In conventional practice, in the absence of electrocardiographic documentation of syncope, cardiac pacing therapy of neurally-mediated syncope has been principally guided by the results of tilt-table testing. Controlled trials of tilt-guided therapy, however, have given controversial results. Learning how to select the patients suitable for pacing is probably the prerequisite for success.
Background
When arrhythmia is suspected to have a role in the genesis of syncope, the correlation of spontaneous syncopal episodes with abnormal findings detected by an Implantable Loop Recorder can be regarded as a reference standard for selecting suitable candidates to cardiac pacing therapy.
Recent data coming from Implantable Loop Recorder studies in patients affected by neurally-mediated syncope (1,2) showed that the mechanism of spontaneous syncope was heterogeneous to bradycardia or asystole, approximately accounting, for only one-half of syncope events.
Pacing is potentially effective when an asystole is documented at the time of syncope. However, there is no rationale for the use of pacing in patients without documented brady-arrhythmias. Indeed, in the ISSUE 2 study (2), the 1-year syncopal recurrence rate was 5% in those patients receiving a pacemaker after documentation of an asystolic spontaneous syncope (compared with 41% recurrence rate in non-asystolic group).
As a consequence of this reasoning, the capability of tilt testing to predict the exact mechanism of spontaneous syncope should have practical therapeutical importance. In the ISSUE-2 study (3), the responses to tilt testing (passive or with nitroglycerin challenge) were prospectively correlated with the mechanism of spontaneous syncope documented by Implantable Loop Recorder in 94 patients. An asystolic pause was more frequently found during spontaneous syncope than during tilt testing (45% vs 21%, p=0.02), but those patients with an asystolic response during tilt testing also had an asystolic response during spontaneous syncope with a positive predictive value of 80%.
In other words it seems that an asystolic response during tilt testing is able to predict an asystolic response during spontaneous syncope with a 20% risk of misdiagnosis, but a mixed or vasodepressor response during the test cannot exclude an asystolic spontaneous syncope.
Data from literature
Pacing in neurally-mediated patients with positive response to tilt testing has been the subject of 5 major multicentre randomised controlled trials (4-8): 3 unblinded gave positive results and 2 blinded gave negative results.
In this regard, the strongest supportive evidence is provided in the published report of the North American Vasovagal Pacemaker Study (VPS) (4), and the pacemaker arm of the European VASIS trial (5). In the randomised controlled Syncope Diagnosis and Treatment Study (SYDIT) (6), the pacemaker was superior to the beta-blocker atenolol in preventing syncopal recurrences. The Second Vasovagal Pacemaker Study (VPS II) (7) and the Vasovagal Syncope and Pacing Trial (Synpace) (8) differed from the previous trials because the patients of the control arm had received a pacemaker implant that was switched off. Although there was a 30% reduction in syncope recurrence rate, the VPS II study failed to prove a significant superiority of pacemaker therapy. In the Synpace study, syncope recurred in 50% of patients assigned to active pacemaker and in 38% of patients assigned to inactive pacemaker.
Putting together the results of the 5 trials, 318 patients were evaluated; syncope recurred in 21% (33/156) of the paced patients and in 44% (72/162) of the not paced patients (p<0.000). It seems that pacing therapy might have been effective in some but not in all patients. This is not surprising if we consider that pacing is probably efficacious for asystolic reflex but has no role to combat hypotension which is frequently the dominant reflex in neurally-mediated syncope (mixed and vasodepressor forms).
Need for patient selection
Different selection criteria is probably the most important reason that explains the different results observed in the above trials.
In the most positive studies, i.e., VASIS (5) and SYDIT (6) trials, the patients had a positive cardioinhibitory response during tilt testing whereas not in VPS 1 and 2 (4,7) and only about a half in SYNPACE (8). We know from ISSUE study (3) that an asystolic response during tilt testing has a 80% positive predictive value that spontaneous syncope detected by Implantable Loop Recorder is also asystolic. In other words patients with asystolic tilt response are likely to benefit more from pacing therapy because their spontaneous syncope is asystolic. The selection based on a positive cardioinhibitory response during tilt testing limit greatly the number of potential candidates for pacemaker therapy since a cardioinhibitory response occurs in about 10% of patients undergoing passive or nitroglycerin tilt testing (20% of positive).
Clinical perspectives
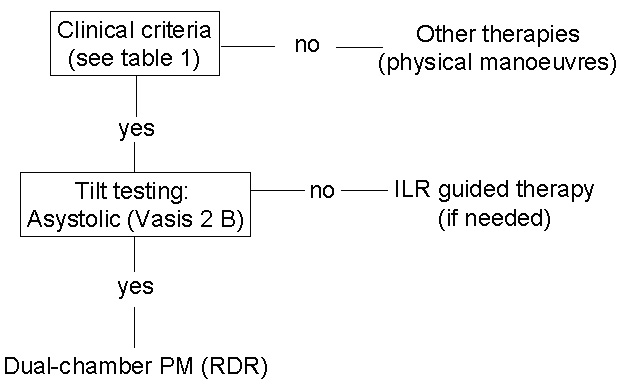
Loop recorder guided therapy is the strategy of choice for selecting suitable candidates to cardiac pacing therapy (2). This strategy, however, implies that therapy is delayed until electrocardiographic documentation of spontaneous syncope is obtained. This may require a long period of time. The capability of tilt testing to predict spontaneous syncope would allow to anticipate therapy and avoid the implant of a loop recorder. A proposed strategy is summarised in Figure 1.
Even though no definite answer can be drawn untill larger prospective therapy trials are performed, it seems that an asystolic response (Vasis 2B type, pause >3 seconds) during tilt testing predicts with a sufficient probability a similar event during spontaneous syncope also and could therefore be used to select patients suitable for cardiac pacing. Apart from asystolic responses, tilt testing has a weak correlation with spontaneous syncope and is unable to guide subsequent therapy. In these cases a loop recorder should be implanted before embarking in pacing therapy.
However, a positivity of the test does not automatically imply the need for pacing therapy. Indeed, it must be underlined that the decision to implant a pacemaker needs to be kept in the clinical context of a benign condition which affects frequently young patients. Thus, cardiac pacing should be limited to a selected proportion of patients affected by severe vasovagal syncope (Table 1).
In accordance with the guidelines of the European Society of Cardiology (9), cardiac pacing may be necessary in patients older than 40 years who present with high-risk or high-frequency settings, such as when:
-
syncope is frequent, altering quality of life
-
syncope is recurrent and unpredictable (absence of presyncope symptoms) and exposes the patient to high-risk of trauma
-
syncope occurs during high-risk activity (driving, machine operation, flying, etc.)
The clinical features of the ISSUE 2 population (2) help define the characteristics of the patients suitable for cardiac pacing; they had a mean age of 65 years, had a history of recurrent syncopes beginning in middle or older ages, presenting without warning and causing frequent injuries (Table 1). No more than 5% of the patients affected by neurally-mediated syncope have these characteristics. Pacing should be discouraged in patients with less severe features and alternative therapies, i.e., physical counterpressure manoeuvres, should be preferred.
Table 1. Clinical characteristics of the patients suitable for cardiac pacing
- Syncope is frequent (>5 episodes in recent years) and alters quality of life
- Syncope is unpredictable (absence of presyncope symptoms) and exposes the patient to high-risk of trauma
- Syncope occurs during high-risk activity (driving, machine operation, flying, etc.)
- No other effective therapy is available and the patient has been informed of the permanent nature of the therapy
Figure 1. Flow pathway for selecting tilt-positive patients suitable for cardiac pacing
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.