We report a case of a 58-year-old woman with known hypertrophic cardiomyopathy (HCM) and left ventricular outflow tract obstruction (LVOTO) (40 mmHg peak gradient) with mild symptoms (NYHA functional class II/IV) with beta blockers and disopyramide. The patient was admitted in the intensive care unit (ICU) for acute heart failure and respiratory sepsis. The patient required prolonged mechanical ventilation and vasoactive drugs. After three days of treatment in the ICU without improvement, and considering the existence of a significant LVOTO, we decided to perform an urgent alcohol septal ablation with a significant and stable resolution of the obstruction during admission. The clinical course was complicated by auriculo-ventricular block. Finally, the patient was discharged in a good clinical situation.
Patient presentation and initial workup
A 58-year-old woman with a medical history of paranoid schizophrenia, type-2 diabetes mellitus and known obstructive hypertrophic cardiomyopathy (HCM) was admitted to ICU due to acute heart failure and a respiratory infection. The patient was previously in good clinical status presenting a left ventricular outflow tract obstruction (LVOTO) (peak gradient of 40 mmHg) but with mild symptoms (NYHA functional class II/IV) under bisoprolol 5mg bid and disopyramide 100mg bid.
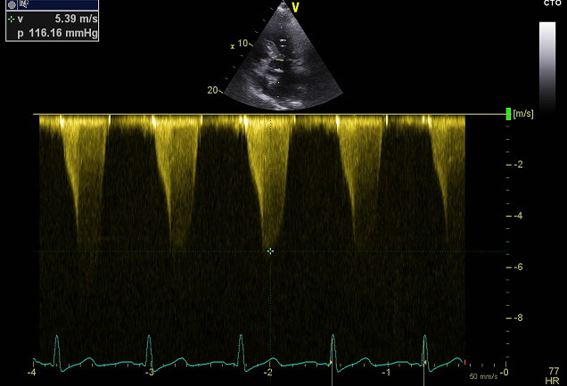
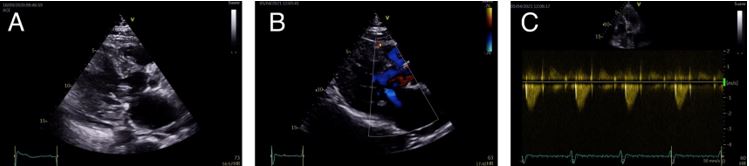
The patient was admitted to the emergency department with acute heart failure with clinical worsening during the last two days. In addition, she presented with cough, expectoration and fever up to 39ºC. An echocardiogramme on arrival confirmed the known asymmetric hypertrophy of the basal interventricular septum (18 mm), and a severe worsening of the left ventricular outflow tract obstruction (120 mmHg) together with SAM and moderate to severe mitral regurgitation (Figure 1)
The patient presented a rapid deterioration with marked haemodynamic instability, requiring intubation and mechanical ventilation and vasopressor agents (norepinephrine). At the admission to the ICU the patient was hypotensive (systolic arterial pressure 80 mmHg), with sinus tachycardia (105 bpm), bilateral pleural effusion, cold extremities, and profuse sweating.
Most people with HCM are asymptomatic and have a normal lifespan but symptoms of chronic heart failure are frequent. In most patients, there is a life-long process of progressive and adverse cardiac remodelling, characterised by myocardial fibrosis and wall thinning. Presentation with acute heart failure is uncommon, but this can be precipitated by arrhythmias (atrial fibrillation or ventricular sustained ventricular tachycardia, acute mitral regurgitation (infective endocarditis), acute coronary syndrome, or infectious disease (e.g. septic shock).
Management
Empiric broad-spectrum antibiotic therapy was administered. Furthermore, intravenous (i.v.) esmolol was given to reduce LVOTO and heart rate and we continued i.v. noradrenaline in order to increase afterload and reduce the relative LVOTO. It was also assessed that the pleural effusion could be significantly conditioning the patient's respiratory distress, and it was finally decided to perform a drainage procedure.
After initial stability during the first three days, the main complication was the difficulty in ventilatory and vasoactive weaning due to severe LVOTO. The patient continued to require high doses of norepinephrine (25ml/h) and mechanical ventilation, in addition to progressive renal failure. However, there was a marked improvement in acute-phase reactants indicating a favourable evolution of the infective condition.
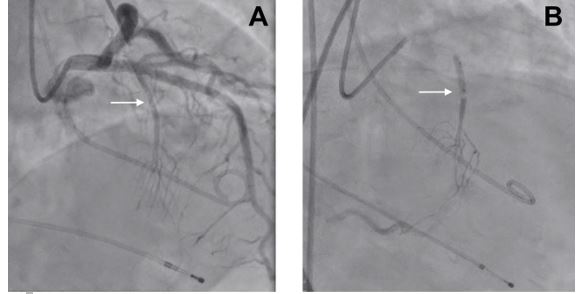
After a discussion of the case, the heart team decided to implant a transient pacemaker and perform an urgent alcohol septal ablation (ASA). The transient pacemaker was implanted in order to reduce LVOT gradients and in preparation for ASA. ASA relieves LVOTO by creating a localised myocardial infarction in the area of the basal septal muscle where SAM-septal contact is occurring. Following remodelling of this area, the LVOT is widened, thereby relieving LVOT obstruction. Previous clinical cases in the literature have shown a rapid gradient resolution and long-term improvement with ASA.
Follow-up
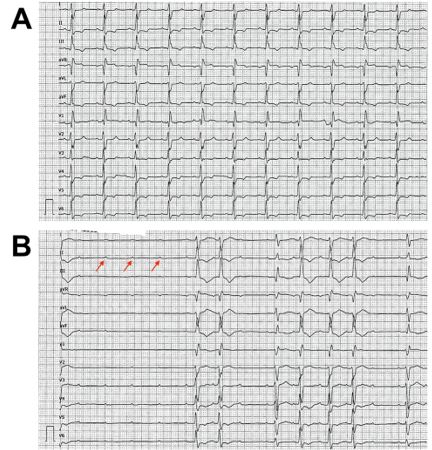
Alcohol septal ablation was performed without complications and the haemodynamic status improved with a sharp decrease in the maximum LVOT gradient (60 mmHg), and a slight elevation of blood pressure. Hours after the ablation procedure, the patient developed a complete atrioventricular block. A dual-chamber pacemaker was implanted via the left axillary route, placing the ventricular electrode in the right ventricular apex.
Because the right branch and the left anterior fascicle are usually supplied by septal branches of the left anterior descending artery, after ASA procedure we have to observe a new right bundle branch block. Therefore, complete heart block requiring a pacemaker occurs in a significant number of patients after ASA.
The progressive improvement of the patient and the resolution of the septic condition allowed the gradual weaning of ventilatory and vasoactive support. During the recovery in the cardiology ward, the patient underwent respiratory and physical rehabilitation. At discharge, 38 days after admission, the echocardiogram showed a thinned anterior ventricular septum (7 mm) and a complete resolution of dynamic LVOTO (peak gradient of 19 mmHg with Valsalva manoeuvre). Left ventricle systolic function remain normal. At one year of follow-up, the patient remained without LVOTO with bisoprolol 5mg bid, and in NYHA functional class II/IV.
Conclusion
Patients with hypertrophic obstructive cardiomyopathy may develop acute heart failure precipitated by other conditions, such as infection or severe anaemia. Sometimes, decompensated obstructive HCM may present with worsening obstruction and mitral regurgitation, often with an unsatisfactory outcome.
In some cases, stabilization with vasoactive drugs, ventilatory support or even ventricular assists devices may help the timing to provide the best treatment strategy. In many cases, this therapy consists of septal reduction (surgical myectomy or alcohol ablation).
In our case, urgent treatment with alcohol septal ablation ameliorated the patient's haemodynamic instability, precipitated by a respiratory infection.
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.