Recent Guidelines on diabetes and on hypertension (1,2) emphasise the growing importance of the obese state in determining cardiovascular risk, particularly when, as it often happens, it clusters together with other major cardiovascular risk factors in the so-called metabolic syndrome which embraces conditions characterised by various combinations of glucose metabolism, lipid metabolism and blood pressure abnormalities.
1 - Obesity and cardiovascular risk
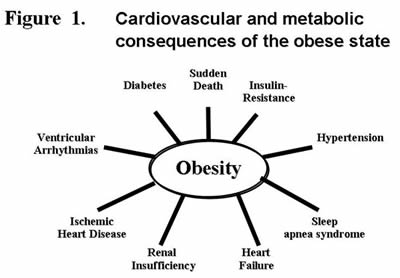
Large scale epidemiological studies carried out in the past 3 decades have clearly shown that the risk of cardiovascular disease increases progressively from the normoweight condition to the overweight and the obese state (particularly of the visceral type), extreme obesity (i.e. the condition in which body mass index exceeds 40 kg/m2) being characterised by an extremely high cardiovascular risk (3). This leads obese people to be more exposed to hypertension, sleep apnea, stroke, coronary artery disease, congestive heart failure, cardiac arrhythmias and sudden death (3) (Figure 1). Needless to say that in addition to the above mentioned clinical complications the obese state is characterised by a 3-to 6-fold increase in the risk of developing diabetes mellitus and renal failure, i.e. diseases which dramatically potentiate the already elevated risk of fatal and non fatal cardiovascular events.
It should be highlighted, however, that the common features of the obese state include the frequent association obesity has with subclinical organ damage, such as microalbuminuria and reduced glomerular filtration rate, arterial stiffness, left ventricular hypertrophy, diastolic dysfunction and carotid artery tickening (3). This renders the assessment of target organ damage of crucial importance, particularly in the severe obese state. Clinical assessment of target organ damage is challenging, however, and still open to a number of questions. For example, which marker of target organ damage may better reflect cardiovascular risk in obesity it is still undefined. It is also unclear whether and to what extent insulin resistance “per se” or obstructive sleep apnea should be regarded as markers of target organ damage. Finally, no recommendation or guideline has been published with the aim of defining whether and when assessment of target organ damage should be performed during non-pharmacological or pharmacological interventions aimed at reducing body weight. This definition should be one of the priorities of the future investigations in the field.
2 - Cardiac hypertrophy and heart failure
Obesity is associated with eccentric and concentric cardiac hypertrophy both in animals and human studies, and increases in left ventricular mass are more pronounced in obese subjects than in lean subjects with comparable blood pressure levels. Even in the absence of hypertension, the heart of an obese individual is chronically volume overloaded with an elevation in cardiac output. As a consequence, obese normotensive subjects feature an increased prevalence of left ventricular dilation and an eccentric pattern of left ventricular hypertrophy (4). Similarly, individuals with the metabolic syndrome more frequently display increased left ventricular mass, both of the concentric and eccentric type. In this population, left ventricular mass is still increased after exclusion of hypertension as the major determinant of increased left ventricular mass and adjustments for blood pressure differences. The observation may suggest that the metabolic syndrome itself exerts adverse trophic effects on cardiac myocytes. Structural and functional cardiovascular alterations can be observed in normotensive individuals with altered glucose or lipid metabolism. Indeed, increased plasma levels of insulin, a characteristic feature of apparent and progressing insulin resistance, has stimulatory growth effects on connective tissue, cardiac muscle, and vascular smooth muscle.
Renin-angiotensin and sympathetic nervous system activation not only contribute to the rise in blood pressure but also exert direct trophic effects on cardiac myocytes. These structural changes which are also likely to be influenced by increased TGF-ß expression, fibrosis and impaired ß-adrenergic receptor signalling result in progressive impairment of left ventricular filling and, subsequently, diastolic heart failure.
In fact, obesity has been identified as an independent predictor of left ventricular diastolic dysfunction in the general population. Furthermore, data from the Framingham study indicate that the risk for heart failure doubles in individuals with a body mass index > 30 kg/m2 when compared to those with a normal body mass index (5).
With long-standing obesity, heart failure symptoms may be further exacerbated by systolic malfunction as evidenced by reductions in mid wall fractional fibre shortening and ejection fraction. In addition to structural changes, cardiac arrhythmias are common in obese subjects. The prevalence of ventricular ectopic beats is substantially elevated, particularly in obese individuals with a concentric pattern of left ventricular hypertrophy. Moreover, obesity is a significant risk factor for atrial fibrillation. Taken together, these data suggest that excess adiposity may increase the risk of heart failure beyond its association with established risk factors for heart failure such as hypertension, left ventricular hypertrophy and diabetes.
3 - Vascular damage
Endothelial dysfunction is one of the earliest markers of vascular damage. Traditional cardiovascular risk factors, such as elevated LDL-cholesterol levels are associated with impaired endothelial function and premature atherosclerosis. Obesity is associated with elevated resting blood flows in many tissues prior to the development of vascular damage through expansion of extracellular fluid and blood volume among other mechanisms (6). However, blood flow reserve during exercise and reactive hyperaemia is reduced in obesity, which may be explained in part by endothelial dysfunction. Indeed, the presence of the metabolic syndrome has been linked to impaired endothelium dependent vasodilation in groups of different ethnic backgrounds (7). Arterial stiffening, another commonly measured marker for vascular damage, also occurs more frequently in individuals with the metabolic syndrome beyond age-related changes. In addition to vascular stiffness, the clustering of at least three components of the metabolic syndrome was independently associated with increased intima-media thickness in the Baltimore Longitudinal Study on Aging (8), even after taking into account each individual component of the metabolic syndrome. Further studies will have to address the specific contribution of the metabolic syndrome and its components on arterial wall damage. The task will be demanding given the complex underlying pathophysiology. Increased blood pressure, inflammation, impaired vascular repair mechanisms, hyperglycaemia, lipotoxicity, oxidative stress, neurohormonal activation, and combinations of these mechanisms are prime suspects and deserve further study.
4 - Obstructive sleep apnea
Recurrent episodes of cessation of respiratory airflow caused by upper airway inspiratory collapse during sleep are of frequent detection in obese subjects and obesity is the most important modifiable risk factor for sleep-disordered breathing (9). This clinical condition has direct and deleterious effects on cardiovascular function, the most relevant are being represented by the risk of sudden death due to the occurrence during the apnoic episodes of life-threatening arrhythmic episodes triggered by hypoxia-induced massive cardiac sympathetic activation (10).
5 - Therapeutic implications
Weight loss by dietary intervention, physical exercise, pharmacotherapy and bariatric surgery can prevent and/or delay the development and progression of several obesity related risk factors for cardiovascular disease (2,4).
Statins, anti-diabetic drugs and antihypertensive agents should be given in presence of dysilipidemia, diabetes and hypertension respectively (2-4). Insulin sensitizers have been shown to reduce the risk of development of new onset diabetes. In contrast, the us of endocannabinoid C1-receptor antagonists, such as rimonabant, although effective in reducing body weight, has been found to be associated with increased incidence of serious side effects. This has led to the premature interruption of the ongoing large scale clinical trials with the use of rimonabant and the drug has been withdrawn.
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.