AF and thromboembolic ischaemic stroke
Atrial fibrillation (AF), especially in subjects with particular anatomic and physiopathologic conditions, including a large left atrium (LA), auricular structure, low flux in LA, reduced positive longitudinal LA strain and positive longitudinal LA strain rate, high levels of pro-brain natriuretic peptide (BNP) or low levels of plasma dipeptidyl peptidase 7, increases the probability of the formation of intra-atrial thrombi. This may frequently move to the arterial circulation, especially in cerebral arteries, leading to their occlusion and subsequent cerebral infarction. It has been estimated that about one-third of ischaemic strokes depend on this mechanism. AF is frequently discovered only during the course of stroke and often has a subclinical course.
Subclinical paroxysmal AF
Clinically silent AF episodes (detected by various electrocardiogram [ECG] recorders) are as much as 12.1 times more frequent than symptomatic episodes [1].
Patients may not perceive any kind of symptoms during episodes of paroxysmal AF, or may experience slight symptoms, like weakness, mild reduction in tolerance of efforts, fatigue, shortness of breath, chest pain, and light-headedness, none of which leads to a suspicion of an arrhythmia.
Paroxysmal AF, whether it is asymptomatic or not, has been related to thromboembolic events with the same rate of occurrence as those of permanent and symptomatic AF.
CS and AF relationship
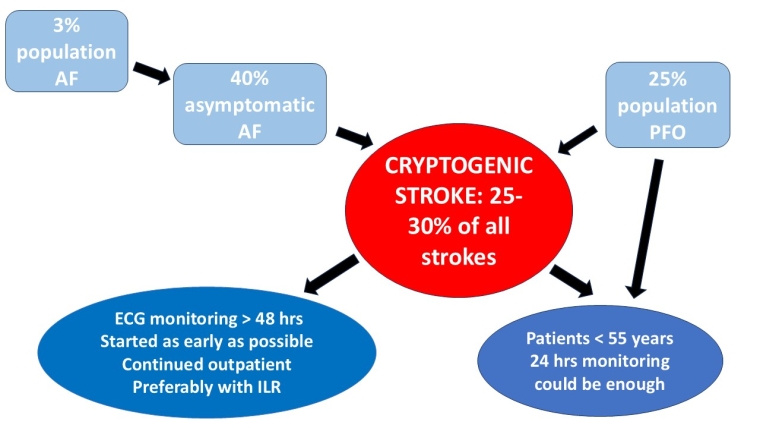
Cryptogenic stroke (CS; a stroke of undetermined origin), as defined by the TOAST classification, is a brain infarction not attributable to a clearly recognised cardioembolic event, carotid or intracranial artery disease, or other diseases after the appropriate vascular, cardiac, and serological investigations. CS is, as a consequence, suspected to result from a cryptogenic embolism, whose potential causes can include paroxysmal AF, patent foramen ovale, aortic arch atherosclerosis, and non-stenosing atherosclerosis of the carotid arteries.
It has been estimated that 26% of strokes are CS, with proportions ranging between 22% and 38% across the different races/ethnicities [2]. The risk of recurrent CS is 3% at 1 month [3] and rises to 14% after 2 years [4]
AF may cause CS when a paroxysmal subclinical AF is present, but a normal sinus rhythm spontaneously has resumed, before the thrombi mobilisation and/or the clinical expression of cerebral ischaemia. The probability that an episode of unknown paroxysmal AF is due to a cerebral thromboembolism of unknown origin is considerably high.
AF and CS diagnostic work-up
Clinical features of patients at risk of AF
Which patients with previous CS should be considered for AF screening?
Magnetic resonance (MR) brain imaging of multiple foci of restricted diffusion involving multiple and often bilateral vascular territories, are considered secondary to a cardiac thromboembolism, as undiagnosed asymptomatic AF. A substudy of the CRYSTAL-AF trial demonstrated that previous chronic brain infarctions and leukoaraiosis were associated with AF detection [5].
Estimates suggest an AF prevalence of approximately 3% in adults aged 20 years or older, with greater prevalence in high-risk AF patients, which includes those aged >65 years as well as patients with conditions such as hypertension, cardiac structural abnormalities, heart failure, coronary artery disease, valvular heart disease, obesity, diabetes mellitus, and chronic kidney disease. A complete evaluation should be undertaken in patients with these conditions, including a standard 12 lead ECG, and a complete blood sample with thyroid function.
Attention must be paid to look for the presence of interatrial block (IAB) with 12-lead ECG: a P-wave duration ≥120 ms identifies partial IAB, and biphasic P-wave morphology in inferior leads (II, III, aVF) indicates a complete block of Bachmann’s bundle (advanced IAB) [6]. IAB is an independent factor associated with AF, stroke, and cognitive impairment.
P-wave terminal force in V1, left atrial size on echocardiogram, and NT-proBNP are markers of atrial dysfunction that are associated with stroke, all independent of clinically apparent AF, and support the hypothesis that atrial cardiomyopathy may cause stroke even in the absence of AF.
For the general population, the European Society of Cardiology (ESC) guidelines [7] recommend:
- review of an ECG (12-lead, single, or multiple leads) by a physician to provide a definite diagnosis of AF and to commence appropriate management (Class I, Level of Evidence [LoE] B);
- routine heart rhythm assessment during healthcare contact in all individuals aged ≥65 years for earlier detection of AF (Class I, LoE C);
- population-based screening for AF using a prolonged non-invasive ECG-based approach should be considered in individuals aged ≥75 years, or ≥65 years with additional CHA2DS2-VASc risk factors to ensure earlier detection of AF (Class IIa, LoE B).
ECG screening
The electrocardiographic screening is the most useful, but also the most difficult, issue for diagnosing a subclinical AF. In patients with CS, the importance of detecting AF is greater, so the ESC guidelines [7] recommend prolonged monitoring to better inform the AF treatment decision (Class I, LoE B).
At present, six different non-invasive monitoring techniques are available [8]:
- The “classic” Holter monitoring, with the ability to record continuous 3- to 12-lead ECG signals during normal daily activities, can be helpful to characterise rhythm before arrhythmia onset. It can detect AF in only 3-5% of cryptogenic stroke. Wearing a vest/belt recorder for 30 days can improve AF detection to 21-30%.
- Patch ECG monitors allow long-term recording of 14 days or longer and some models offer wireless ECG transmission.
- External loop recorders analyse rhythms with 1 to 3 ECG leads and can store up to ten different arrhythmias, recording before, during and after the episode, either automatically or manually by the patient. Due to intermittent monitoring, they can work up to 1 month. Some of them may generate an immediate alarm upon event detection.
- Event recorders are generally simpler and less expensive devices that must be activated by the patient when a symptom occurs. They can generate an immediate alarm upon event detection. They can be worn for longer time but are not suitable to record asymptomatic arrhythmias.
- Multilead mobile cardiac telemetry may record pseudostandard, 3-lead ECG. These devices can stream data continuously to caregivers.
- Smart watches can be worn continuously by patients and have identified irregular rhythms in 0.5% of a large study population. To validate smart watch results, patients were subsequently monitored with an electrocardiogram patch which showed a positive predictive value for detecting AF of 0.84. Recently, a cardio tracker (CART) ring outperformed a smart watch for automated AF detection, with higher sensitivity (84.6% vs 69.1%) and significantly fewer unclassified ECGs (1.9% vs 20.1%).
In recent years, the diffusion of internal loop recorders (ILR) has been rapidly increasing as they can monitor patients for up to 3 years and their implantation is very easy.
The role of age
The role of age in AF prevalence is evident when comparing two large studies like CRYSTAL-AF [9] and EMBRACE [10]. In the former, 441 patients older than 40 years with ischaemic stroke were randomised to implant a loop recorder or to standard 24-hour monitoring. At 6 months, AF detection was 8.9% vs 1.4%, at 12 months 12.4% vs 2% and at 36 months 30% vs 3%, respectively. In the EMBRACE study, 552 patients with ischaemic stroke older than 55 years underwent 30 days of event-triggered monitoring or standard care. At 90-day follow-up, AF was detected in 16.1% in the intervention group versus 3.2% in the control group. The higher prevalence in a shorter period can be due to the patients mean age of 72.5 years in EMBRACE versus 61.6 years in CRYSTAL-AF.
The role of monitoring duration
While longer cardiac monitoring certainly increases the rate of subclinical AF detection, the optimal duration of monitoring is still a matter of debate. In the ASSERT trial, the median time to first AF episode was approximately 35 days after monitoring onset in patients implanted with a pacemaker or a defibrillator without previous stroke [11]. In the SMART Registry, the first episode was at an average of 11.4±8.6 days after initiation of monitoring in patients with recent CS [12]. During a 30-day monitoring period, 45% of AF episodes were recorded during the first 10 days, 36 in the middle 10, and 24% in the last 10 days. Only 6.1% of episodes were associated with symptoms.
The best time to start monitoring is also uncertain: as early as possible after ischaemic stroke or one month later? A higher yield might be obtained within the first weeks from stroke [ 13]. In FIND-AF [14], the first 10 days of monitoring detected 18 AF cases as compared to 6 cases during the 10-day monitoring at 3-month follow-up. However, a meta-analysis [15] indicated that the detection rate is identical with ILR implanted in the first month from the stroke or later. Only monitoring duration and mean patient age were independently associated with the proportion of AF detection.
However, the AF-stroke relationship is complex: a series of studies performed on patients implanted with an electronic device, with or without previous documented AF, found that ischaemic stroke may occur without the concurrent presence of atrial tachyarrhythmias or AF at the time of stroke or in the days before.
These studies also demonstrated that, even if AF episodes of very short duration (minutes to hours) are associated with stroke/systemic embolism, thromboembolic events may occur at temporal distance from AF. A meta-analysis [16] reported the temporal association between subclinical AF and stroke: in 181 patients with stroke, only 54% had atrial high-rate episodes (AHRE); these AHRE episodes preceded stroke in 56% of the cases, were at the time of stroke in 17% and after stroke in 27% of these cases. Up to 46% of this group of patients with stroke had no AHRE detected in their implanted device, enhancing the fact that it may be that many patients had strokes because of causes other than AF, or that the link between AHRE burden and stroke could be an epiphenomenon, that is, that patients with more AHRE may have more severe vascular risk factors. This is further supported by the ASSERT study [11], where an ILR, implanted in older asymptomatic patients with atrial enlargement and associated risk factors, detected subclinical AF in 34.4% of patients at 16-month follow up. The evidence that subclinical AF is so common in older patients with and without prior stroke could substantially weaken the causality link between subclinical AF and stroke.
What duration of AF increases stroke risk?
According to ASSERT [11], asymptomatic atrial tachyarrhythmias lasting more than 6 minutes recorded by a pacemaker or an implantable cardioverter defibrillator during a 3-month monitoring period were associated with a higher adjusted rate of stroke or systemic embolism. Additionally, an AF burden longer than 5 minutes was associated with a higher stroke risk, but it was not associated with an increase in all-cause mortality.
What the guidelines say
The ESC Guidelines for the management of AF have specific recommendations for screening, particularly in cases of subclinical arrhythmia, and are debated in the chapter about the diagnostic work-up. In the European Stroke Organisation (ESO) Guideline [17], published in 2022, some questions remain unanswered and require more evidence from randomised controlled trials, critical reviews and evaluations.
PICO (Population, Intervention, Comparison, and Outcome) questions have been developed to determine the effects of cardiac rhythm monitoring duration, setting (in-hospital vs outpatient), monitoring device type (implantable vs non-implantable) and according to patient phenotype (with and without a PFO).
What to do in daily clinical practice
ESO indications for AF screening in adult patients with ischaemic stroke or transient ischaemic attack (TIA) of undetermined origin are [17]:
- prolonged cardiac monitoring instead of standard 24 h monitoring is recommended to increase the detection of subclinical AF;
- the use of additional outpatient monitoring compared with in-hospital cardiac rhythm monitoring alone is suggested to increase the detection of subclinical AF;
- initiating ECG monitoring as early as possible during the in-hospital stay is suggested to increase the rate of AF detection;
- the use of implantable devices for cardiac monitoring instead of non-implantable devices is suggested to increase the detection of subclinical AF;
- there is continued uncertainty over the advantages of the use of blood, echocardiographic, ECG or heart or brain imaging biomarkers to increase the detection of subclinical AF;
- the presence of potential blood, echocardiographic, ECG or brain imaging biomarkers might increase the probability of AF detection but given the limited current evidence, it is suggested to avoid using these to exclude patients from long-term ECG monitoring.
In adult patients with ischaemic stroke or TIA of undetermined origin and PFO, there is continued uncertainty over the risks and benefits of the use of implantable monitor devices over any non-implantable external monitor devices to increase the detection of subclinical AF:
- prolonged cardiac rhythm monitoring for AF for more than 48 h in patients >55 years is suggested to increase the detection of subclinical AF;
- prolonged cardiac rhythm monitoring for AF to increase the rate of anticoagulation or reduce unnecessary PFO occluder implantations is suggested in patients with cryptogenic stroke and PFO in patients >55 years;
- using an implantable monitoring device, compared to any non-implantable external monitoring device, is suggested to detect paroxysmal AF in patients with cryptogenic stroke and PFO in patients >55 years.
- In patients younger than 55 years with undetermined stroke and PFO, basic cardiac monitoring for 24 h by telemetry or Holter-ECG could be enough to rule out subclinical AF, but clinical, stroke and PFO characteristics should be taken into account.
Impact on practice statement
CS may occur after an undiagnosed subclinical paroxysmal AF in a relevant percentage of patients (up to 30%).
One major issue in the prevention of CS recurrence is the clinical discovery that a primary episode of CS was a consequence of an asymptomatic AF does not present during the first clinical evaluation. Consequently, the screening for AF in patients with CS is key for their clinical management.
In particular, patients at risk for AF – patients older than 65 years with conditions such as hypertension, cardiac structural abnormalities, heart failure, coronary artery disease, valvular heart disease, obesity, diabetes mellitus, chronic kidney disease – should undergo a thorough clinical evaluation and ECG monitoring to unveil a subclinical AF.
The electrocardiography screening for AF may be difficult and the diagnosis probability is directly related to the duration of the ECG recording. Therefore, in selected cases of high suspicion for AF, the duration of the monitoring should be as prolonged as possible, including different methods, such as the implantation of an ILR.