The most recent guidelines for the management of essential hypertension, published jointly in the 2007 by the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC), recommend a blood pressure goal of 140/90 mmHg in the general hypertensive population and a lower goal of 130/80 mmHg or less in patients with type 2 diabetes and in high-risk individuals, such as those with a clinical history of an acute cerebrovascular or coronary event or with an evidence of target organ damage (1). Based on the information provided by recent clinical trials, however, the issue of the risk/benefit ratio of aggressive blood pressure-lowering interventions and the so-called “J-curve” phenomenon (2) have been a matter of academic and clinical debate. As a result, an ESH task force recently updated some of the recommendations for hypertension management, with special emphasis on the definition of the blood pressure goals (3).
1- The “J-Shaped Curve" Hypothesis: previous history
The first evidence in favour of the “J-curve” was provided in 1979 by Stewart who claimed in a retrospective analysis of 169 hypertensive patients that the risk of myocardial infarction was of greater magnitude in patients in whom the diastolic blood pressure was lowered to less than 90 mmHg compared with 100 mmHg to 109 mmHg (4).
In 1987, a group of british investigators published a retrospective analysis of 939 treated hypertensive patients (5). From this analysis, they claimed that lowering of the diastolic blood pressure to less than 85 to 90 mmHg was associated with an increase in fatal myocardial infarction in patients with pre-existing ischemic heart disease. Support for this view appeared to be provided by Alderman and coworkers (6), who observed a huge number of previously untreated hypertensive patients for about 4 years. They found that the 39 fatal and nonfatal myocardial infarctions that occurred in the study were significantly more common in patients with a small fall in diastolic blood pressure (=6 mmHg) or a large fall (=18 mmHg), whereas patients with a reduction of diastolic blood pressure between 7 and 17mm Hg had a significantly smaller risk. Studies supporting the "J-shaped curve" hypothesis have been mostly retrospective, often open, and commonly have included too few events to allow significant conclusions to be reached. Furthermore, “J-shaped" relationships between cardiovascular events and blood pressure have also been described in untreated or placebo-treated patients, which suggests that increased event rates at lower blood pressure may be a sign of poor health conditions, particularly in the elderly. However, the real issue is not whether the relationship between achieved blood pressure and cardiovascular risk is ‘“J-shaped" (as it must be), but whether there are additional benefits or risks in lowering the blood pressure of patients with hypertension to fully normotensive levels, that is, to diastolic blood pressure between 70 mmHg and 85 mmHg.
2 - The “J-Curve" Phenomenon: Recent Findings
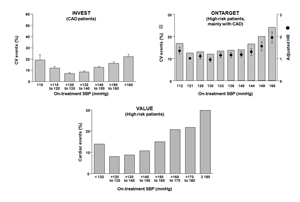
The existence of a “J-curve” has been investigated for both systolic and diastolic blood pressure, on the assumption that a critical level of blood pressure (particularly diastolic) is of vital importance for maintaining coronary blood flow adequate to the physiological needs. The results of four recently published studies, looking separately at systolic blood pressure (Figure 1) (7-9) and at diastolic blood pressure (10) have concluded in favour of the existence of a “J-curve”. These data have led us to readdress the question of whether blood pressure is sometimes lowered too far, resulting in underperfusion of vital organs that increases cardiovascular risk, The issue is open to several considerations.
First, although there must be a blood pressure value below which organ perfusion is compromised, observational studies in patients initially free of cardiovascular disease show that the relationship between blood pressure and the cardiovascular event rate is substantially linear down to very low blood pressure values (about 110/70 mmHg), which are only exceptionally achieved during antihypertensive drug treatment. Second, It is possible that in patients with high cardiovascular risk, impairment of the mechanisms that guarantee blood flow autoregulation elevates the blood pressure threshold below which organ perfusion is reduced (2), However, the extent of this elevation (which may differ between patients in relation to the degree of organ damage and age) has never been unequivocally established by trials specifically designed to explore the advantages of more-intense versus less-intense blood pressure lowering. Third, despite adjustment for initial demographic and clinical differences between groups, post-hoc analysis of trial results cannot escape the problem that the members of the group with the lowest on-treatment blood pressure could have had the greatest initial cardiovascular risk, which caused both the excessive blood pressure reduction and the increased incidence of cardiovascular events. Indeed, this idea is supported by the evidence of a similar J-curve phenomenon in placebo-treated groups of several trials (2). Furthermore, the post hoc analyses have consistently showed that the nadir of cardiovascular outcome incidence occurred at a rather wide range of blood pressure values, between 120 mmHg and 140 mmHg systolic blood pressure and 70-80 mm Hg diastolic blood pressure, suggesting that within this low range, the differences in achieved cardiovascular protection are small (2-3). This finding is in line with the results of observational studies showing that the relationship between blood pressure and cardiovascular events is linear when cardiovascular events are quantified on a logarithmic scale, which implies smaller absolute differences at lower blood pressure values.
3 - Blood pressure goals
Based on the above mentioned clinical trials results, in the 2009 a reappraisal document of the European guidelines made a number of recommendations regarding blood pressure goals of antihypertensive drug treatment (3). These recommendations can be briefly summarized as follows. In the general hypertensive population the recommendation to decrease systolic/diastolic blood pressure below 140/90 mmHg in all hypertensive patients still remains valid and supported by a large amount of data. As far as diabetic hypertensive population is concerned, the results of The ADVANCE and ACCORD trial have raised the possibility that the benefits of lowering blood pressure gradually flattens at lower systodiastolic blood pressure values (11-12). This has led the ESH in the 2009 document to suggest less ambitious but safer blood pressure targets, i.e. 130-139 mmHg for systolic and 80-85 mmHg for diastolic (3). The same targets should be prudently valid also in hypertensive patients with a history of cardiovascular disease, given the evidence that many clinical trials have been unable to show benefits from more intense lowering of blood pressure. In patients with previous coronary disease, for example, the greater blood pressure reduction induced by active (or more active) treatment was accompanied by a beneficial effect on the primary end point in only two trials, whereas five trials did not show any consistent beneficial effect (2-3).
Figure 1. Relationship between achieved levels of systolic blood pressure (SBP) and risk of cardiovascular events in high risk and coronary artery disease (CAD) patients in three recently published trials (Ref 7-9). HR: hazard ratio.
Conclusion:
Critical analysis of the available data regarding which target blood pressure values should be achieved during antihypertensive treatment in current clinical practice allows the following recommendations to be issued:
- There is enough evidence to recommend that systolic blood pressure should be lowered to 140 mmHg (and diastolic blood pressure below 90 mmHg) in all antihypertensive patients, both those at low to moderate risk and those at high risk.
- The recommendation from previous guidelines to aim for a lower goal for systolic blood pressure values (<130 mmHg) in diabetic patients and in patients at very high cardiovascular risk (those with previous cardiovascular events) may be wise, but it does not appear to be consistently supported by trial evidence.
- A “J-curve" phenomenon may indeed occur when lower blood pressure values are achieved, particularly in patients with advanced atherosclerotic arterial disease.
- It is recommended to lower systolic and diastolic blood pressure to values within the range of 130-139/80-85 mm Hg in all hypertensive patients. The lower values in this range should be the goal of treatment in high risk patients.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.