Background
Percutaneous coronary interventions (PCIs) have been shown to be superior for the treatment of acute myocardial infarction (AMI) compared to fibrinolytic or other non-invasive treatment strategies (1). Randomised trials showed a significant reduction in the rates of death and recurrent ischemia when using PCI compared to medial treatment in AMI.
With the introduction of drug eluting stents (DES) into the market, the question appeared whether the use of DES instead of bare metal stents (BMS) would further improve the outcome of patients with AMI. The first randomised studies evaluating the role of DES in AMI became available in 2005 (2). Here we will discuss the role of DES in patients presenting with AMI which has been very recently suggested to be superior to BMS in an unselected, population based cohort of patients with myocardial infarction (3).
DES versus BMS in AMI
1) Randomised trials
Numerous trials have investigated the role of DES compared to BMS in patients presenting with AMI (4). Within randomised trials, more than 3600 patients with AMI have been studied.
Published trials were performed using paclitaxel- or sirolimus- eluting stents with various durations of clopidogrel treatment (3-12 months). In most trials the follow-up of patients was 12 to 24 months.
Meta-analyses (4;5) suggest that DES were :
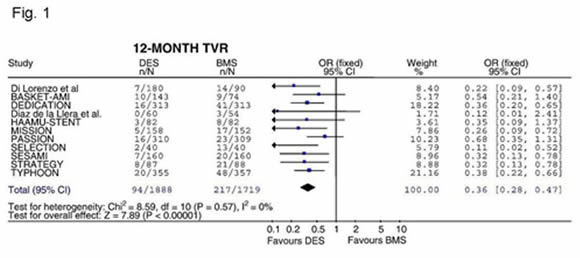
- able to significantly reduce the risk of target vessel revascularisation compared to BMS (odds ratio in two meta-analyses including 11 and 8 randomised trials 0.36 (95%CI 0.28-0.47) and 0.38 (95%CI 0.29-0.50; figure 1) .
However,
- stent thrombosis was not significantly different between groups treated with DES or BMS.
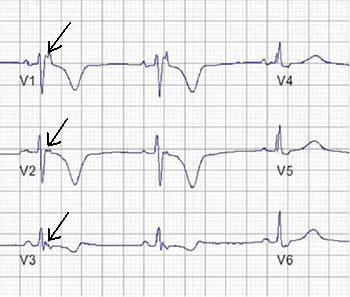
- the important endpoint mortality was not significantly reduced in patients treated with DES (figure 2).
- duration of dual oral antiplatelet therapy did not have impact on the mortality endpoint as well as the duration of follow-up in the analyses available, (max. 24 months).
- the rate of reinfarction was not influenced by the choice of stents. No significant differences were observed in the main two published meta-analyses between DES and BMS at one year follow-up.
- again, longer follow-up or duration of dual platelet inhibition did not influence the results.
Taken together, the results derived from randomised controlled trials demonstrate a benefit in target vessel revascularisation after DES use in STEMI patients undergoing primary angioplasty but no effects on mortality and reinfarction. Follow-up data for 12 months suggest that stent thrombosis is comparable in DES and BMS treated STEMI patients.
2)
A recently published study in an unselected, population based cohort of patients with myocardial infarction has challenged the results of the randomised trials (3). In this study, 7217 patients treated for STEMI and non-ST elevation AMI (NSTEMI) in Massachusetts hospitals between April 1, 2003 and September 30, 2004 were identified and assigned to either the DES or BMS group according to the stent type used during the acute intervention. The primary outcome was defined as death from any cause within 2 years after the initial procedure. Patients treated with DES (n=4016; 71% sirolimus eluting stents, 27% paclitaxel-eluting stents, 2% both) were slightly younger (63.6±13.4 versus 64.3±14.0, p=0.03) and suffered more frequently from diabetes, hyperlipidemia and hypertension. In contrast, patients receiving a BMS (n=3201) suffered more often from cardiogenic shock, ejection fraction below 30% and AMI with ST-segment elevation and had more often emergency procedures. To overcome these differences in treatment groups, a propensity-score model was applied. In this model, potential confounders (up to 63 including demographioc factors, medical history, risk factors etc.) were used to build a propensity-score and patients with similar scores were then matched. 2570 patients were matched and further analyses suggested a balance between treatment groups.
Patients treated with DES had a significant lower mortality (primary endpoint) after 2 years compared to patients in the matched group receiving a BMS (NSTEMI and STEMI patients, 10.7% versus 12.8%, p=0.02). These results were also observed for patients with STEMI and patients with NSTEMI. Interestingly, the rates of reinfarction did not significantly differ in the total population of patients whereas a significant reduction in reinfarction was observed in patients with NSTEMI (12.8% versus 15.6%, p=0.04). In accordance with the published randomised controlled trials, target vessel revascularisation was significantly reduced in all groups (9.6% versus 14.5%, p<0.001).
Taken together, the results derived from a study evaluating an unselected, population based cohort of patients with myocardial infarction suggest that the use of DES is associated with reduced rates of death and repeat revascularization at 2 years of follow-up compared to BMS.
Does these analyses change our strategy in patients with AMI?
The question arises from the available data whether we should use DES as a preferable strategy in patients presenting with AMI.
- First, the study by Mauri et al. confirms the data from randomised trials that DES in AMI reduce the rates of target vessel revascularisation.
- Secondly, it appears that reinfarction rates are not significantly reduced in patients treated with DES compared to BMS. This is confirmed in all randomised trials.
- Thirdly, the question remains whether the observed differences in mortality rates are due to a selection bias or a true observation.
Inclusion of propensity scores can help to reduce large biases, but significant biases may remain especially since unobserved confounders can not be included into the statistical model. Therefore, only large randomised trials with adequate follow-up will allow us to adequately address the question whether DES treatment has benefits concerning mortality rates compared to BMS. For the moment, patients presenting with AMI should be treated with BMS.
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.



 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.