Impact on practice statement
There is strong evidence of the benefits of treating hypertension in the elderly. In the elderly, polypathology and polypharmacy, drug-drug interactions, side effects, reduction in compliance, specific conditions like orthostatic hypotension or dysautonomic diseases, and the condition of frailty can all contribute to the creation of complications and challenges in the treatment of many patients. Revision of blood pressure targets and tailored therapies could be considered in some cases.
Take-home messages
- Hypertension is highly prevalent in older patients. There are specific risks and threats in treating hypertension in the elderly: polypathology, polytreatments, reduced compliance, special conditions, frailty.
- Blood pressure targets for elderly patients: individualised treatments.
- Common adverse effects of antihypertensive drugs: special considerations in older adults,
- Adherence to treatment: specific issues.
Patient-oriented messages
- If you are over 70 you need to measure your blood pressure. If you are diagnosed with hypertension, you need to treat this condition because by treating it you could reduce both your cardiovascular and overall risk.
- When measuring blood pressure, take the measurement after standing up. Your blood pressure shouldn't drop more than 20 mmHg, and you shouldn't feel dizzy after standing up. However, be careful when moving to the orthostatic position after lying down in bed (particularly during the night, after long periods of illness, fever, low hydration...) to avoid harmful drops in blood pressure values.
- If your blood pressure is high, you can encounter some difficulties in managing this condition. This is particularly true if you are taking other drugs for different diseases, if you forget to take medications or if you have a disease like Parkinson’s or problems with your blood pressure dropping abruptly when you stand up.
- According to the ESC guidelines you should be treated as a younger patient; however, if you are more than 80 years old or you are “frail” according to a medical diagnosis, your blood pressure should ideally be maintained around 130 to 140 mmHg for the systolic and 80 to 90 mmHg for the diastolic pressure, if tolerated. In this case you will probably be prescribed a monotherapy as a first-line strategy.
- As we age, it is possible that the drugs you have taken for many years are no longer suitable or work for you. Talk to your doctor about modifying your medications.
Introduction
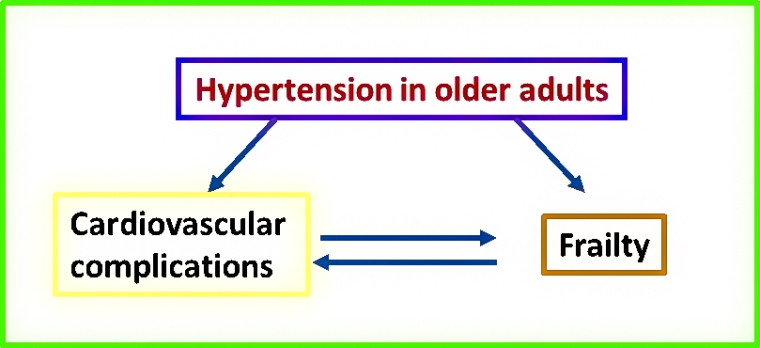
Hypertension is frequently found in patients aged 65 or older and represents a risk factor for various cardiovascular diseases such as heart failure, atrial fibrillation, stroke, kidney diseases and dementia. Moreover, hypertension in the elderly is associated with an accelerated decline in health status and frailty [1]. Frailty is defined as a condition of increased vulnerability to stressors leading to a reduced ability to combat potential acute negative events and reduced ability to maintain homeostasis. Frailty can lead to an increased risk of adverse health outcomes [2-6] (Figure 1).
Hypertension and frailty are closely interconnected. Hypertension may lead to frailty and may produce frailty and disability through cardiovascular complications.
Risks and threats in treating hypertension in the elderly: polypathology, polytreatments, reduced compliance, special conditions, frailty
A major concern when treating older patients with antihypertensive drugs should be hypotension, particularly orthostatic hypotension and post-prandial hypotension.
Orthostatic hypotension, defined as a fall of systolic BP more than 20 mmHg from supine to standing position, affects the prognosis of older people by increasing the risk of syncope and falls and, in turn, increases cardiovascular risk and all-cause mortality [1,6]. When treating hypertension in the elderly, antihypertensive therapies should be carefully titrated, taking into account the standing position which should be part of the standard evaluation in older patients and in frailty [6].
In particular, dysautonomic diseases such as Parkinson’s disease, diabetes and frailty should be carefully considered in order to avoid orthostatic hypotension.
Other concomitant conditions associated with potential adverse effects during antihypertensive treatments that should be considered are aortic stenosis, heart failure, atrial fibrillation, reduced renal function, endocrine diseases such as thyroid disease, and associated polytherapy.
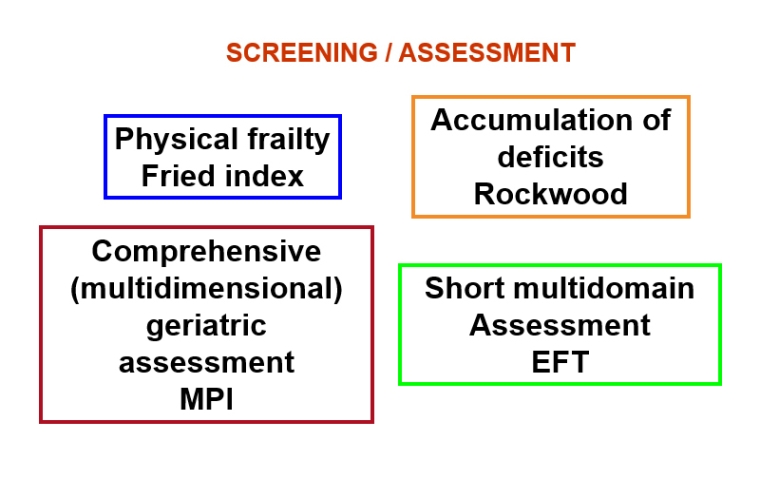
Frailty should be screened for and assessed using validated tools [6,7]. These tools investigate the various domains of frailty and may focus mainly on physical frailty, on the accumulation of deficits, or may perform a multidimensional assessment, even in a brief form [6] (Figure 2).
The figure indicates some of the validated screening/assessments for frailty according to the subtype of frailty investigated. EFT: essential frailty toolset; MPI: multidimensional prognostic index
Blood pressure targets in the elderly: individualised treatments
Although the treatment of hypertension in the elderly is undoubtedly a main goal for cardiovascular prevention to reduce both morbidity and mortality, blood pressure targets in hypertensive older patients are not fully defined [1,8,9].
There is limited evidence in published trials on the balance between benefits and adverse events in treating hypertension to lower blood pressure targets in the elderly. This is due to the exclusion of elderly patients with multimorbidities and the lack of investigations into the degrees of frailty.
Particular subgroups of older patients, such as institutionalised patients, those requiring nursing, or those with dementia are underrepresented in clinical research. Patients with orthostatic hypotension are often excluded as well.
Moreover, heterogeneous frailty evaluations have been reported: the intake of a greater number of antihypertensive drugs, increased presence of comorbidities, malnutrition and overtreatment have been used as proxy of frailty [10-12].
Guideline recommendations are inconsistent, especially for adults aged 80 years and older, as shown by a recent systematic review [13]. Thirty-four guidelines provided recommendations concerning antihypertensive drug therapy in older adults, most of which were set on chronological rather than biological age.
Neutral or adverse effects on mortality from targeting low blood pressure values in older adults have been reported. In a recent review of patients with frailty, no difference in all-cause mortality between systolic blood pressure <140 mmHg and ≥140 mmHg was found [14]. In a large administrative database [15], patients with frailty who showed a systolic blood pressure below 130 mmHg were found to have an excess of all-cause mortality, without benefits to cardiovascular risk. The blood pressure target of 150/80mmHg in adults aged 80 or older was associated with lower mortality after adjustment for baseline frailty in the HYpertension in the Very Elderly Trial (HYVET) [16]. When frailty was assessed by an accumulation-of-deficit index such as the frailty index, no evidence was reported regarding potential interactions between this baseline index and treatment with antihypertensives for the occurrence of stroke, all-cause death, or cardiovascular events in very old patients. Both frail and fit participants benefitted from treatment [17]. However, it should be underlined that a standing systolic blood pressure >140mm Hg was required as a study protocol in the HYVET trial.
The current ESC guidelines suggest specific recommendations for very old or frail patients: to maintain a 130 to 140 mmHg systolic target and 80 to 90 mmHg diastolic target, if tolerated, and to consider monotherapy as a first-line strategy in these patients [18].
While waiting for stronger evidence, the best way to handle the potential benefit/harm ratio in treating hypertension in the elderly is to consider the individual condition of the patient, with an integrated evaluation of their characteristics and care environment, taking into account pharmacokinetical changes due to advanced age and the risk of drug interactions.
Common adverse effects of antihypertensive drugs: special considerations in older adults
Antihypertensive drugs may have specific adverse effects requiring specific precautions in individuals aged 80+ years, for a comprehensive view refer to Table 3 of Benetos et al [19].
Adherence to treatments: specific issues
A critical point in treating patients with hypertension is adherence and persistence to treatment. This is particularly true when treating the elderly [1]. Moreover, shared decision making about treatments aimed at prevention is mandatory in older adults. Besides potential adverse reactions to drugs, other challenges that the elderly may face include difficulty in taking the prescribed therapy, difficulty in accessing a doctor’s office or hospital due to physical impairment, difficulty in accessing prescribed drugs, dementia and forgetfulness leading to missed appointments or other scheduled therapies. The use of digital health technologies may help to support both correct drug timing and adherence, and teleconsultations and other interactions with caregivers can be beneficial as well [20].
Conclusions
Hypertension in the elderly should be treated to reduce morbidity and mortality. Blood pressure targets in older adults should be tailored on an individualised basis, according to the presence of orthostatic hypotension, comorbidities, potential polytherapy, and the potential presence of frailty.
Note to editors
Authors: Luigina Guasti1, MD, PhD, FESC, Giovanni Gaudio1,2, MD
- University of Insubria, Department of Medicine and Surgery, Varese-Como, Italy;
- Ospedale Bellini, Somma Lombardo, Varese, Italy
Address for correspondence:
Associate Professor Luigina Guasti, University of Insubria, Department of Medicine & and Surgery, Varese, Italy
Author disclosures:
The authors have no conflicts of interest to declare.
References
- Guasti L, Ambrosetti M, Ferrari M, Marino F, Ferrini M, Sudano I, Tanda ML, Parrini I, Asteggiano R, Cosentino M. Management of Hypertension in the Elderly and Frail Patient. Drugs Aging . 2022;39:763-72.
- Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, Cesari M, Chumlea WC, Doehner W, Evans J, Fried LP, Guralnik JM, Katz PR, Malmstrom TK, McCarter RJ, Gutierrez Robledo LM, Rockwood K, von Haehling S, Vandewoude MF, Walston J. Frailty consensus: a call to action.J Am Med Dir Assoc. 2013;14:392-7.
- Rodríguez-Mañas L, Féart C, Mann G, Viña J, Chatterji S, Chodzko-Zajko W, Gonzalez-Colaço Harmand M, Bergman H, Carcaillon L, Nicholson C, Scuteri A, Sinclair A, Pelaez M, Van der Cammen T, Beland F, Bickenbach J, Delamarche P, Ferrucci L, Fried LP, Gutiérrez-Robledo LM, Rockwood K, Rodríguez Artalejo F, Serviddio G, Vega E; FOD-CC group (Appendix 1). Searching for an Operational Definition of Frailty: A Delphi Method Based Consensus Statement. The Frailty Operative Definition-Consensus Conference Project.J Gerontol A Biol Sci Med Sci. 2013;68: 62–7.
- Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people.Lancet. 2013; 381:752–62.
- Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health.Lancet. 2019;394:1365-75.
- Richter D, Guasti L, Walker D, Lambrinou E, Lionis C, Abreu A, Savelieva I, Fumagalli S, Bo M, Rocca B, Jensen MT, Pierard L, Sudano I, Aboyans V, Asteggiano R. Frailty in cardiology: definition, assessment and clinical implications for general cardiology. A consensus document of the Council for Cardiology Practice (CCP), Association for Acute CardioVascular Care (ACVC), Association of Cardiovascular Nursing & Allied Professions (ACNAP), European Association of Preventive Cardiology (EAPC), European Heart Rhythm Association (EHRA), Council on Valvular Heart Diseases (VHD), Council on Hypertension (CHT), Council of Cardio-Oncology (CCO), Working Group (WG) Aorta & Peripheral Vascular Diseases, WG e-Cardiology, WG Thrombosis, of the European Society of Cardiology, European Primary Care Cardiology Society (EPCCS).Eur J Prev Cardiol. 2022;29:216-27.
- Vaes B, Depoortere D, Van Pottelbergh G, Matheï C, Neto J, Degryse J. Association between traditional cardiovascular risk factors and mortality in the oldest old: untangling the role of frailty.BMC Geriatr. 2017;17:234.
- Garrison SR, Kolber MR, Korownyk CS, McCracken RK, Heran BS, Allan GM. Blood pressure targets for hypertension in older adults.Cochrane Database Syst Rev. 2017;8:CD011575.
- Rivasi G, Tortù V, D'Andria MF, Turrin G, Ceolin L, Rafanelli M, Mossello E, Ungar A. Hypertension management in frail older adults: a gap in evidence.J Hypertens. 2021;39:400-7.
- Pajewski NM, Williamson JD, Applegate WB, Berlowitz DR, Bolin LP, Chertow GM, Krousel-Wood MA, Lopez-Barrera N, Powell JR, Roumie CL, Still C, Sink KM, Tang R, Wright CB, Supiano MA; SPRINT Study Research Group. Characterizing Frailty Status in the Systolic Blood Pressure Intervention Trial.J Gerontol A Biol Sci Med Sci. 2016;71:649-55.
- Anker D, Santos-Eggimann B, Zwahlen M, Santschi V, Rodondi N, Wolfson C, Chiolero A. Blood pressure in relation to frailty in older adults: A population-based study.J Clin Hypertens (Greenwich). 2019;21:1895-904.
- Basile G, Catalano A, Mandraffino G, Maltese G, Alibrandi A, Ciancio G, Lasco A, Cesari M. Relationship between blood pressure and frailty in older hypertensive outpatients.Aging Clin Exp Res. 2017;29:1049-53.
- Bogaerts JMK, von Ballmoos LM, Achterberg WP, Gussekloo J, Streit S, van der Ploeg MA, Drewes YM, Poortvliet RKE. Do we AGREE on the targets of antihypertensive drug treatment in older adults: a systematic review of guidelines on primary prevention of cardiovascular diseases.Age Ageing. 2022;51:afab192.
- Todd OM, Wilkinson C, Hale M, Wong NL, Hall M, Sheppard JP, McManus RJ, Rockwood K, Young J, Gale CP, Clegg A. Is the association between blood pressure and mortality in older adults different with frailty? A systematic review and meta-analysis.Age Ageing. 2019;48:627-35.
- Masoli JAH, Delgado J, Pilling L, Strain D, Melzer D. Blood pressure in frail older adults: associations with cardiovascular outcomes and all-cause mortality. Age Ageing. 2020;49:807-13.
- Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, Stoyanovsky V, Antikainen RL, Nikitin Y, Anderson C, Belhani A, Forette F, Rajkumar C, Thijs L, Banya W, Bulpitt CJ; HYVET Study Group. Treatment of hypertension in patients 80 years of age or older.N Engl J Med. 2008;358:1887-98.
- Warwick J, Falaschetti E, Rockwood K, Mitnitski A, Thijs L, Beckett N, Bulpitt C, Peters R. No evidence that frailty modifies the positive impact of antihypertensive treatment in very elderly people: an investigation of the impact of frailty upon treatment effect in the HYpertension in the Very Elderly Trial (HYVET) study, a double-blind, placebo-controlled study of antihypertensives in people with hypertension aged 80 and over.BMC Med. 2015;13:78.
- Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension.Eur Heart J. 2018;39:3021-104.
- Benetos A, Petrovic M, Strandberg T. Hypertension Management in Older and Frail Older Patients.Circ Res. 2019;124:1045-60.
- Guasti L, Dilaveris P, Mamas MA, Richter D, Christodorescu R, Lumens J, Schuuring MJ, Carugo S, Afilalo J, Ferrini M, Asteggiano R, Cowie MR. Digital health in older adults for the prevention and management of cardiovascular diseases and frailty. A clinical consensus statement from the ESC Council for Cardiology Practice/Taskforce on Geriatric Cardiology, the ESC Digital Health Committee and the ESC Working Group on e-Cardiology.ESC Heart Fail. 2022;9:2808-22.
















