Abbreviations
(S)BP (systolic) blood pressure
ABPM ambulatory blood pressure monitoring
GSR Global SYMPLICITY Registry
HTN hypertension
RCT randomised clinical trial
RDN renal denervation
RF radiofrequency
Introduction
Hypertension (HTN) is the key trigger for the vicious cardiovascular continuum. In recent years an impressive amount of progress has been made towards controlling a high blood pressure (BP). However, the absolute number of patients with uncontrolled HTN drift forward inexorably [1]. The major interest of the scientific and medical community is currently oriented towards patients with resistant HTN (RHTN), which affects around 10% of the adult hypertensive population and aggravates prognosis [2].
The introduction of device-based therapies became a definitive milestone on the path to overcoming resistance to antihypertensive therapy in this patient strata. Destruction of the adventitial and perivascular sympathetic nerves in the renal arteries (the so-called renal denervation, RDN) represent the most attractive and promising path. The concept of RDN and its biological grounds are based on the interruption of the crosstalk between the kidney and the central nervous system, thus decreasing sympathetic activity. Chronic hyperactivation of [renal] sympathetic nerves has proven to be one of the key pathophysiological mechanisms of HTN and other associated comorbidities [3].
The status of RDN has not been easily established in the blink of an eye. Rather, it was gathered under difficult conditions. The first two studies in RHTN patients using unipolar catheters were a great success in the early 2010s, but then one of the biggest scientific disappointments occurred with the results of the first sham-controlled randomised controlled study (RCT), SYMPLICITY HTN-3 [4], which showed no significant differences in the systolic blood pressure (SBP) between groups (only a 2 mm Hg change).
That was the defining moment which at the same time instigated further research while stimulating the great debate which is still ongoing. In addition to the sticklers and those looking for confrontation, many of the expert teams from around the world deemed it necessary to come up with position statements on RDN [5,6]. Indeed, science does not stay still, and the evidence accumulated over the past several years contributed to a gradual paradigm shift from wariness towards greater generalising of the procedure.
In this review we aim to address the current pro et contra positions on RDN, performed with various techniques in HTN patients.
Renal denervation: PROs
In this section we will cover three relevant arguments favouring RDN: its safety, efficacy, and patient preferences.
Primum non nocere
Every clinician knows ‘safety first’, particularly when it comes to invasive procedures or surgery. From the 1930s through the 1950s, surgical sympathectomies (or splanchnicectomy) were performed in more than a thousand of patients with uncontrolled HTN, but these were ultimately abandoned due to the high rates of disabling side effects [7]. Further drug development made it obsolete and futile as well. All in all, those early sympathectomies were in some ways effective in reducing BP and associated symptoms. When RDN was introduced, these concerns were diminished almost immediately after the first-in-human open label SYMPLICITY HTN-1 trial. Even in the first-generation studies (e.g., SYMPLICITY HTN-2), only <5% of patients experienced adverse procedural events. Since then, there have been no reports on major periprocedural complications both in RCTs and in registries. These were mostly anecdotal cases of pseudoaneurysms and groin haematomas [8]. Transradial access for RDN may advance the procedure, and put an end to vascular site complications. More importantly, as contrast agents are used during the procedure, kidney function was a matter of concern. Again, there was no sign of decline in eGFR up to 9 months in almost 50 patient cohorts in a large meta-analysis [9] as well in the Global SYMPLICTY Registry (GSR) up to 3 years [10]. Finally, pre-clinical studies signalled that local renal artery endothelial injuries might become a problem [11]. However, despite several cases, the annual incidence of renal artery stenting following RDN was estimated at 0.20% (as in the rest of the hypertensive population) [12].
A class effect?
Renal denervation had to go through two rounds of trials to prove its concept. The ‘Big Bang’ of SYMPLICITY HTN-3 forced design reviews of further studies. The chief points of criticism concerned the patient selection process, procedural aspects, and adherence. The second-generation studies that have emerged in the last five years are mostly RCTs with sham-procedure control groups. In almost all of them, multielectrode catheters were used to ensure circumferential energy distribution, some were conducted without medical therapy (the second proof-of-concept round) and with more homogeneous groups. The investigators’ enthusiasm was based on a durable theoretical basis backed by R. Smithwick’s investigation in the 1950s [7], as well as on the urgent need for a method of solving problems in the RHTN patient population. Currently, there are at least five different methods of performing RDN that are known: (a) radio frequency (RF), (b) ultrasound energy, (c) a method based on brachytherapy using β-radiation, (d) a chemical method that introduces various compounds and drugs into the proximal parts of the nerve fibres (most often, ethanol) and finally, (e) magnetic resonance RDN [13]. In most of the second round RDN RCTs, RF ablations were performed but there were two in which ultrasound was used to destroy the nerves. Some baseline parameters and key findings of these studies are shown in Table 1.
Table 1. Baseline characteristics and results of five pivotal randomised clinical trials of renal denervation in the second-generation era.
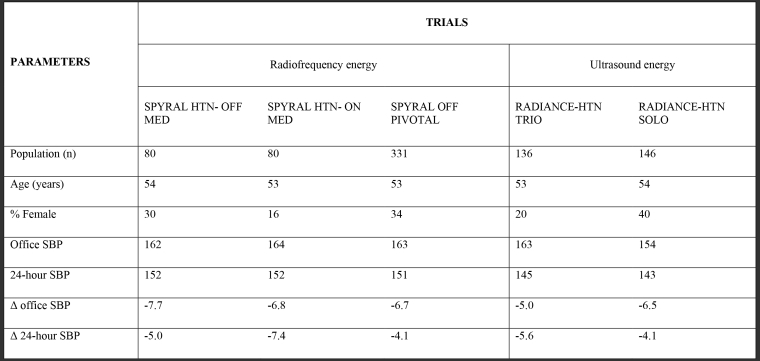
SBP: systolic blood pressure in mmHg
The ∆ of office and 24-hour systolic blood pressure is defined as renal denervation group versus sham-control group (p<0.05 for all).
As opposed to the first-generation RDN RCTs, in these thoroughly planned international RCTs, we notice only a slight decline in office and 24-hour SBP. These might be linked to careful adherence testing in almost all enrolled subjects (witnessed drug intake or toxicological analyses) and simultaneous ambulatory BP monitoring (ABPM) as a primary efficacy endpoint. SPYRAL (RF) and RADIANCE (ultrasound) studies have turned the page of history and provided a crystal-clear signal of a class effect of RDN. The evidence has been strengthened by the GSR, with the largest data set of RDN-treated patients to date (3000 patients worldwide), in which the reduction in 24-hour SBP at three years was –8.9 ± 20.1 mm Hg for the overall hypertensive cohort [14]. These long-term data, the 12-month unblinded results of RADIANCE HTN-SOLO and some other independent but long-lasting studies [8] support the durability of the effect of RDN (Figure 1).
Figure 1. Change in office systolic and diastolic blood pressure dynamics from baseline to 12 months (first timepoint) and to 5 or more years (up to 8 years, second timepoint).
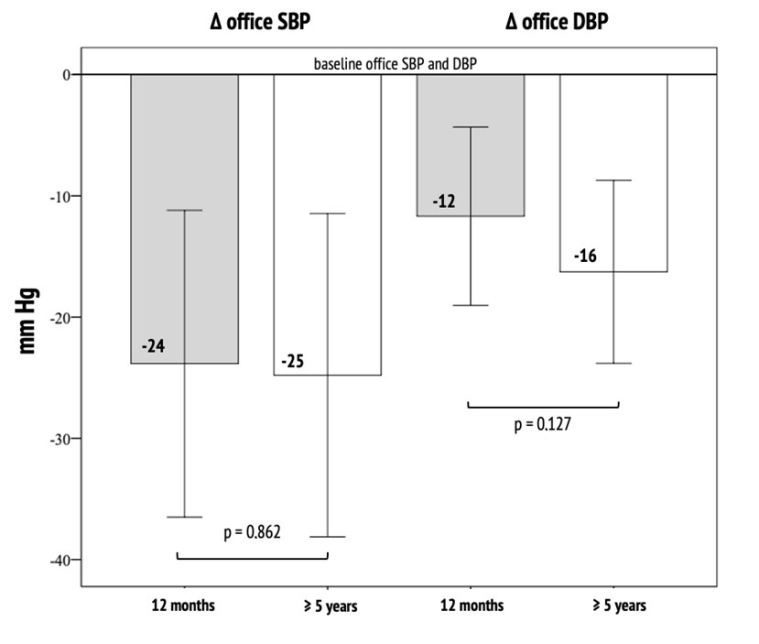
N=22
DBP: diastolic blood pressure; SBP: systolic blood pressure
To date there is one, single-centre, small RCT comparing ultrasound versus RF RND in patients with RHTN (RADIOSOUND-HTN). In this RCT, a lower daytime SBP was observed at 3 months with ultrasound-based ablation compared with RF RDN but only for the main renal artery ablation arm at 3 months (mean difference: -6.7 mm Hg, p=0.038). There was no significant difference found in SBP between the ultrasound and the side branch RF RDN groups [15].
The third method uses the Peregrine Catheter system (Ablative Solutions) with the injection of alcohol directly into the perivascular space via three microneedles. Initially effective (BP reduction), open-label studies have yet to be confirmed in currently ongoing RCTs [6].
Make their voices heard!
There is a global turn towards value-based medicine in most industrialised countries. A patient-centric approach precisely addresses the patient’s preferences and needs, named ‘values’. Today, no one disputes that the more pills a patient is prescribed, the fewer they really swallow. After SYMPLICITY HTN-3, different reports have underscored problems of universally poor adherence to antihypertensive medication in this population. Careful attention to adherence and Hawthorne’s effect became one of the most important issues addressed in second-generation RCTs. On the one hand it helps to conduct purely unbiased RCTs. But on the other hand, it does not help those patients who have trouble with taking multiple drugs for high BP. Patients’ perspective and preference are also important determinants in controlling the disease [6]. It seems that a sizeable percent of hypertensive patients are willing to pay an average of $1445 to avoid taking antihypertensive pills [16]. Moreover, about 30% of such patients might prefer RDN instead of drug therapy, regardless the number of pills or BP level [17]. That is why the structured and close follow-up of patients with RHTN is crucial particularly in Excellence Centres. It should be done in a patient-centric way, including patient-reported outcomes collection, consideration of drug side effects and other barriers for adherence. An RDN should be always considered during patient-provider discussions.
Renal denervation: CONTRAs
The avalanche of criticism appeared post-SYMPLICITY HTN-3 [18]. Here we describe three relevant opposing points: dubious effect on hard endpoints, no clear predictors of intraoperative and long-term success.
For what it’s worth
First, the overall antihypertensive efficacy of RDN is unquestionable. But here are at least two major limitations.
Firstly, the reduction in ABPM of approximately 6 mmHg, reported in new RCTs and in the GSR, equals one antihypertensive drug [19]. The optimistic point of view is that this pill is taken only once and can reduce antihypertensive drug requirements after RDN; the pessimistic view is that the operative treatment is not worth the risk (it is difficult to imagine someone taking such a risk for e.g., enalapril) and not worth the monetary investment.
Secondly, despite the long journey of RDN, we are left with those coveted 6 mm Hg and no equivalent published or in-progress RCT analysing the effect of RDN on the incidence of cardiovascular events. Only predictive modelling studies [20] may be used as indirect evidence. We may only extrapolate the consequences of BP reduction on various associated cardiovascular conditions. One of the possible ways is to analyse high-risk subgroups. In one evaluation of the GSR data, authors found that blood pressure reduction was –10.2 mm Hg in patients with diabetes, –10.1 mm Hg in chronic kidney disease, and –10.0 mm Hg in atrial fibrillation. In 2021, Medtronic announced the launch of the GSR-DEFINE study with an additional 2000 patients who will undergo RF RDN with Simplicity Spyral. The study will collect data for a subgroup of patients to 5 years. These are only observational data but RCTs with such high-risk cohorts are needed to show that BP reduction following RDN protects the brain, heart, kidneys and large arteries [19].
Reinnervation
Despite the indirect evidence of significantly reduced central sympathetic outflow (norepinephrine spill-over, muscle sympathetic nerve activity and positive signals from high-risk patient cohorts), we still do not have a safe, accurate, and clinically practical method to identify complete nerve destruction after RDN (particularly intraoperatively). One of the proposed techniques is endovascular electrical mapping of the renal artery or the use of remodelled RDN energy generators to assess temperature and impedance feedback independently for each electrode. The problem of nerve regrowth is another troubling condition which may cause an escape phenomenon contributing to an HTN relapse and usually occurs in native human kidneys after transplantation. This complication is critical for patients with resistant hypertension and chronic kidney disease [21] although it has not been confirmed in humans and remains pre-clinical evidence.
Responders wanted
Identifying the optimal candidates for RDN is perhaps the greatest challenge for many research groups. Since SIMPLICITY HTN-3 was published, a lot of investigators have been trying to identify the responders and then to find their key distinct features. There are at least two problems at this point. The first one is that the definition of ‘responder’ varies among the studies (office BP or ABPM, ∆ 5- or 10-mm Hg etc.). The second is that baseline BP is often revealed as the one and only predictor of RDN response and success. This phenomenon is easily explained by the revived Wilder’s law of initial value (‘the direction of response of a body function to any agent depends to a large degree on the initial level of that function’). It is hard sometimes to overcome this significant factor during statistical analysis. New prespecified and targeted patient enrolment protocols intended to check the response in the supposed groups (e.g., those with isolated systolic HTN, accelerated heart rate etc.) and incorporation of receiver operator characteristic curves might help researchers to get the answers.
Nevertheless, the points described above are in fact open questions which provide the rationale to conduct more sophisticated and long-term RCTs and they are not intended to pave the way for cancelling RDN.
Take-home messages
In accordance with current position statements and guidelines, a few crucial standpoints must be recapped. These should be taken into account when RDN is considered as a treatment option.
- Renal denervation is safe perioperatively and in the long-term. The rate and type of complications are comparable to any other endovascular intervention requiring femoral access and contrast agents. Transradial access and the use of low-volume, low-osmolar contrast media are sought to minimise complications.
- Renal denervation proved to be rather effective in decreasing office and ambulatory BP both in the short- and long-term. Multielectrode RF or ultrasound RDN techniques are the most studied and evidence-based, thus should be preferred. The choice of each technique should be based upon the availability of resources.
- Patient perspectives and preferences need to be respected and taken into account in a shared decision-making process.
- To date there is no high-quality evidence that RDN impacts on CVD morbidity and mortality. These were only shown in registries, sporadic observational and predictive modelling studies.
- Determination of complete renal nerve destruction in vivo (preferably intraoperative) is an unmet clinical and investigational need. To ensure the completeness of RDN, it is advised to perform multiple ablations (in case of RF RDN) and to focus on side and accessory branches.
- Considering RDN the greater priority should be given to non-frail patients with apparent RHTN without a large pulse pressure whose adherence may be violated or in whom antihypertensive therapy is limited for various reasons. Other patient groups may be considered according to regional statements and expert positions: e.g., in Russia RDN might be performed in patients with incurable secondary forms of HTN [5].
- Structured and extended follow-up of patients who undergo RDN is strongly recommended. These include building up databases with rigorous data management, standardisation of core clinical evaluation protocols, extension of telehealth to facilitate follow-up and provide extra-safety in the COVID-19 era. These steps ease the exchange of information between centres and hospitals, regionally and/or internationally, in order to consolidate evidence.
Conclusion
Resistant hypertension is responsible for excessive morbidity and mortality. A lot of patients are still out of target BP range, representing the most vulnerable strata. Recently, device-based therapies have been introduced to rectify the situation. Of all of them, RDN has earned it’s place in the sun and remains the most resilient modality, thanks to scrutiny from many different angles.
After all, the good news is that the concept of RDN has been (doubly) proved, and its antihypertensive effect is indisputable. The sobering news is that this effect is akin to the addition of one more pill. The bad news is that we still do not know the ideal profile of the patient who can benefit most from the procedure. We are in need of large-scale, prospective, longitudinal RCTs to address points of concern. Hopefully, with these in hand, RDN won’t be treated as either the Holy Grail nor as a global crafty deception.















