Keywords
chemotherapy, radiotherapy, toxicity, follow-up, cardio-oncology
Abbreviation list
CPET cardiopulmonary exercise test
CS cancer survivors
cTn cardiac troponins
CTR-CVT cancer treatment related cardiovascular toxicity
CVD cardiovascular disease
ESC European Society of Cardiology
GLS global longitudinal strain
HFA Heart Failure Association of the ESC
LVEF left ventricular ejection fraction
ICOS International Cardio-Oncology Society
MDT multidisciplinary team
NP natriuretic peptide
NMR nuclear magnetic resonance
PAD peripheral artery diseases
RT radiotherapy
Take-home messages
- Specific recommendations apply to the long-term management of childhood and adolescent CS.
- Specific recommendations apply to the long-term management of asymptomatic adult CS.
- Specific recommendations apply to the management of symptomatic or asymptomatic CRT-CVT after the conclusion of cancer therapy.
Patient-oriented messages
- If you are a childhood and adolescent CS, you may sometimes experience CTR-CVT many years after the end of therapy. A careful assessment of your cardiac health should be undertaken periodically to avoid the development of these complications.
- If you are an adult asymptomatic CS, a CTR-CVT may theoretically occur in your future as well.
- If you developed a CTR-CVT during cancer therapy, there are treatments that can help restore your CV health, but you will need periodic testing to re-evaluate your conditions.
- To continue to be in good CV health you should follow a healthy lifestyle, including a healthy diet, regular physical activity, avoiding smoking, controlling your blood pressure and glycaemic and lipidic levels, and avoiding obesity.
Impact on practice statement
The risk assessment of CS allows us to select patient risk categories and to take decisions about their one year and long-term follow-up management.
Specific considerations should be kept in mind for the long-term follow-up of adult survivors of childhood and adolescent cancer, asymptomatic CS with or without development of a cardiovascular disease (CVD) during treatment, asymptomatic or symptomatic CS with new or persisting abnormalities at end-of-therapy assessment.
There are specific protocols for each class of patients, as regards to the timing and the tools used to evaluate the evolution or the development of a new CTR-CVT.
Moreover, many CTR-CVT induced by cancer treatments may have particular clinical presentations and entail difficult diagnostic challenges and therapy considerations. Sometimes these decisions should be submitted to and agreed upon by a multidisciplinary team (MDT).
1. Long-term follow-up
Long-term follow-up is oriented to two separate categories of CS: the adult CS of childhood and adolescent cancer and the adult CS, both asymptomatic and symptomatic, who may develop many different CTR-CVT.
1.1 Adult survivors of childhood and adolescent cancer
In recent years, children and adolescent CS have experienced a dramatic increase in 5-year survival that exceeding 80%.
Left ventricular (LV) dysfunction, valvular heart diseases, coronary artery disease (CAD), arrhythmias, autonomic dysfunction, pericardial disease, and premature cardiovascular (CV) mortality are all possible late outcomes in this population, particularly affecting those exposed to anthracyclines, mitoxantrone, and chest radiotherapy (RT), alone or in combination.
LV dysfunction is the most frequent late effect in childhood CS leading to morbidity and non-cancer related mortality in adulthood. A large cohort from the Childhood Cancer Survivor Study showed a cumulative incidence of 4.8% of heart failure (HF) by the age of 45 [1].
In 2015, the International Late Effects of Childhood Cancer Guideline Harmonization Group [2] published the criteria for an in-depth evaluation of paediatric CS. The risk stratification is based upon the total cumulative dose of anthracycline and total RT dose, including the heart region, and is divided as follows:
- At very high risk:
- A total cumulative doxorubicin >400 mg/m2
- A RT >25 Gy mean heart dose (MHD)
- A combination of RT >15 Gy and total cumulative doxorubicin ≥100 mg/m2
- At high risk:
- A total cumulative doxorubicin ≥250 mg/m2
- A RT >15 Gy MHD
- A combination of RT ≥5–15 Gy MHD and total cumulative doxorubicin ≥100 mg/m2
- At moderate risk:
- A RT ≥5–15 Gy MHD
- A total cumulative doxorubicin 100–249 mg/m2
- A combination of RT <5 Gy MHD and total cumulative doxorubicin ≥100 mg/m2
- At low risk:
- RT <5 Gy MHD, no anthracycline
- A total cumulative doxorubicin <100 mg/m2
In high-risk survivors, a CV review and an echocardiogram every 2 years with lifelong surveillance is strongly recommended, while for moderate risk, a review every 5 years is considered sufficient and always with an echocardiographic assessment.
In any case, all childhood CS, especially those treated with anthracyclines, mitoxantrone, or RT alone or in combination, should be informed of their increased CV risk, should review their common CV risk factors annually and optimise their lifestyle.
Considering that many females CS of childhood and adolescent cancers may want to become pregnant, a careful CV evaluation is recommended prior to or in the first trimester of a pregnancy.
1.2 Asymptomatic adult cancer survivors
Although there has been great progress in cancer-free survival over the last decades, many CS may develop late side effects, including CTR-CVT and particularly LV dysfunction. In some cancer survivors, CV mortality exceeds cancer mortality and deeply affect the quality of life. Anthracycline administration and RT with the heart included in the radiation field have the highest risk. Notably, radiation CV damages begin to occur 5–10 years after exposure.
As a consequence, all CS should receive a CV risk assessment at the end of therapy and those identified as at high risk need lifelong surveillance.
The risk categories for asymptomatic adult CS may be summarised as follows:
- At very high risk:
- CS with a baseline very high CV toxicity risk
- CS treated with a ≥400 mg/m² doxorubicin
- CS treated with RT ≥25 Gy MHD
- CS treated with RT ≥15-25 Gy MHD and ≥100 mg/m² doxorubicin
- At early high risk (the first 5 years after therapy):
- CS with a baseline high CV toxicity risk
- Symptomatic or asymptomatic moderate to severe CTR-CVT during treatment
- CS treated with 250–399 mg/m² doxorubicin
- High risk haematopoietic stem cell transplantation
- At late high risk (over 30 years from therapy):
- CS treated with RT ≥ 15–25 Gy MHD
- CS treated with RT of 5–15 Gy MHD and doxorubicin dose > 100 mg/m²
- CS with poorly controlled CV risk factors
- At moderate risk:
- CS with baseline moderate CV toxicity risk
- CS treated with > 100–249 mg/m² doxorubicin
- CS treated with RT ≥ 5–15 Gy MHD
- CS treated with RT <5 Gy MHD and doxorubicin > 100 mg/m²
- At low risk:
- CS with baseline low CV toxicity risk and a normal end of therapy cardiac assessment
- Mild LV dysfunction during therapy but recovered by the end of cancer therapy
- RT <5 Gy MHD
- Doxorubicin < 100 mg/m²
The long-term surveillance program should be based on this assessment and carried out in collaboration with primary care physicians. For all risk categories, every patient should receive education on lifestyle measures and on CV risk factor optimisations based on an annual check-up. Possible symptoms of a CTR-CVT have to be searched for carefully, especially for CS submitted to anthracycline, RT involving the heart, and survivors of bone marrow transplants.
CS at high or very high early risk, particularly in the first 2 years, should undergo an electrocardiogram (ECG), natriuretic peptide (NP) measurement and an echocardiogram at 1, 3 and 5 years and every 5 years thereafter.
In asymptomatic CS with late high CTR-CVT risk, if the end of therapy evaluation is normal, an annual CV assessment with ECG and NP measurement is recommended starting at 5 years. An echocardiogram, a non-invasive screening for CAD and a carotid ultrasound should be undertaken every 5 years.
Although less stringent, asymptomatic CS at moderate risk of future CTR-CVT with a normal end of therapy CV assessment should receive a clinical assessment with ECG, echocardiography, and NP measurement every 5 years.
Figure 1 summarises the long-term protocol for surveillance in CS.
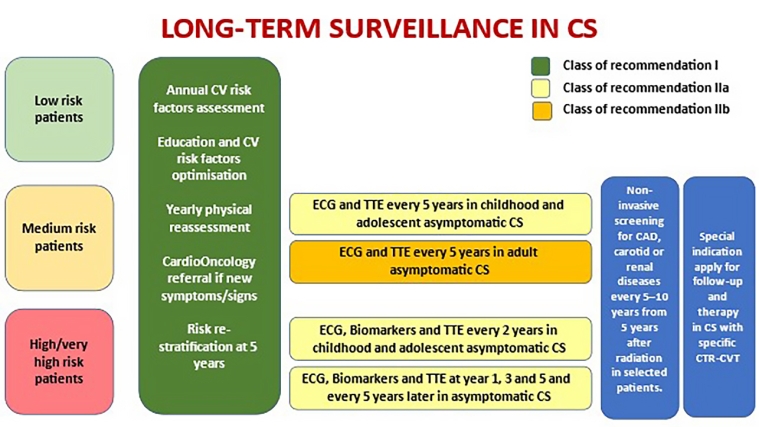
Figure 1. Long-term surveillance protocol
2. CTR-CVT Conditions in symptomatic and asymptomatic patients
2.1 Myocardial dysfunction and heart failure
Adult low baseline risk CS who received a high total cumulative anthracycline dose or high radiation doses to the chest have a progressive risk of cardiac dysfunction and HF over 20–30 years [3] which generally manifest 5–10 years after the end of treatment. Heart failure in CS has a six-fold higher incidence than in the general population and the increased CV risk from RT has been shown for Hodgkin lymphoma, non-Hodgkin lymphoma, breast cancer, and lung cancer [4].
The prognosis beyond 10 years of LV dysfunction from trastuzumab and other TKIs without elevation of cTn, with a complete recovery of LV function, a normal end of therapy assessment and a weaning off CV medication, is unknown.
Both symptomatic and asymptomatic CS who have LVEF <50% should continue angiotensin-converting enzyme (ACE) inhibitors/angiotensin receptor blockers (ARB) and/or beta-blocker treatment as part of the long-term follow-up, while these medications are also suggested for CS with mild asymptomatic LV dysfunction (LVEF >50% but with a new fall in global longitudinal strain [GLS] or NP increase).
2.2 Coronary artery disease
RT to the chest increases the risk of accelerated atherosclerosis in every vascular structure but mainly in the coronary artery. CV risk factors, particularly smoking and concurrent metabolic risk factors, pre-existing atherosclerosis, the age of the patient at the time of RT, RT doses and volumes and the type of radiation source, all influence the duration of the latency of the occurrence of clinical CAD as well as its severity. The proximal left anterior descending or the right coronary artery are the most commonly affected vessels, showing a severe diffuse pattern at angiography.
Balloon angioplasty or percutaneous coronary intervention (PCI) with bare metal stents (BMS) seem to have an increased risk of all-cause and CV mortality. PCI with drug-eluting stents (DES) seems to have results similar to those obtained in patients without prior chest RT. Interventional revascularisation seems preferable over coronary artery bypass grafts (CABG) in CS with severe left main or three-vessel disease, with a high SYNTAX score (>22).
Surgical revascularisation after RT entails possible injury to the left and right internal mammary arteries, small size and fibrotic native coronary vessels, due to poor skin and sternum healing and increased sternotomy pain, requiring a careful pre-operative evaluation.
The clinical presentation of RT-induced CAD may be sudden death. Infrequently, patients with severe diseases present with angina due to a higher pain threshold caused by the chest denervation after radiation damage.
The screening for CAD in high-risk asymptomatic patients should begin at 5 years post RT, and at 2 years with functional imaging in high-risk groups (known CAD or age >60 years and ≥1 CV risk factors).
The management of asymptomatic patients with inducible ischaemia should be discussed by the MDT to decide on the revascularisation options available according to the anatomic conditions, ischaemia burden, LV function, arrhythmia, time since treatment and previous normal review, risks of surgical or percutaneous revascularisation and eventually, the option of medical therapy.
The evolution of RT-induced CAD is unpredictable and can sometimes accelerate rapidly.
Also, platinum-based chemotherapies have been shown to cause CAD in CS. Testicular CS treated with a platinum-based chemotherapy are the most exposed to this condition and should be educated to promptly report any new chest pain or cardiac symptoms.
Prevention of CAD in CS is based on aggressive risk factor control and on a tight CV diagnostic follow-up, while aspirin and statins are recommended for primary/secondary prevention and beta-blockers and nitrates for symptom control.
2.3 Valvular heart disease
Valvular heart diseases (VHD) in CS who have undergone RT involving the heart generally appear >10 years after treatment. Calcific lesions may affect aortic and mitral valves leading to stenosis and/or regurgitation, with an incidence up to 40% and with <10% presenting with clinically significant VHD [5].
Prognosis and management are not different from the non-cancer patient population. Management is based on the severity of the disease and on symptoms. Common surgical risk calculators such as the Society of Thoracic Surgeons–Predicted Risk of Mortality (STS-PROM) or the European System for Cardiac Operative Risk Evaluation (EuroSCORE) II may underestimate the true risk in CS because several technical surgical and post-surgery complications are possible after irradiation, such as pericardial calcification, aortic calcification, impaired skin healing, and wound infections. So, transcatheter aortic valve implantation (TAVI) or similar strategies such as percutaneous mitral valve repair or replacement may be the preferred treatment. The patient’s choice and an MDT discussion should lead to the best shared management decision.
2.4 Peripheral artery disease and cerebrovascular disease
Chemotherapies with cisplatin, BCR-ABL inhibitors, and RT have a direct long-lasting effect on the vasculature. A previous peripheral arterial or cerebrovascular disease in CS may be accelerated by these treatments. Moreover, new vascular diseases that occur during, or after cancer therapy may be induced and generally become clinically evident within 2–4 years after the start of therapy.
Notably, head/neck radiation may induce significant carotid artery stenoses (>70%) in up to 30% of patients, which may lead to ischaemic stroke [6].
The effects of CV-related factors are additive to the direct treatment-related effects and their optimal control is recommended.
2.5 Pericardial complications
Some cancer therapies (anthracyclines, cyclophosphamide, cytarabine, bleomycin) may induce acute pericarditis but in the long-term the risk of evolution is low. Dasatinib treatment may lead to pericardial effusion and pericarditis, while long-term immune checkpoint inhibitor (ICI)-associated pericarditis is rare.
Although the risk is reduced with modern radiation procedures, a high rate of pericardial effusion persists in lung and oesophageal CS.
RT-induced chronic pericardial diseases like constrictive pericarditis can appear decades after RT, but their incidence is difficult to determine, as they are frequently asymptomatic. A 5-year echocardiography in CS following RT-induced acute pericarditis is ideal.
2.6 Arrhythmias and autonomic dysfunction
Supraventricular and ventricular arrhythmias, atrial fibrillation (AF) and atrial flutter, conduction diseases (AV block, bundle branch block, and sick sinus syndrome) and autonomic disease are common complications in CS. They are generally caused by RT or anthracyclines and are associated to other CTR-CVT.
Autonomic dysfunction with orthostatic hypotension, postural orthostatic tachycardia syndrome, inappropriate sinus tachycardia, and loss of circadian heart rate variability can occur after chest RT.
2.7 Obesity, hypertension, dyslipidaemia, diabetes, metabolic syndrome
All these CV risk factors may also be involved in cancer development and progression but are generally underestimated in cancer populations and undertreated. This applies particularly to patients who are obese at cancer diagnosis as some anticancer treatments may lead to further weight gain.
Intentional weight loss and diet post-treatment may improve CS prognosis and survival. A diet with a high intake of vegetables, fruits and whole grains is associated with reduced mortality, cancer recurrence and CTR-CVT.
Physical exercise during and after anticancer treatment, particularly aerobic exercise, improves survival and CS should exercise at least 150 minutes per week.
Aggressive treatment of hyperlipidaemia and possibly also of hypertension in CS seems to lead to a reduction in all-cause mortality and cancer recurrence.
2.8 Pulmonary hypertension
Pulmonary hypertension (PH), defined as an increase in mean PAP ≥20 mmHg during right heart catheterisation, may develop during dasatinib but is usually reversible after interruption. Other rare causes of pulmonary hypertension have been described (cyclophosphamide and other alkylating agents through a pulmonary veno-occlusive disease and other conditions related to enhanced risk of thromboembolic complications through chronic thromboembolic pulmonary disease). Postcapillary PH, due to left heart disease or with multifactorial mechanisms, may also occur in CS with cancer treatment-related cardiac dysfunction.
Patients who develop PH during therapy should undergo long-term surveillance. New exertional dyspnoea, fatigue, or angina, require the exclusion of pulmonary hypertension, and eventually a cardiology assessment of the aetiology and a right heart catheterisation.
2.9 Pregnancy
Many female paediatric and adolescent CS may have a pregnancy years after cancer treatment. Approximately 60% have been exposed to anthracycline and/or chest RT and have a 15-fold increase of HF, so the impact of cancer treatment on fertility, pregnancy outcomes, and CV health should be evaluated. The overall incidence of LV dysfunction or HF during pregnancy in adult CS ranges between 0–7.8% [7]. In a recent meta-analysis, LV dysfunction or HF risk in CS treated with anthracyclines was 1.7% with no reported maternal cardiac deaths [8].
Although the risk of HF in CS without CTR-CVT seems low, a pregnant CS should be submitted to a careful surveillance managed in an MDT environment.
Note to editors
Author:
Riccardo Asteggiano MD, FESC, Adjunct professor
Department of Medicine and Surgery, University of Insubria, Varese, Italy;
LARC-Laboratorio Analisi e Ricerca Clinica, Turin, Italy
Address for correspondence:
Dr Riccardo Asteggiano, Via San Marino 11 a, 10134 Turin, Italy
Author disclosures:
The author has no conflicts of interest to declare with regards this article.
References
- Kremer LC, van Dalen EC, Offringa M, Voûte PA. Frequency and risk factors of anthracycline-induced clinical heart failure in children: a systematic review.Ann Oncol. 2002;13:503-12.
- Armenian SH, Hudson MM, Mulder RL, Chen MH, Constine LS, Dwyer M, Nathan PC, Tissing WJ, Shankar S, Sieswerda E, Skinner R, Steinberger J, van Dalen EC, van der Pal H, Wallace WH, Levitt G, Kremer LC; International Late Effects of Childhood Cancer Guideline Harmonization Group. Recommendations for cardiomyopathy surveillance for survivors of childhood cancer: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group.Lancet Oncol. 2015;16:e123-36.
- Banke A, Fosbøl EL, Ewertz M, Videbæk L, Dahl JS, Poulsen MK, Cold S, Jensen MB, Gislason GH, Schou M, Møller JE. Long-Term Risk of Heart Failure in Breast Cancer Patients After Adjuvant Chemotherapy With or Without Trastuzumab.JACC Heart Fail. 2019;7):217-24.
- Boyne DJ, Mickle AT, Brenner DR, Friedenreich CM, Cheung WY, Tang KL, Wilson TA, Lorenzetti DL, James MT, Ronksley PE, Rabi DM. Long-term risk of cardiovascular mortality in lymphoma survivors: A systematic review and meta-analysis.Cancer Med. 2018;7:4801-13.
- Lancellotti P, Nkomo VT, Badano LP, Bergler-Klein J, Bogaert J, Davin L, Cosyns B, Coucke P, Dulgheru R, Edvardsen T, Gaemperli O, Galderisi M, Griffin B, Heidenreich PA, Nieman K, Plana JC, Port SC, Scherrer-Crosbie M, Schwartz RG, Sebag IA, Voigt JU, Wann S, Yang PC; European Society of Cardiology Working Groups on Nuclear Cardiology and Cardiac Computed Tomography and Cardiovascular Magnetic Resonance; American Society of Nuclear Cardiology, Society for Cardiovascular Magnetic Resonance, and Society of Cardiovascular Computed Tomography. Expert consensus for multi-modality imaging evaluation of cardiovascular complications of radiotherapy in adults: a report from the European Association of Cardiovascular Imaging and the American Society of Echocardiography.J Am Soc Echocardiogr. 2013;26:1013-32.
- Carpenter DJ, Mowery YM, Broadwater G, Rodrigues A, Wisdom AJ, Dorth JA, Patel PR, Shortell CK, Clough R, Brizel DM. The risk of carotid stenosis in head and neck cancer patients after radiation therapy.Oral Oncol. 2018;80:9-15.
- Garcia-Pavia P, Kim Y, Restrepo-Cordoba MA, Lunde IG, Wakimoto H, Smith AM, Toepfer CN, Getz K, Gorham J, Patel P, Ito K, Willcox JA, Arany Z, Li J, Owens AT, Govind R, Nuñez B, Mazaika E, Bayes-Genis A, Walsh R, Finkelman B, Lupon J, Whiffin N, Serrano I, Midwinter W, Wilk A, Bardaji A, Ingold N, Buchan R, Tayal U, Pascual-Figal DA, de Marvao A, Ahmad M, Garcia-Pinilla JM, Pantazis A, Dominguez F, John Baksi A, O'Regan DP, Rosen SD, Prasad SK, Lara-Pezzi E, Provencio M, Lyon AR, Alonso-Pulpon L, Cook SA, DePalma SR, Barton PJR, Aplenc R, Seidman JG, Ky B, Ware JS, Seidman CE. Genetic Variants Associated With Cancer Therapy-Induced Cardiomyopathy.Circulation. 2019;140:31-41.
- Nolan M, Oikonomou EK, Silversides CK, Hines MR, Thompson KA, Campbell BA, Amir E, Maxwell C, Thavendiranathan P. Impact of Cancer Therapy-Related Cardiac Dysfunction on Risk of Heart Failure in Pregnancy.JACC CardioOncol. 2020;2:153-62.
















