excess LV remodelling with MAD include LV atrophy versus fibrosis as consequence of annular detachment [24]. MAD is also associated with abnormal annular movement, widening in late systole (unanchored annulus) tending to enhance the separation of posterior and anterior leaflets [26]. While longitudinal data are lacking, MAD likely progresses with aging [27]. Progressive detachment may be linked to peri-annular inflammation and possibly to LV basal fibrosis [28], and to arrhythmia development. MAD’s clinical link to progressive development of ventricular arrhythmias is now well established [10]. Indeed, patients with MAD at MVP diagnosis have a 2-fold increase in the cumulative probability of arrhythmic events, particularly VT, compared to those without MAD. The incidence of arrhythmic events tends to be progressive, affecting close to 1/3 of patients five years after diagnosis and 2/3 at 10 years after diagnosis but is much higher than in patients without MAD. Thus, MAD at MVP diagnosis is a harbinger of ventricular arrhythmias, but often these are delayed during follow-up, emphasising the very reassuring absence of excess mortality after MAD diagnosis [6] (Figure 4). Thus, with MAD, prudent MVP management should remain the rule. However, once severe ventricular arrhythmias are detected, particularly VT ≥180 bpm, subsequent excess mortality is observed, warranting appropriate and prompt therapeutic interventions based on the arrhythmias diagnosed [6].
Figure 4. Survival impact of MAD and ventricular arrhythmia long-term by MAD presence in age-matched cohort.
(Left-panel) Survival stratified by MAD groups of matched age, body mass index, coronary artery disease history, atrial fibrillation and comorbidity index. Note the comparable mortality between MAD groups. (Middle-panel) Overall survival free of clinical arrhythmic event stratified by MAD. Note the substantial reduction of arrhythmic event-free survival with MAD presence. (Right-panel) Mortality rate of MVP stratified by ventricular arrhythmia severity in overall cohort. Note the mortality difference with ventricular arrhythmia severity, considerable when severe. Kaplan-Meir curves indicate estimated survival±standard error.
MAD: mitral-annulus-disjunction; MVP: mitral valve prolapse; PVC: premature ventricular contraction; VT: ventricular tachycardia.
Reproduced with permission from the Figures of J Am Coll Cardiol. 2020 Aug, 76 (6) 637–649, J Am Coll Cardiol Img. 2021 Nov, 14 (11) 2073–2087 and Eur Heart J 44(33): 3121-3135.
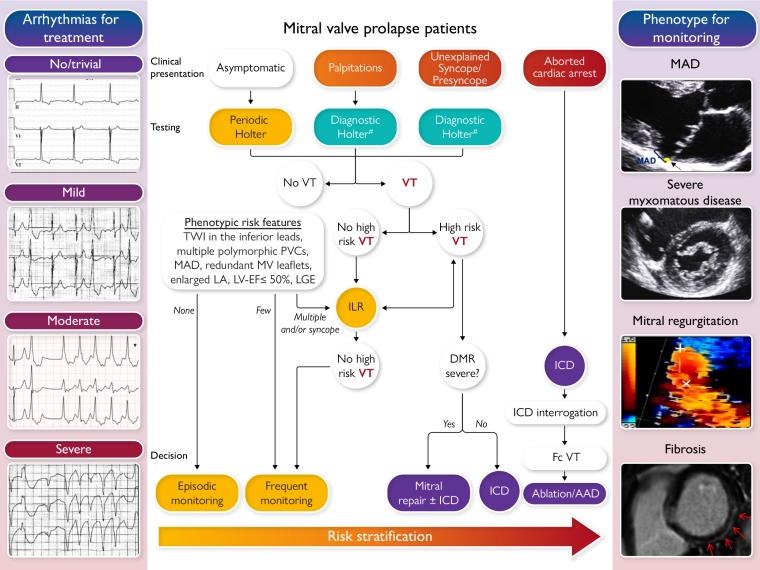
AMVP risk stratification (graphical abstract)
Risk stratification of AMVP relies first on clinical presentation and cardiac imaging tools, and therefore dictates the intensity of arrhythmia screening. The arrhythmia severity detected by monitoring [6] then guides both frequency of follow-up and therapeutic interventions. Indeed, not all patients with MAD present with arrhythmias [10], and not all arrhythmias detected are associated with excess mortality [6]. Thus, MVP itself should trigger reassurance in the absence of significant DMR, clinical complications or severe arrhythmia. The detection of an MVP phenotype predisposing to arrhythmias or of ventricular arrhythmias of a mild or moderate grade represent an elevated risk and therefore warrant more frequent rhythm monitoring. Indeed, the arrhythmia detected is the crucial element that will trigger the therapeutic decision and not the MVP phenotype alone. Prompt therapeutic intervention is solely indicated by severe ventricular arrhythmias (and not MAD presence), particularly if those are associated with syncope or presyncope [5].
Clinical/echocardiographic presentation
A clinical/echocardiographic presentation with presyncope or unexplained syncope strongly raises suspicion of an ongoing severe arrhythmia. Phenotypic risk features such as negative T waves, severe myxomatous degeneration with redundant leaflets, MAD, or LGE by MRI represent a higher risk of ongoing or future ventricular arrhythmias. Therefore, the clinical and imaging context strongly influences the intensity of rhythm monitoring [8]. For example, patients presenting with unexplained syncope, even without VT on Holter monitoring are prime candidates to undergo extended ECG monitoring by long-duration Holter or preferably an implantable loop recorder (ILR), to uncover ventricular arrhythmias with the highest sensitivity. It should be noted that the risk-benefit ratio of this intensified rhythmic enquiry remains to be determined.
Conversely, asymptomatic patients without complex ventricular arrhythmia on the initial screening Holter would only require episodic Holter assessment by primary care practitioners, more frequently if they present with phenotypic risk features. Because ventricular arrhythmias may develop secondarily, rhythmic reassessment over time is warranted, and its frequency/intensity depend on presence/number of phenotypic risk features [8]. The role of electrophysiologic (EP) studies is unknown but is not considered to replace Holter or ILR monitoring in screening for spontaneous ventricular arrhythmias [29]. Indeed, while induced monomorphic VT is more specific than polymorphic VT, arrhythmia induction by EP studies can be non-specific [8].
Arrhythmia severity by Holter
Arrhythmia severity by Holter is the main determinant of intensity/frequency of repeated rhythmic screening and of medical/surgical therapy. Sustained VT, spontaneous polymorphic nonsustained VT (NSVT) and rapid monomorphic NSVT (>180 bpm) are considered harbingers of SCD. Polymorphic, frequent and complex ventricular extrasystole, monomorphic NSVT at a lower rate (<180 bpm) are all considered intermediate-risk arrhythmias. Isolated frequent monomorphic ventricular extrasystole are considered low-risk. In case of asymptomatic MVP without arrhythmia at index Holter, the absence of further phenotypic risk factors will indicate episodic Holter-ECG monitoring whereas more frequent monitoring by Holter or ILR is advised in case of multiple phenotypic risk factors. Conversely, the presence of palpitations and/or presyncope/syncope without severe VT at index Holter will trigger prompt ILR implantation to guide the therapeutic approach [8].
This management scheme is summarised by the Central illustration below [8,30].
(Left panel, from top-to-bottom) No/trivial, mild, moderate and severe ventricular arrhythmia. (Middle panel) Risk stratification aiming at assessing the risk of VAs and SCD in patients with MVP, involving two phases based on the clinical and imaging context and the uncovered arrhythmia. In the absence of ventricular tachycardia, phenotypic risk features will trigger the intensity of screening for arrhythmia. Green boxes indicate green heart consensus statements and yellow boxes indicate yellow heart consensus statements. High risk=sustained VT, polymorphic NSVT, fast (>180 bpm) NSVT, VT/NSVT resulting in syncope. (Right panel, from top to bottom) The arrhythmic MVP imaging phenotype with bileaflet MVP and MAD, leaflet redundancy, mitral regurgitation severity and LGE.
ICD: implantable cardioverter defibrillator; LA: left atrium; LGE: late gadolinium enhancement; LV-EF: left ventricular ejection fraction; MAD: mitral annular disjunction; MVP: mitral valve prolapse; PVC: premature ventricular contractions; TWI: T-wave inversion; VA: ventricular arrhythmia; VT: ventricular tachycardia
#Additional ECG monitoring method may be used such as loop recorders.
Reproduced with permission from the Figures of J Am Coll Cardiol. 2020 Aug, 76 (6) 637–649, EP Europace, Volume 24, Issue 12, December 2022, Pages 1981–2003 and Eur Heart J 44(33): 3121-3135.