Mechanisms
In acute myocardial infarction the aggressive therapy of modern cardiology is geared toward re-opening the related infarcted artery. Nevertheless, even though the artery may be opened, there may still be regions with a low or absent flow, within the irreversibly injured myocardium(1).
Several mechanisms underlie this pathophysiological status. It may be as endothelial cell blebbing, white cell infiltration, red blood cell stagnation and extravascular edema, microvascular spasm, platelet aggregation, inflammation, etc. This process may be even worsened by reperfusion due to injury caused by oxygen-free radicals. Furthermore, in the clinical setting, the occlusive coronary thrombus can spontaneously embolise distally, during thrombolytic therapy or during percoutaneous transluminal coronary angioplasty (PTCA). In the latter case, plaque components can also be found distally as an embolic consequence of the procedure.
Epidemiology
It has been calculated that one-fifth to one-third of patients with a restored TIMI grade 3 flow have evidence of tissue no-reflow.(2).
Despite recanalisation , regions with no-reflow have a poor outcome.
Indeed there is a proven correlation between tissue no-reflow and a lower global systolic function. the presence of malignant arrhythmias, intractable congestive heart failure, progressive left ventricle remodelling, cardiac rupture and higher mortality.
MRI : advantages
The diagnostic effort to detect the presence and the extension of no-reflow areas is not an easy task and nuclear methods and contrast echocardiography have been proposed.
The diagnostic effort to detect the presence and the extension of no-reflow areas is not an easy task and nuclear methods and contrast echocardiography have been proposed.
Magnetic Resonance Imaging (MRI) has shown more recently, some advantages which seem to fit well with diagnostic purposes. The irreversibly injured myocardium can be assessed both through the evaluation of regional myocardial perfusion and thanks to the acquisition of late images – after the intravenous administration of contrast agent.
The delayed enhancement (DE) of infarcted areas can help to differentiate between viable tissue, necrotic tissue and the gross microvasculature damage with hemorrhage (see Fig. 1) which is seen as a darker area within the infarcted region (3) (Fig 1).
The advantages of DE with respect to the other technique is reduced operator dependence, excellent spatial resolution, and the sharp contrast between the no-reflow areas and the surrounding necrotic tissue. This method is simple, risk free, and relatively non time-consuming (about 20 minutes).
The main advantage of MRI is probably the possibility that it offers of obtaining an accurate three dimensional quantitation of the extension of the no-reflow areas. It has been shown that MRI-DE can be proposed in the clinical setting for this purpose and in many centers it is performed as a routine check after primary PTCA.
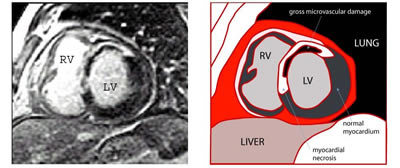
Figure 1: MR image obtained using the delayed enhancement technique after contrast agent administration. Short axis of the left ventricle of a patient with acute myocardial infarction (three days before). The image shows a large anterior myocardial infarction (white area) and the inner large no-reflow area (dark area). LV = left ventricle, RV = right ventricle.
MRI : limitations
There are some limitations which have to be taken into account, such as the setting up of the scanner, the time necessary for obtaining the images after contrast agent administration and, of course, the necessary presence of local expertise in this specific field. However the strongest limitation, which is having to measure the no-reflow with MRI-DE seems more related to the changes occurring in the no-reflow areas in the first several hours after reperfusion which are reactive hyperemia, vasospasm, edema, etc.
There are some limitations which have to be taken into account, such as the setting up of the scanner, the time necessary for obtaining the images after contrast agent administration and, of course, the necessary presence of local expertise in this specific field. However the strongest limitation, which is having to measure the no-reflow with MRI-DE seems more related to the changes occurring in the no-reflow areas in the first several hours after reperfusion which are reactive hyperemia, vasospasm, edema, etc.
It has been described that no-reflow can occur following a transitory behaviour that is sustained by microvascular spasm. The ideal time for measuring no-reflow, it is said, is about 48 hours after reperfusion.
By adopting MRI as a diagnostic technique though, it is difficult to adhere to this temporal limit, and in the majority of studies published so far, MRI scanning is performed between 2 to 10 days after the acute event. In these cases, the evaluation by MRI could result in an underestimation of the phenomenon. However, in terms of negative prognostic relevance, the evidence of a persistent no-reflow pattern with intramyocardial hemorrhage has a relevant meaning for the patient's outcome and hence for the treatment to be adopted.
Conclusion:
Contrast enhanced MRI has opened a new insight in a pathophysiological phenomenon which occurs in a relevant percentage of patients with acute myocardial infarction. DE images can help better understand the clinical implications underlying the no-reflow phenomenon. When available, MRI can be used as a standard technique for assessing the immediate consequences of ischemic injury and reperfusion.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.