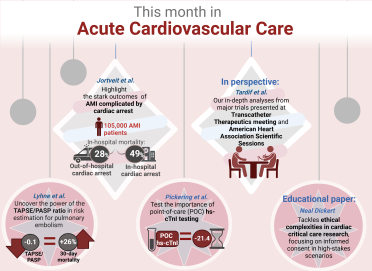
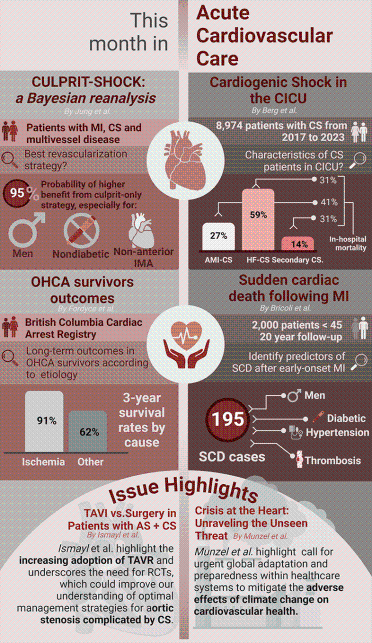
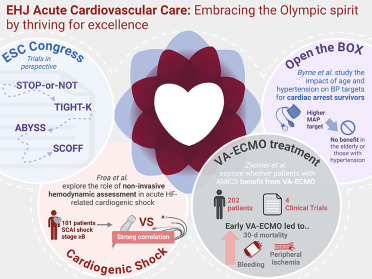
November 2024 Highlights
Welcome to the November issue of the European Heart Journal Acute Cardiovascular Care! As we transition into the final months of the year, the days may be getting shorter, but the warmth in our field remains as we shine a spotlight on groundbreaking developments in cardiovascular care. This month’s edition brings a fresh perspective to some of the most pressing challenges in acute cardiovascular care, from innovative treatments for electrical storm (ES) to novel insights into the microcirculation in cardiogenic shock (CS). With each study, we edge closer to improving patient outcomes in life-threatening scenarios.
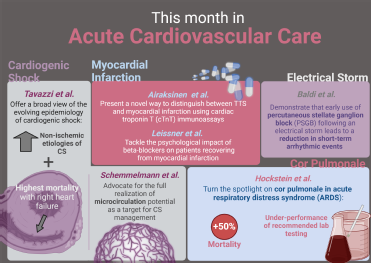
1. Enrico Baldi et al. demonstrated that the early use of percutaneous stellate ganglion block (PSGB) led to a dramatic reduction in arrhythmic events within the first hour, paving the way for safer, more effective interventions. PSGB offers new hope with potential to prevent progression to refractory ES—a breakthrough in an area where rapid intervention is critical. Although the study invites further exploration through randomized trials, the results are promising and may redefine how we approach ES in its early stage. Read more
2. Maxwell Hockstein et al. shed the light into often-underdiagnosed condition of cor pulmonale in acute respiratory distress syndrome (ARDS). Their analysis reveals that cor pulmonale is associated with a 50% higher mortality rate, emphasizing the need for early identification. By examining factors such as pulmonary artery pulsatility index and arterial elastance (Ea), the study highlights that traditional metrics, including pH and PaO2, are less reliable predictors. This work stresses the necessity for multimodal diagnostics to better understand right ventricular-pulmonary artery coupling and prevent complications in ARDS—a call for greater awareness and proactive management. Read more
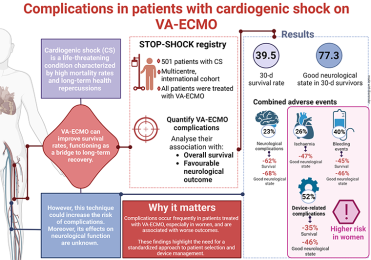
3. Guido Tavazzi et al. offer a broad view of the evolving epidemiology of CS, examining data from over 11 000 ICU admissions in Italy. Their study reveals a shift from the traditional ischaemic causes to non-ischaemic etiologies and that right heart failure portends the highest mortality risk among CS patients. This trend potentially highlights the importance of early recognition and tailored interventions. As CS remains a condition with mortality rates hovering near 50%, this study underscores the need for integrated, multidisciplinary care strategies to improve survival outcomes. Read more
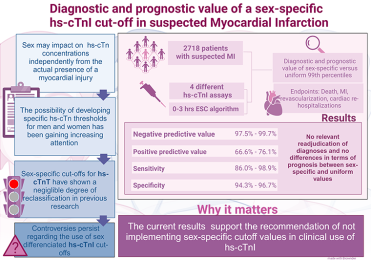
4. On the front of mental health Leissner et al. tackle an often-overlooked consequence of cardiac care: the psychological impact of beta-blockers on patients recovering from myocardial infarction (MI). Drawing from the REDUCE-AMI trial, the authors found that while beta-blockers are associated with an increase in depressive symptoms, anxiety levels remain largely unaffected. Although the rise in depressive symptoms was modest, this finding reminds us of the importance of considering the mental health implications when managing MI patients, especially in those with preserved left ventricular ejection fraction. As we deepen our understanding of the interplay between cardiovascular and mental health, this study highlights the need for a holistic approach to cardiovascular patient care. Read more
5. In a fascinating diagnostic advance, Juhani K.E. Airaksinen's study presents a novel way to distinguish between Takotsubo syndrome (TTS) and MI using cardiac troponin T (cTnT) immunoassays. The study’s discovery that TTS patients exhibit a significantly lower ratio of long to total cTnT compared to MI patients could offer a more precise diagnostic tool. While further research is needed to validate these findings with this investigational method, the potential for early differentiation between these two conditions could have a profound impact on treatment decisions, offering clinicians a powerful future tool in their diagnostic arsenal. Read more
6. Rounding out this month’s issue is our educational paper from Christian Jung et al.9, which advocates for a more nuanced approach to CS management. By shifting focus from macrocirculation to microcirculatory dysfunction, this paper makes a compelling case for integrating microcirculation assessments into clinical practice. The authors emphasize that while advances in microcirculation-guided therapies hold great promise, their full potential has yet to be realized. More research is needed to bridge the gap between theoretical benefits and practical application in the ICU setting. Read more
As we close this November issue, we invite our readers to engage with these pioneering studies, which collectively push the boundaries of cardiovascular care. We are excited about the discoveries shared in this edition, and we thank the authors for their invaluable contributions to our understanding of acute cardiovascular conditions. Together, let us continue to explore new horizons, expanding the possibilities of what can be achieved in the care of critically ill patients. Stay with us as we move into the final months of the year, energised, and optimistic about the future of our field.