Background
Myocarditis has been reported in up to 12% of young adults presenting with sudden death and is an important underlying etiology of other myocardial diseases such as dilated cardiomyopathy and arrhythmogenic right ventricular cardiomyopathy.
The incidence of nonfatal miocarditis is probably greater than actually diagnosed. Direct viral infection or post-viral immune-mediated reaction is likely the most common cause of myocarditis but toxic, mechanical injury, drug related inflammation, transplant rejection, etc., can also sustain the inflammatory status.
Although the molecular and cellular pathophysiology may differ between the different aetiologies, cellular infiltration, necrosis, oedema and fibrotic scars are common features. Endomyocardial biopsy (histopathology, immunohistology and molecular techniques to identify viral genomes) is a widely accepted method for diagnosing miocarditis. However endomyocardial biopsy suffers limited sensitivity, the occurence of complications (severe or trivial complications in up 6% of patients) and poor overall inter-observer agreement when applying diagnostic criteria to endomyocardial specimens.
Several papers have studied the diagnostic utility of non-contrast and contrast enhanced CMR in patients with suspected or confirmed myocarditis. Although the lack of large and controlled multicenter trials still prevent us from considering this technology as first choice imaging technique, several reports underline the clinical suitability of CMR in patients with clinical suspected myocarditis.
The CMR comprehensive evaluation in patients with suspected myocarditis
Diagnostic targets for CMR include Left Ventricle regional and global function and morphological abnormalities such as transient increase of ventricular volumes and mass. Other pathologic abnormalities of which pericardial effusion can be easily detected.
The exclusive added value of CMR is the capability to assess pathologic aspects of myocardial tissue as diagnostic features of inflammation. Oedema is an important hallmark of inflammatory cell injury and T2-weighted images sensitively detects tissue oedema. The presence of high signal intensity of oedematous tissue can be easily differentiated from normal darker tissue. In the rare case where an homogeneous oedematous myocardium is present, a more sophisticated post processing approach needs to be adopted.
Furthermore, early on after the injection of contrast agent (two-three minutes) an signal increase can be detected as a marker of increased blood volume in the inflamed area due to regional vasodilatation. Furthermore, the Late Gadolinium Enhancement (LGE) technique specifically reflects irreversible myocardial injury (i.e. necrosis and fibrosis) in the acute phase (acute injured cell membranes) but also in the chronic phase after the inflammatory clearance of necrotic regions (fibromyocytes and large interstitial fibrotic deposits). If all the three markers of myocardial inflammation are used, a Positive Predictive Value of 91% a Negative Predictive Value of 69% and a Diagnostic Accuracy of 78% have been shown.
When to perform CMR and the follow-up
Cases of reduced sensitiveness of CMR when performed too early (within 7 days) after the onset of symptoms have been reported. This may be due to the focal nature of the early stage of the disease.
Furthermore pilot data indicate a prognostic relevance of persisting CMR markers for inflammation at 4 weeks after onset. Thus the decision regarding folow-up of patients with suspected or proven active myocarditis depends on the individual scenario. To summarise:
- CMR should not be performed too early after onset of symptoms (if this decision is clinically acceptable
- A negative CMR should be repeated after some days if performed within 7 days after the onset of symptoms and if the clinical features are such to indicate this diagnosis as likely.
- A positive CMR should be repeated after at least 4 weeks after onset of symptoms.
Fig.1
Patient with recent episode of chest pain and fever. Slight increase in Troponin, ECG inconclusive, normal coronary arteries. At CMR evidence of small areas of Myocardial oedema (arrow). Images obtained by Triple Inversion Recovery technique.
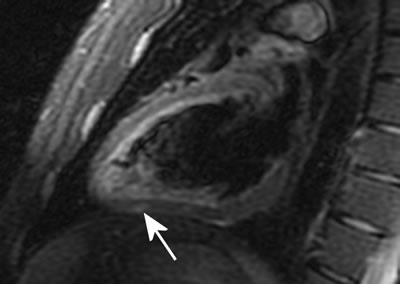
Fig. 2
Patient with clinical features of myocarditis in the past (10 weeks before the CMR study). Normal coronary arteries. At CMR evidence of small areas of fibro-necrosis (arrows). Images obtained using Late Gadolinium Enhancement technique.

Conclusion:
The use of CMR appears suitable to identify patients with ongoing inflammation. All the tissue markers of inflammation should be evaluated during the CMR study in a patients with suspected myocarditis
- T2 weighted images to detect oedema,
- T1 images early after gadolinium administration to detect increased blood volume due to vasodilatation and
- Late Gadolinium Enhancement due to the presence of necrosis/fibrosis.
Furthermore left ventricle regional and global function as well as the presence/absence of pericardial effusion need to be assessed. Lasty, the correct scheduling for CMR exams to take place is to be evaluated either in the acute phase or during follow-up.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.