Hot Line 1:report by Dr Riccardo Asteggiano (Turin, Italy)
Thirty years later, Digitalis is coming back!
DIGIT-HF trial (Professor Udo Bavendiek, Hannover Medical School, Hannover, Germany)
After theDigitalis Investigation Group (DIG) trial of 1997, the DIGIT-HF trial tested the effects of digitoxin on 1,212 patients (66 years, 20.4% women), most of them New York Heart Association (NYHA) class III or IV, who were randomly assigned to receive, on top of standard care, either digitoxin or a matching placebo. The mean left ventricular ejection fraction (LVEF) was 29%, and 27.2% of the patients had atrial fibrillation (AF). The median duration of treatment was 18 months with a median follow-up period of 36 months.
A primary-outcome event occurred in 242 patients (39.5%) in the digitoxin group and 264 (44.1%) in the placebo group (hazard ratio [HR] for death or first hospital admission: 0.82; 95% confidence interval [CI]: 0.69-0.98; p=0.03).
Less death from any cause occurred in the digitoxin group (167 patients: 27.2%) compared to placebo (177: 29.5%) (HR 0.86; 95% CI: 0.69-1.07; threshold for non-inferiority, 1.303; p<0.001).
At least one serious adverse event occurred in 29 patients (4.7%) in the digitoxin group and in 17 patients (2.8%) in the placebo group.
These findings appeared to be consistent among all pre-specified subgroups, including patients treated with angiotensin receptor-neprilysin inhibitors (ARNI) and sodium glucose cotransporter 2 inhibitors (SGLT2i), and treatment with digitoxin appeared to be safe.
Using a careful dose titration protocol, digitoxin may represent an additional option for patients with heart failure with reduced ejection fraction (HFrEF), particularly when guideline-recommended treatment cannot be tolerated.
Other trials:
The POTCAST trial (Speaker: Doctor Christian Jons, Rigshospitalet - Copenhagen University Hospital - Copenhagen, Denmark) tested a strategy of actively increasing plasma potassium levels to the high-normal range in 1,200 patients with automatic implantable cardioverter defibrillators (AICDs), at high risk of ventricular arrhythmias. Severe arrhythmias occurred in 22.7% of the participants in the high-normal potassium group, versus 29.2% of the participants in the standard-care group (HR 0.76; 95% CI: 0.61-0.95; p=0.01).
The AMALFI study (Speaker: Professor Louise Bowman, Oxford Population Health, Oxford, UK) showed a modest long-term increase in AF diagnosis during 2.5 years of screening with an electrocardiogram (ECG) patch monitoring for durations of 14 continuous days in over 5,000 older patients at moderate-to-high risk of stroke.
In the DOUBLE-CHOICE trial (Speaker: Professor Mohamed Abdel-Wahab, Heart Center Leipzig at Leipzig University, Leipzig, Germany), a “minimalist” (isolated local anaesthesia) was compared to a standard of care (SoC) approach in 752 patients submitted to transcatheter aortic valve implantation (TAVI). Similar results and non-inferiority were shown for the active group (primary endpoint: 22.9% in the minimalist group versus 25.8% in SoC).
Access the session here: HOT LINE 1 (content restricted to ESC Professional members)
Hot Line 2: report by Associate Professor Ruxandra Christodorescu (Timişoara, Romania)
Dapagliflozin under our expectations?
DAPA-ACT HF-TIMI 68 (Speaker: Professor David Berg, Brigham and Women's Hospital, Boston, MA, USA) tested early in-hospital initiation of dapagliflozin in 2,401 patients with acute heart failure (HF). At 60 days, there was no significant difference in the primary endpoint (cardiovascular [CV] death or worsening HF) between the active (10.9%) and the placebo group (12.7%): HR 0.86 (95% CI: 0.68-1.08; p=0.20).Safety was acceptable, with slightly more hypotension and renal events in the active group.
In-hospital initiation of dapagliflozin did not significantly reduce the risk of CV death or worsening HF through two months in hospitalised HF patients.
Note: this could result from a lower-than-anticipated event rate and the short duration of the study: indeed, a pooled analysis across SGLT2i trials suggests that in-hospital initiation of SGLT2i does reduce the high risk of adverse outcomes (CV death or worsening HF and all-cause mortality) in the early post-discharge period.
Efficacy of vericiguat in HF patients
Two presentationsevaluated the efficacy of vericiguat, an oral soluble guanylate cyclase stimulator, in heart failure patients with reduced ejection fraction (HFrEF).
VICTOR trial (Speaker: Professor Faiez Zannad (Université de Lorraine - Vandoeuvre-Les-Nancy, France).
In the VICTOR (Vericiguat Global Study in Participants with Chronic HF) trial, Prof. Zannad studied 6,105 stable, ambulatory HFrEF patients in a double-blind, placebo-controlled trial.
The drug failed to prove vericiguat superiority on the primary endpoint (CV death andand time to first hospitalisation): 18% versus 19.1%, HR 0.93 CI 0.83-1.04, p=0.20.
VICTORIA and VICTOR trials (Speaker: Professor Javed Butler Baylor Scott and White Research Institute, Dallas, TX, USA)
The pooled analysis of VICTOR and the previous VICTORIA trialwhich showed a reduction of CV death or HF hospitalisation by vericiguat (HR 0.90) in 5,050 patients at high risk of HFrEF [1]. This analysis assessed outcomes in 11,155 participants across the full spectrum of HFrEF and resulted in a reduction of the major primary points: hospitalisation for heart failure (HHF) or CV death (HR 0.91; 95% CI: 0.85–0.98 p=0.0088), HF hospitalisation: (HR 0.92; p=0.043) and all-cause mortality: (HR 0.90; p=0.025).
Benefits were consistent across age, sex, EF strata, and background therapies, including ARNIs and SGLT2 inhibitors. Patients with N-terminal pro-B-type natriuretic peptide (NT-proBNP) ≤6,000 pg/ml derived the clearest benefit. Safety was acceptable, with no excess hypotension, syncope, or renal events.
In conclusion, this pooled analysis supports vericiguat as an effective add-on therapy in HFrEF, both in high-risk and stable populations. The findings reinforce its role in comprehensive guideline-directed therapy, especially in patients with elevated but not extreme NT-proBNP levels.
Aficamten is superior to beta blockers in symptomatic obstructive hypertrophic cardiomyopathy (HCM).
The MAPLE-HCM trial (Speaker: Dr Pablo Garcia-Pavia, Hospital Universitario Puerta de Hierro Majadahonda, Majadahonda, Spain) compared aficamten, a cardiac myosin inhibitor, with metoprolol in 175 adults with symptomatic obstructive HCM over 24 weeks. Aficamten significantly improved exercise capacity (peak VO2 +1.1 mL/kg/min vs −1.2 with metoprolol; LSM difference 2.3 mL/kg/min; p<0.0001), NYHA class (51% ≥1 class improvement vs 26%; p<0.001), Kansas City Cardiomyopathy Questionnaire (KCCQ) score, NT-proBNP levels, and left ventricle outflow tract (LVOT) gradients. Left atrial volume decreased significantly; left ventricular (LV) mass was unchanged. Safety was favourable, with a mean LVEF decrease of 4% and only 1.1% experiencing LVEF <50%.
These results support aficamten as a superior alternative to beta blockers in symptomatic obstructive HCM.
Mavacamten: no effect in symptomatic non-obstructive cardiomyopathy.
The ODYSSEY-HCM trial (Speaker: Dr Milind Desai, Cleveland, OH, USA) of mavacamten in symptomatic non-obstructive cardiomyopathy enrolled 580 adults with symptomatic non-obstructive HCM (NYHA II–III). Over 48 weeks, mavacamten did not significantly improve the dual primary endpoints versus placebo: peak oxygen consumption (Δ 0.47 mL/kg/min; p=0.07) or KCCQ symptom score (Δ 2.7 points; p=0.06). Exploratory analyses revealed echocardiographic improvements in diastolic function and modest regression of LV hypertrophy.
Overall, mavacamten did not demonstrate clear benefits in non-obstructive HCM, underscoring a distinct pathophysiology and highlighting the need for tailored therapies in this subgroup.
REFERENCE
- Armstrong PW, Pieske B, Anstrom KJ, Ezekowitz J, Hernandez AF, Butler J, Lam CSP, Ponikowski P, Voors AA, Jia G, McNulty SE, Patel MJ, Roessig L, Koglin J, O'Connor CM; VICTORIA Study Group. Vericiguat in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med. 2020 May 14;382(20):1883-1893. doi: 10.1056/NEJMoa1915928. Epub 2020 Mar 28. PMID: 32222134.
Access the session here: HOT LINE 2 (content restricted to ESC Professional members)
Hot Line 3: report by Dr Dimitri Richter (Athens, Greece)
Beta blockers after myocardial infarction: stop or continue?
This is a pertinent debate, since the majority of our indications date from eras before contemporary reperfusion and modern medical therapy, and three communications addressed this question in patients with LVEF ≥40%.
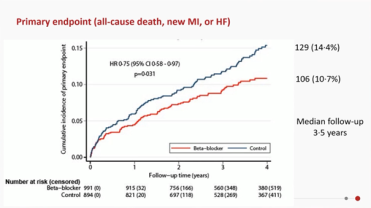
BETAMI and DANBLOCK [1] (Speaker: Dr Dan Atar, University of Oslo, Oslo, Norway)are two randomised controlled trials (RCTs) that were investigator-initiated in Norway and Denmark with almost identical design in a combined cohort of 5,574 myocardial infarction (MI) survivors, with LVEF ≥40% and no clinical heart failure (HF). Median follow-up was ~3.5 years.
The primary endpoint (composite of all-cause mortality, recurrent MI, unplanned revascularisation, ischaemic stroke, HF or malignant ventricular arrhythmias) was reached by the beta blocker (BB) arm (14.2% vs 16.3% in no-BB arm; HR=0.85; 95% CI: 0.75–0.98; p=0.027), with the key benefit driven especially by less new MI. All-cause mortality was not significantly different.
BBs reduce major adverse cardiovascular events (MACE) among MI survivors with LVEF >40%.
REBOOTCNIC [2] (Speaker:Dr Borja Ibañez, National Centre for Cardiovascular Research [CNIC] and Fundacion Jimenez Diaz Hospital, Madrid, Spain)is anRCT, investigator-initiated in Spain and Italy, including ~8,505 patients post-MI, treated invasively, with LVEF >40%, no history nor signs of HF, randomised to BB versus no BB before discharge. Median follow-up of ~3.7 years.
The primary endpoint rates: (composite of all‐cause death, non-fatal reinfarction, or HF hospitalisation) wereessentially the same in BB versus no-BB groups: 22.5 versus 21.7 per 1,000 patient-years. In the no-BB arm (HR 1.04; 95% CI: 0.89–1.22, p=0.63), without any benefit overall.
There wasno evidence of benefit across pre-specified subgroups.
Interestingly, women with LVEF ≥50% appeared to have worse outcomes if on beta blockers (HR ~1.52; 95% CI: 1.06–2.18) in that subgroup. This was a post hoc signal, so hypothesis-generating.
In uncomplicated MI patients with LVEF >40%, BB therapy did not significantly improve the primary endpoint.
REBOOT, BETAMI, DANBLOCK, and CAPITALRCT (Speaker: Professor Francisco Javier Rosselló Hospital Universitari Son Espases, Mallorca, Spain)
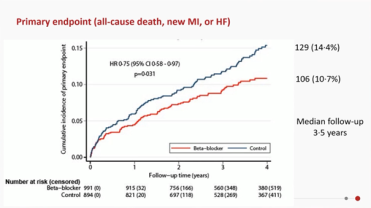
The session discussed an individual patient-level meta-analysis[3] across four trials: REBOOT, BETAMI, DANBLOCK, and CAPITALRCT including ~1,885 MI patients with mildly reduced LVEF (40–49%).The primary composite was all-cause death, new MI, or HF.
Results were in favour of the BB versus the no-BB arm, with an effect consistent across countries, and without significant heterogeneity: 10.7% vs 14.4%; HR=0.75; 95% CI: 0.58–0.97; p=0.031. All individual components (death, MI, HF) trended favourably though often with broader confidence intervals.
Post-MI patients with mildly reduced EF benefit from BB in terms of risk of death, MI, or HF.
Of course, these somewhat contradictory results generated debates and discussions, but the discussant, Professor John Cleland (University of Glasgow, Glasgow, UK) considered it possible, on present data, to stop BB use 6 to 12 weeks after MI, unless indicated for LV dysfunction, hypertension, arrythmias, or angina.
Implantable cardioverter defibrillator therapy does not improve survival in post-MI patients with mildly reduced LV function.
The REFINE ICD trial (Speaker: Professor Derek Exner, Libin Cardiovascular Institute of Alberta and University of Calgary, Calgary, Canada) evaluated the effect of implantable cardioverter-defibrillators (ICD) on survival in post-MI patients with 35-50% LVEF and, on the Holter registration,impaired heart rate turbulence and T-wave alternans. ICDs did not reduce mortality in this group compared to standard care alone. Interestingly, the abnormal electrocardiogram (ECG) markers did identify patients at a higher risk of death.
ICDs should not be used in the patient population investigated.
Figure 1. Beta blockers post-MI in patients with EF >40%.
REFERENCES
- Munkhaugen J, et al. N Engl J Med. 2025 Aug 30. doi: 10.1056/NEJMoa2505985. Epub ahead of print. PMID: 40888716.
- Ibanez B, et al. N Engl J Med. 2025 Aug 30. doi: 10.1056/NEJMoa2504735. Epub ahead of print. PMID: 40888702.
- Rossello X, et al. Lancet. 2025 Sep 13;406(10508):1128-37. doi: 10.1016/S0140-6736(25)01592-2. Epub 2025 Aug 30. PMID: 40897190.
Access the session here:HOT LINE 3(content restricted to ESC Professional members)
Hot Line 4: report by Dr Thomas Kümler (Herlev, Denmark)
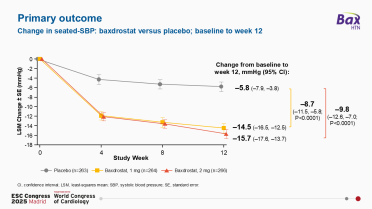
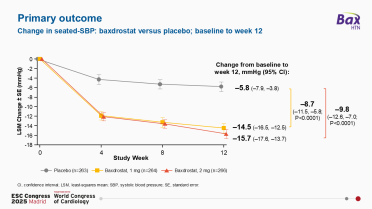
Baxdrostat (an aldosterone synthase inhibitor) lowers systolic blood pressure (SBP) in patients with uncontrolled or resistant hypertension.
BaxHTN (Speaker: Prof. Bryan Williams University College London, London, UK) is a multinational, double-blind, randomised, placebo-controlled trial recruiting non-controlled hypertensive patients (170 mmHg >SBP ≥140 mmHg despite two anti-hypertensive medications [uncontrolled hypertension] or three or more such medications [resistant hypertension], including a diuretic). Patients were randomly assigned 1 or 2 mg of baxdrostat or placebo in addition to background therapy. The primary endpoint was the change in seated SBP from baseline to week 12.
The changes from baseline in the least-squares mean seated SBP with 1 or 2 mg baxdrostat or placebo were respectively: −14.5 mmHg (95% CI: −16.5 to −12.5), −15.7 mmHg (95% CI: −17.6 to −13.7), and −5.8 mmHg (95% CI: −7.9 to −3.8). Baxdrostat was generally well tolerated, with a small increase in hyperkalaemia.
In the NEJM publication [1], “it was concluded that among patients with uncontrolled or resistant hypertension, the addition of baxdrostat to background therapy resulted in a significantly lower BP sys at 12 weeks compared to placebo.”
It would be interesting to check whether similar results could be obtained with spironolactone and to measure the effect of the drug on hard clinical endpoints.
Figure 2. Change in blood pressure in patients with uncontrolled or resistant hypertension.
Olezarsen reduces hypertriglyceridaemia in high cardiovascular risk patients.
Essence-TIMI 73b [2] (Speaker: Professor Brian Bergmark Brigham and Women’s Hospital, Boston, MA, USA), isa phase 3, international, double-blind, randomised, placebo-controlled trial, evaluating olezarsen, an N-acetylgalactosamine-conjugated antisense oligonucleotide that targets the messenger ribonucleic acid (RNA) of apolipoprotein C-III, which inhibits triglyceride clearance.
The trial included 1,349 patients with moderate hypertriglyceridaemia and elevated cardiovascular risk, randomised in 3 groups: olezarsen 50 mg, olezarsen 80 mg, and placebo.
Treatment with olezarsen resulted in a significantly greater reduction in triglyceride levels at 6 months than placebo. (−58.4%; 95 % CI: −65.1 to −51.7; p<0.001) for 50 mg, and −60.6% (95% CI: −67.1 to −54.0; p<0.001) for 80 mg.
The incidence of serious adverse events appeared to be similar across the trial groups.
In conclusion, a significantly greater reduction in triglyceride level at 6 months when compared to placebo is noted.
In addition, 2 other trials were presented in Hot Line 4:
- KARDIA-3: Zilebesiran as Add-on Therapy in Adults with Hypertension and Established Cardiovascular Disease or at High Cardiovascular Risk.
Speaker: Assistant Professor Neha Pagidipati, Duke Clinical Research Institute, Durham, NC, USA
- VICTORION-Difference study: Inclisiran-based strategy versus standard of care.
Speaker: Professor Ulf Landmesser, Deutsches Herzzentrum der Charité, Berlin, Germany
REFERENCES
- Flack JM, et al. N Engl J Med. 2025 Aug 30:10.1056/NEJMoa2507109. doi: 10.1056/NEJMoa2507109. Epub ahead of print. PMID: 40888730; PMCID: PMC7618089.
- Bergmark BA, et al. N Engl J Med. 2025 Aug 30. doi: 10.1056/NEJMoa2507227. Epub ahead of print. PMID: 40888739.
Access the session here: HOT LINE 4 (content restricted to ESC Professional members)
Hot Line 6:report by Professor Alexander Kharlamov (Heerhugowaard, the Netherlands)
Four trials — SWEDEPAD, PULSE, AQUATIC, and OPTION-STEMI — highlighted the fine balance between innovation, patient-centred outcomes, and clinical pragmatism in coronary and peripheral artery disease.
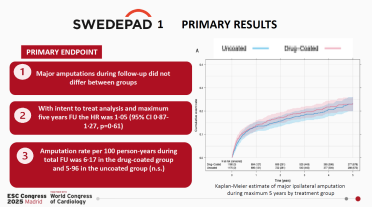
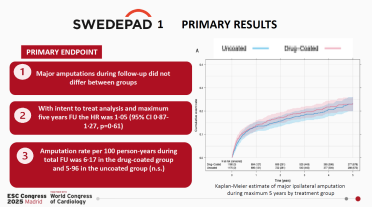
Caution with paclitaxel-coated stent use in peripheral artery disease.
SWEDEPAD 1 & 2 (Speaker: Professor Marten Falkenberg, Sahlgrenska University Hospital, University of Gothenburg, Gothenburg, Sweden) addressed the value of paclitaxel-coated balloons and stents in peripheral artery disease (PAD). Nearly 3,500 patients were randomised: 2,355 with chronic limb-threatening ischaemia (SWEDEPAD 1) and 1,136 with intermittent claudication (SWEDEPAD 2). In SWEDEPAD 1, major amputation occurred at similar rates with drug-coated versus uncoated devices (HR 1.05; 95% CI: 0.87–1.27; p=0.61). In SWEDEPAD 2, the one-year disease-specific quality of life score (VascuQoL-6) showed no difference (mean difference –0.02; 95% CI: –0.66 to 0.62; p=0.96). Alarmingly, five-year all-cause mortality was significantly higher in the drug-coated group (HR 1.47; 95% CI: 1.09–1.98; p=0.01), while reintervention rates were slightly reduced during the first year in chronic ischaemia (HR 0.81, p=0.03).
These devices do not improve limb outcomes or quality of life and may even jeopardise long-term survival in some patients.
Figure 3. SWEDEPAD 1 Primary results
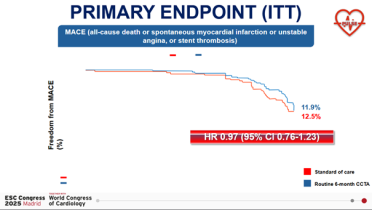
Routine CCTA after left main artery percutaneous coronary intervention: no benefit.
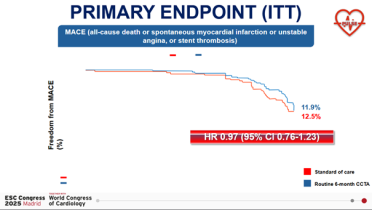
PULSE (Speaker: Dr Ovidio De Filippo, Hospital Citta della Salute e della Scienza di Torino, Turin, Italy), an international, randomised, open-label trial, compared routine six-month coronary computed tomography angiography (CCTA) after percutaneous coronary intervention (PCI) of the unprotected left main artery to standard care.
In 606 patients, routine CCTA did not reduce the 18-month composite endpoint of death, spontaneous myocardial infarction (MI), unstable angina, or stent thrombosis (MACE: 12.5% vs 11.9%; HR 0.97; 95% CI: 0.76–1.23). Yet, spontaneous MI was reduced more than fivefold (0.9% vs 4.9%; HR 0.24; 95% CI: 0.07–0.84; p=0.025). This benefit came at the cost of more revascularisations, many triggered by imaging alone (CCTA-driven target lesion revascularisation [TLR] 4.9% vs 0.3%; p=0.001).
Routine use of CCTA for all is not justified, even if the findings suggest selective benefit in anatomically complex cases.
Figure 4. PULSE
Do not continue aspirin longer than 6 months after PCI in anticoagulated patients!
In the AQUATIC trial (Speaker: Professor Martine Gilard, Hospital Cavale Blanche, Brest, France), 872 French patients on long-term oral anticoagulation (OAC) treatment with prior PCI (>6 months), and high risk of atherothrombotic events, were randomised to OAC plus aspirin or OAC plus placebo. After a median follow-up of 2.2 years, adding aspirin significantly worsened outcomes: the primary composite ischaemic endpoint occurred in 73 patients (16.9%) in the aspirin and in 52 (12.1%) in the placebo group (adjusted HR: 1.53, CI:1.07-2.18, p=0.02). Major bleeding tripled (HR 3.35; 95% CI: 1.87–6.00; p<0.001), and all-cause mortality rose by 72% (adjusted HR 1.72; 95% CI: 1.14–2.58; p=0.01). Enrolment was halted early for excessive rates of all-cause mortality.
In anticoagulated and stented patients, continuation of aspirin longer than 6 months is not only unnecessary but dangerous.
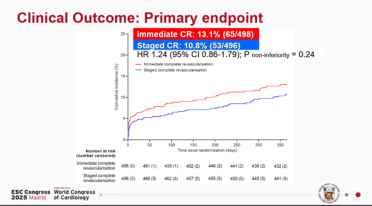
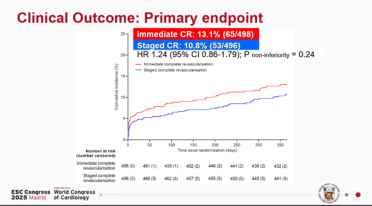
No advantage of immediate complete PCI revascularisation in STEMI patients.
The OPTION-STEMI trial (Speaker: Professor Youngkeun Ahn, Chonnam National University Hospital, Gwangju, South Korea) revisited the timing of complete revascularisation in STEMI with multivessel disease. In Korea, 994 patients were randomised to immediate versus staged in-hospital PCI. At one year, the primary composite outcome (death, non-fatal MI, or unplanned revascularisation) occurred in 13.1% vs 10.8%, failing to demonstrate non-inferiority (HR 1.24, 95% CI: 0.86–1.79; p for non-inferiority=0.24). Mortality was numerically higher in the immediate arm (7.5% vs 5.3%; HR 1.44; 95% CI: 0.87–2.38), and acute stent thrombosis was notably more frequent (8 cases vs 1).
“Fixing everything at once” is not always safe and supports staged revascularisation during the same admission.
Figure 5. OPTION-STEMI trial
Access the session here: HOT LINE 6 (content restricted to ESC Professional members)
Hot Line 8: report by Professor Diana Tint (Brasov, Romania)
May we stop anticoagulation after a successful catheter ablation in patients with atrial fibrillation and identifiable stroke risk factors?
The ALONE-AF trial (AnticoaguLation ONE Year After Ablation of Atrial Fibrillation) [1](Speaker: Professor Boyoung Joung, Yonsei University, Seoul, Republic of Korea) is a prospective, multicentre, open-label trial with blinded outcome assessment which sought to determine whether stopping oral anticoagulants (OACs) is safer and more beneficial than maintaining OACs in patients free of atrial arrhythmias for at least a year following successful ablation.
840 patients, with at least one risk factor, were randomised to either continue or discontinue OACs, with a follow up of two years; the primary outcomes included stroke, systemic embolism, major bleeding, mortality, quality of life, and frailty.
Events rate was lower in patients discontinuing OAC (0.3%) than in those that continued anticoagulation (2.2%): −1.9% (CI −3.5 to 0.3, p=0.02), and this was driven by a lower major bleeding rate, while ischaemic events (stroke, systemic embolism) were infrequent and similar in the two groups.
This significant benefit challenges the long-held belief of an indefinite anticoagulation after ablation: patients who maintain sustained sinus rhythm for at least 12 months post-ablation may be able to safely reduce or discontinue anticoagulant therapy. Ongoing studies [2,3] will help refine these strategies.
Which technique in AF catheter ablation?
The BEAT-PAROX-AF trial [2] (Speaker: Professor Pierre Jais, IHU Liryc, Bordeaux, France) executed across multiple European centres, compared pulsed field ablation (PFA) with the conventional point-by-point radiofrequency ablation (RFA) in patients with symptomatic, drug-resistant paroxysmal AF in 290 patients and focused on single-procedure success and safety profiles at 12 months. Both techniques demonstrated comparable efficacy rates (~77%), with some advantages for PFA (significantly shorter procedural durations, and fewer serious adverse events (i.e.,pulmonary vein stenosis and tamponades).
Should we personalise our AF ablation strategy?
The CUVIA-PRR trial [3, 4] trial(Speaker: Professor Joost Lumens, Cardiovascular Research Institute Maastricht [CARIM], Maastricht University, Maastricht, the Netherlands) is pioneering a digital twin-guided approach, aiming to customise ablation to each patient’s unique atrial substrate. Importantly, this approach did not prolong procedures or increase complication risks, highlighting the potential of precision medicine to enhance outcomes.
In conclusion, contemporary research indicates a paradigm shift towards more personalised, evidence-based management of AF. The insights from ALONE-AF and BEAT-PAROX-AF suggest that a patient-specific targeted approach may optimise clinical outcomes, reduce complications, and improve quality of life, heralding a new era in AF care.
References:
- Kim D, et al. JAMA. 2025 Aug 31:e2514679. doi: 10.1001/jama.2025.14679. Epub ahead of print. PMID: 40886309; PMCID: PMC12400166.
- Erhard N, et al. Europace. 2024 May 2;26(5):euae103. doi: 10.1093/europace/euae103. PMID: 38646926; PMCID: PMC11068269.
- Digital twin technology helps reduce the recurrence of atrial arrhythmias after catheter ablation for persistent atrial fibrillation. European Society of Cardiology. Press release. (Accessed September 7, 2025)
- Deisenhofer I, et al. Nat Med. 2025 Apr;31(4):1286-1293. doi: 10.1038/s41591-025-03517-w. Epub 2025 Feb 14. PMID: 39953289; PMCID: PMC12003177.
Access the session here: HOT LINE 8 (content restricted to ESC Professional members)
Hot Line 9: report by Dr Marc Ferrini (Lyon, France)
Should we screen for helicobacter in myocardial infarction patients?
The HELP-MI SWEDEHEART trial (Speaker: Associate Professor Robin Hofmann, Karolinska Institutet, Stockholm, Sweden) is a Swedish nationwide, open-label, 2-period with crossover, randomised, clinical trial using a clinical registry.
Among 18,466 patients with myocardial infarction, 9,245 were screened and 6,480 of them (70%) underwent testing for Helicobacter pylori. Of these 1,532 (23.6%) had positive results and received eradication therapy at the treating physician’s discretion. This group was compared with the “usual care” group of 9,221 patients. After a median follow-up of 1.9 years, 299 patients in the active and 336 in the usual care group experienced gastrointestinal bleeding, without significant difference. (RR 0.90; 95% CI: 0.77-1.05; p=0.18).
In unselected patients with acute myocardial infarction, routine Helicobacter pyloriscreening did not significantly reduce the risk of upper gastrointestinal bleeding and cannot be recommended.
Sacubitril with valsartan does better than enalapril in HF caused by Chagas disease.
The PARACHUTE-HF trial (Speaker: Professor Renato Delascio Lopes, Duke University School of Medicine, Durham, NC, USA) is a prospective, randomised, open-label, blinded, endpoint PROBE design in heart failure with reduced ejection fraction (HFrEF) caused by Chagas disease.
Sacubitril/valsartan was compared with enalapril in 922 patients (mean age: 64, mean LVEF: 29.8%; N-terminal pro-B-type natriuretic peptide (NT-proBNP): 1,730 pg/mL, NYHA Class II or III) randomised 1:1 in improving a hierarchical composite endpoint including CV death, first HF hospitalisation, and reduction in NT-proBNP at week 12. Sacubitril/valsartan was superior to enalapril (total wins [%]: 48.5% vs 31.6%; 95% CI: 1.52 [1.28-1.82]; p<0.001). These results were essentially driven by a reduction of 32% in the adjusted geometric mean of NT-proBNP levels at week 12 (22.5% vs 7.2%; HR 0.68; 95% CI: 0.62-0.75). Sacubitril/valsartan was well tolerated without any safety findings identified.
Note that this is the first randomised trial generating high-quality evidence to support a pharmacological treatment in this high-risk population of HFrEF caused by Chagas disease.
How to increase BP control in rural South African hypertensive patients?
The IMPACT BP trial (Speaker: Associate Professor Thomas Andrew Gaziano, Harvard T.H. Chan School of Public Health, Boston and Mass General Brigham, MA, USA) is an open-label, randomised, controlled trial of a home-based model of hypertension care in rural South Africa.
Adults with hypertension (n=774; 76% women; mean age 62 years), were assigned to receive home-based care with patient monitoring of blood pressure (BP), medication delivery, and remote nurse-led decision by a mobile application (community health worker [CHW] group); or enhanced home-based care, with added BP machines transmitting readings automatically (enhanced CHW group); or standard care management.
The mean systolic BP at 6 months was lower in the CHW group (–7.9 mmHg; p<0.001) and in the enhanced CHW group (−9.1 mmHg; p<0.001) than in the standard-care group. These results persisted at 12 months.
CHW-led home BP monitoring with remote nurse-guided dose titration and free home delivery of medicines resulted in substantial BP reduction at 6 months in rural South Africa.
Access the session here: HOT LINE 9 (content restricted to ESC Professional members)
Hot Line 10: report by Associate Professor Ruxandra Christodorescu (Timişoara, Romania)
Advances in cardiac surgery and surgical left atrial appendage occlusion (SLAAO)
Should we de-escalate DAPT in CABG patients?
The TOP-CABG trial (Speaker: Dr Xin Yuan, State Key Laboratory of Cardiovascular Disease, Fuwai Hospital, National Centre for Cardiovascular Diseases, Beijing, China) explored whether a de-escalation strategy could balance graft protection and bleeding in 2,290 first-time CABG patients. De-escalated DAPT (ticagrelor plus aspirin for 3 months, then aspirin alone for 9 months) was non-inferior to 12 months of DAPT for saphenous vein graft (SVG) occlusion at 1 year (10.8% vs 11.2%). Importantly, bleeding was significantly reduced with the de-escalated regimen (8.3% vs 13.2%; HR 0.62; p<0.001).
Shorter DAPT might become a safer option in future guidelines.
Evolocumab does not prevent early saphenous vein graft failure.
The NEWTON-CABG CardioLink-5 trial (Speaker: Professor Subodh Verma, St Michael’s Hospital, Toronto, Canada) tested whether evolocumab could prevent early SVG failure after CABG. In 782 patients on moderate-to-high-intensity statins, evolocumab achieved a 48% low-density lipoprotein cholesterol (LDL-C) reduction at 24 months but did not lower the rate of SVG occlusion compared with placebo (21.7% vs 19.7%; p=0.44).
Prof. Verma concluded that mechanisms beyond LDL-C, such as remodelling, thrombosis, or inflammation, likely drive early SVG disease, highlighting the need for novel strategies.
No advantage of DAPT over aspirin alone in CABG patients.
The TACSI trial (Speaker: Professor Anders Jeppsson, Sahlgrenska University Hospital, Gothenburg, Sweden) compared 12 months of dual antiplatelet therapy (DAPT; ticagrelor + aspirin) versus aspirin alone in 2,201 CABG patients with acute coronary syndrome (ACS). The primary composite outcome (death, MI, stroke, or new revascularisation) was similar between groups (4.8% vs. 4.6%; HR 1.09; p=0.77). However, major bleeding was more than twice as common with DAPT (4.9% vs. 2.0%; HR 2.50).
DAPT offers no cardiovascular advantage over aspirin alone and increases bleeding risk at 1 year after CABG.
No effect after 1 year of routine LA appendage occlusion during valve surgery.
The OPINION trial (Professor Yang Wang, State Key Laboratory of Cardiovascular Disease, Fuwai Hospital, National Centre for Cardiovascular Diseases, Beijing, China) assessed routine SLAAO in 2,118 high-risk patients undergoing valvular surgery without atrial fibrillation. At 1 year, the composite endpoint of stroke, transient ischaemic attack (TIA), or cardiovascular death was not significantly reduced with SLAAO versus control (6.9% vs 8.2%; HR 0.83; p=0.25), with no difference in bleeding.
Scheduled extended 3-year follow-up may clarify potential late benefits?
Access the session here: HOT LINE 10 (content restricted to ESC Professional members)