In routine clinical practice, coronary angiograms (CAG) are assessed only semiquantitatively: the cardiologist, performing CAG describes subjectively approximate luminal narrowings of major epicardial coronary arteries (expressed as % stenosis). Obviously, this is highly subjective and has high inter-individual variability.
In research protocols, true quantitative computerised analysis of CAG is used (1, 2). The operator selects the coronary segment to be measured and automated contour detection system delineates the coronary lumen and calculates several parameters: minimal luminal diameter, % diameter stenosis, % are stenosis, etc.
Surprisingly, the systematic qualitative assessment of CAG is usually lacking. Our center is currently testing the hypothesis, that qualitative despription of coronary involvement might contribute to the CAG result. Since 2005 we describe each CAG in two ways: qualitatively (with words) and (semi)quantitavely (with numbers). The qualitative description is not influenced by the presence or absence of >50% stenosis, but represents only the verbal description of the "quality" of angiographically visible coronary artery disease (table 1).
- Example 1: Type 2 "diffuse coronary calcifications" may include three (or more) clinically entirely different patients: (a) 100% occlusion of diffusely calcified right coronary artery in ST-elevation myocardial infarction, (b) severe 3-vessel disease with diffuse calcifications in stable angina, (c) patient with atrial fibrillation and no significant stenosis with coronary arteries diffusely calcified, etc.
-
Example 2: Patients with nonobstructive (all lesions < 50%) mild coronary disease are frequently described in routine practice as having "normal CAG". In our center similar patients are never described as "normal" (3), but are assigned one of the coronary involvement types – it may be ectasias, calcifications, focal lesions, diabetic type, etc.
Initial experience is described here. Based on the retrospective review of 2778 consecutive CAG performed during one year period 10 distinct qualitative types of angiographically visible coronary involvement were defined (table 1). This classification is now routinely used by four Czech tertiary university centers. During the description of each routine CAG the cardiologist asigns patients to one of these 10 types. During the initial 6 months, a total of 4093 consecutive CAG were prospectively described in this method. The relative frequency of each angiographic type was assessed. The inter- and intra-observer variability was tested on 200 consecutive CAG performed after 4 months experience with routine qualitative assessment.
The relative frequency of each angiographic type in this initial prospective cohort is shown in table 1. The inter-observer agreement was in 84%, intra-observer agreement in 95%. All disagreements were within three types: calcifications, "diabetic" disease and focal atherosclerosis.
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.
Conclusion:
This new method of simple qualitative assessment of routine CAG into ten distinct types of coronary involvement is feasible and reproducible. It remains to be established, whether it might help to elucidate the relative role of different etiologic factors contributing to the clinical picture of coronary artery disease (4-7). We believe, that it may at least add another type of information to the physician, who referred the patient for CAG.
Fig. 1: CAG of a patient with non-Q-wave myocardial infarction.
Semiquantitative CAG description (used in most routine settings):
Mid-LAD 70%, proximal OM 90%.
Qualitative + semiquantitative CAG description (as used in our center): Right dominant coronary type. Entirely diffuse "diabetic" coronary irregularities, with small lumen diameter (1,5 – 2,5 mm) of all left coronary artery branches. Double-vessel disease: significant stenoses on mid-LAD (70%) and on proximal segment of obtuse marginal artery (90%).
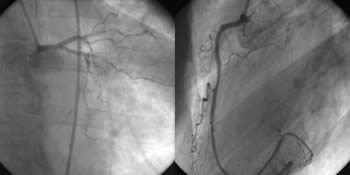
Fig. 2: CAG in a patient with ST-elevation myocardial infarction.

Semiquantitative CAG description (used in most routine settings):
Distal RCA 90% with thrombus. Left coronary artery normal.
Qualitative + semiquantitative CAG description (as used in our center): Right dominant coronary type. Coronary ectasias involving entire right coronary artery and proximal segment of the left circumflex artery. Large partially occlusive intraluminal thrombus, probably without pre-existing significant stenosis in the largest aneurysmatic segment of the RCA. Due to the likely absence of pre-existing stenosis and extremely large RCA diameter (> 6 mm) no PCI is recommended and treatment by intracoronary GP IIb/IIIa inhibitor should be used.
Petr Widimsky
Cardiocenter, Charles University Prague, Czech Republic.
Table 1: Qualitative description of coronary angiogram.
1. Coronary ectasias : Segmental or diffuse aneurysmatic dilatations 5 mm (Prevalence in consecutive cath-lab patients (acute & chronic 1%))
2. Diffuse coronary calcifications : Diffuse and/or massive calcifications, visible in at least two coronary arteries by fluoroscopy (without contrast), (Prevalence in consecutive cath-lab patients (acute & chronic 11,6%))
3. Isolated coronary thrombosis or embolism (in otherwise angiographically normal arteries) : In situ coronary thrombosis or embolism into coronary artery without other angiographically visible signs of atherosclerosis (for details see ref. 8), (Prevalence in consecutive cath-lab patients (acute & chronic 1,9%))
4. Diffuse "diabetic" irregularities without calcifications : Totally diffuse coronary involvement (without any healthy coronary segment), (Prevalence in consecutive cath-lab patients (acute & chronic 12,8%))
5. Focal atherosclerosis : Combination of at least one non-spastic, non-thrombotic focal lesion (obstructive or non-obstructive) with multiple angiographically normal coronary segments. (Prevalence in consecutive cath-lab patients (acute & chronic 54,9%))
6. Congenital coronary anomaly : Coronary fistula, abnormal coronary origin or other congenital anomaly without other visible coronary disease, (Prevalence in consecutive cath-lab patients (acute & chronic 0,05%))
7. Coronary spasm : Angiographically proven spasm (not catheter-induced) in otherwise normal CAG, (Prevalence in consecutive cath-lab patients (acute & chronic 0,1%%))
8. Myocardial bridge : Systolic occlusion of coronary segment with normal lumen in diastole in oherwise normal CAG, (Prevalence in consecutive cath-lab patients (acute & chronic 0,1%))
9. Spontaneous coronary dissection : The proximal tear is at least 2 cm distally from the catheter tip or dissection is first proved by non-invasive imaging (otherwise iatrogenic dissection is most likely), (Prevalence in consecutive cath-lab patients (acute & chronic 0,03%))
10. Normal CAG : Entirely normal CAG, including absence of any (even minor) irregularities, (Prevalence in consecutive cath-lab patients (acute & chronic 17,5%))
Restenosis is not presented as an independent type, because it is a iatrogenic disease and patients have native preexisting coronary involvement type.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.