Since Cardiac Resynchronisation Therapy (CRT) started to be applied in heart failure it has been clear that around 30% of patients are unresponsive to this therapeutical approach. The research into new selection criteria is currently involving all the imaging techniques available.
MRI allows the non-invasive evaluation of site and transmurality of scar tissue in post-ischemic cardiomyopathy. This morphologic information is likely to be integrated with other parameters derived from electrophysiology or imaging techniques to reduce the number of non-responders.
1 - MRI to detect scar tissue and predict non-responders to CRT
Among other techniques, MRI allows to detect the presence of scar tissue precisely, depicting the segments involved and the transmurality of necrosis in each segment. In post-ischemic cardiomyopathy, scar tissue may play a key role for predicting non-responders to CRT. Namely the transmural necrosis of posterolateral segments has been supposed to be responsible for a less effective or even ineffective left ventricle pacing (1).
2 - Left ventricular dyssincrony by Echocardiography in predicting reverse remodelling
However, other researchers have postulated that the presence of necrotic areas are less sensitive than other parameters such as, for example, the evaluation of left ventricular dyssincrony by Echocardiography in predicting reverse remodelling (2).
This controversy is probably based on differences in study protocols, patient selection and differences in the end points considered as well as the methods used to evaluate the outcome. Despite the efforts, none of the proposed parameters derived by the different imaging techniques has reached a level such a level of evidence as to be suggested in the “guide lines” edited by the Scientific Societies.
3 - Individual diagnostic flow charts
At the present stage the patients that are candidates for CRT are preventively evaluated with the different methods available in the single site on individual diagnostic flow charts. From a practical point of view, it has to be considered that the evaluation of scar by MRI is an easy, fast and risk free task and is routinely used in all advanced cardiac centers. Furthermore, once the scanner and the procedure have been optimised, the results are robust, repeatable and almost operator independent.
4 - The integration of the morphologic findings regarding scar distribution with the ones obtained with the other techniques
In the figure below, you will see an example of postero-lateral necrosis. For these reasons and despite the lack of consolidated results it seems reasonable to suggest a preventive evaluation of scar localisation and extension by contrast enhanced MRI. With respect to other techniques such as ultrasonography (echo, Doppler, tissue Doppler, stress-echo), computed tomography (for the evaluation of cardiac veins), scintigraphy, electrophysiology (and others?) a realistic approach could be the integration of the morphologic findings regarding scar distribution with the ones obtained with the other techniques.
Conclusion
This organising and financial effort is greatly justified by the cost of the resynchronisation device, the indirect costs due to hospitalisation, etc and primarily by the hope to reduce the percentage of non-responders whose number makes the CRT clinically and financially frustrating.
The depiction of myocardial scar is also helpful for a better understanding of electrophysiologic data such as high impedence on the tip of the stimulating catheters which are often recorded during their positioning in myocardial area with post-ischemic necrosis.
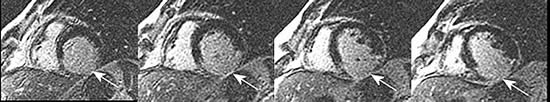
Legend of the figure
Images obtained by MRI (post contrast delayed enhancement technique) in a patient with a previous infero-lateral infarction. In white, the necrotic tissue (arrows).
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.