Background
COVID-19 is synonymous with tumultuous challenges and changes in healthcare delivery, testing the resolve of specialist nurses and exhibiting their capacity for adaptability and creativity. The importance of recognition and response to the needs of heart failure (HF) patients are reflected in the aims of care, namely, improving quality of life (QoL) and reducing hospital admissions for this vulnerable patient group (ESC, 2021, Health Service Executive, 2012). HF disease management programmes are traditionally face-to-face consultations, providing lifestyle education and psychological support to patients and their families, alongside initiation and titration of optimal medical therapy (Ponikowski et al., 2016).
However, owing to the COVID-19 pandemic, restrictions were placed on face-to-face contact with patients with heart failure to minimise the risk of COVID-19 transmission. As such, HF nurses throughout Ireland needed to rapidly adapt to providing the majority of HF care remotely, via telemedicine. International studies have found significant improvements in mortality and hospitalisation, in select cohorts of HF patients, enrolled in telemonitoring programmes (Kotb et al., 2015, Inglis et al., 2017, Kruse et al., 2017). Subsequently, recent heart failure clinical guidelines suggest using telemonitoring as an adjunct to multidisciplinary HF disease management programmes (Ponikowski et al., 2016). However, telemonitoring is still in its infancy in Ireland with infrastructure only starting to develop. The outcomes of patients within Ireland using telemedicine as a platform of care is unknown. United by a collective motivation to reduce avoidable hospital admissions, heart failure nurses in 34 centres in Ireland considered a number of solutions to provide HF services remotely during the COVID-19 pandemic. An initiative developed in Beaumont Hospital was adopted as a standardised approach whereby HF patients were provided with home blood pressure monitors to augment telemedicine/virtual consults.
The Irish Association of Heart Failure Nurses (IAHF Nurses) are a subgroup of the Irish Nurses Cardiovascular Association (INCA). Forming part of the INCA mission statement is to build national collaboration and to promote excellence in nursing through education, research and leadership. The IAHF Nurses have truly embraced that mission statement. The strong collaboration between its over 60 members came to the forefront during the pandemic crisis.
The IAHF Nurses were eager to determine the impact of telemedicine on patient outcomes during the COVID-19 pandemic in Ireland. Against a context of mass re-deployment of specialist nurses to frontline clinical practice to bolster diminishing staffing, a retrospective review of electronic care records, HF databases and discharge summaries, was conducted in September 2020 in ten healthcare settings across Ireland. A standardised proforma was used to collect data over 14 days (last week of May-first week of June) in 2019 and 2020.
Adult patients with HF, >18 years who attended outpatient HF services, were eligible and included in the review. Variables included HF service activity, hospitalisation, admission avoidance and drug titrations. Data were analysed using SPSS with descriptive analysis employed to provide quantitative summaries and describe the changes in variables over time.
Results
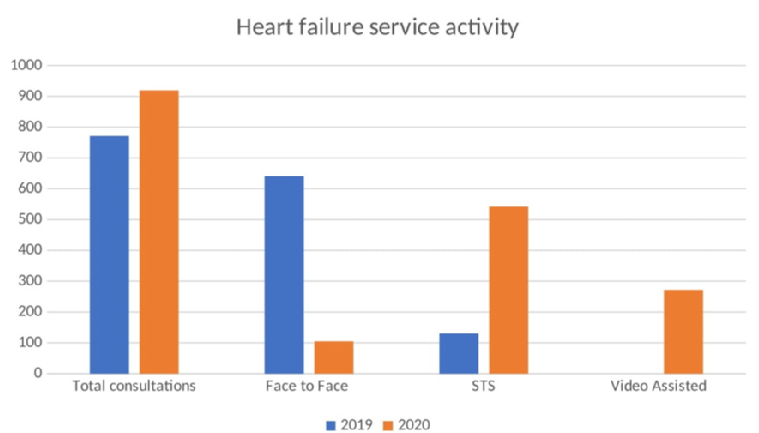
Face-to-face consultations decreased by 83% in 2020, with a shift to the use of telemedicine for managing patients with HF, which included structured telephone support (STS) and/or the use of video-assisted technologies (Figure 1). The use of remote management, alongside face-to-face reviews, when required, facilitated a 19.2% increase in the number of patient consultations undertaken in 2020 compared to the same period in 2019. Over one-third of these consultations in 2020 (n= 329, 36%) resulted in a change to patient’s medications, in response to a change in the patients' clinical status. 191 consultations focused on direct admission avoidance due to clinical deterioration for community-dwelling HF patients. A further 34.4% (n=316) of these consultations did not result in the titration of disease-modifying therapies for HFrEF patients. HF hospitalisations via the emergency department for patients enrolled in these HF services with acute presentations increased by 11.5% compared to 2019, while elective admissions for patients enrolled in HF services fell by 80%.
Conclusion(s)
This review provides valuable insight into the utility of remote monitoring during the lockdown due to the COVID‐19 pandemic in Ireland. Utilising STS and/or video-assisted technologies, alongside face-to-face consultations, where required, HF nurses in Ireland were able to provide continuous monitoring. As a result, several hospitalisations due to deteriorating clinical status were avoided. However, proactive titration of disease-modifying therapies for HFrEF patients via remote monitoring platforms was largely paused. Urgent development of protocols and strategies to ensure optimisation of evidence-based therapies using telemedicine/AI platforms is required.
There is growing awareness of a possible increase in the need for service capacity post-COVID-19 era. Therefore, establishing evidence-based best practices to allow for optimisation of disease-modifying agents via telephone and virtual visits should be a priority for heart failure services in Ireland going forward. The value of harnessing the collective knowledge, capability and creativity of specialist nurses through the lens of national (INCA) and European (ACNAP) societies should not be underestimated as a powerful vector of change.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.