Introduction
Salt, in addition to sugar, are known to be the notorious white killers. While the cardiovascular effect of high blood sugar has been well established over the years, the risk of high salt intake on cardiovascular morbidity and mortality is still debated. The relationship between salt intake and poor cardiovascular prognosis is not a consistent linear relationship, but rather a J-shaped curve [1]. This explains why people on significantly high and those on significantly low salt intake experience adverse cardiovascular events. Most guidelines suggest a low salt intake, defined as <2-2.3 g of sodium (equivalent to <5-5.75 g of sodium chloride) per day to reduce high blood pressure and to improve cardiovascular outcomes [2, 3]. The mechanisms by which high salt intake affects the blood pressure are through water retention, vascular remodelling, and endothelial dysfunction [1]. On the other hand, the mechanisms linking low salt intake and high mortality are not yet well understood, although it may involve activation of the renin-angiotensin-aldosterone system (RAAS) and the sympathetic nervous systems as well as an increase in insulin resistance [1].
The habit of high salt intake
Salt consumption varies in different countries across the world, with the highest levels found in Northern China [4] and Japan (where the daily salt intake exceeds 10 g) and the lowest level found in an isolated tribe (Yanomami Indians) inhabiting the tropical equatorial rainforest of northern Brazil and southern Venezuela (consuming as low as 0.2 g salt per day) [5]. Globally, the usual sodium intake is between 3.5–5.5 g per day (equivalent to 9 - 12 g of daily salt) [2].
Since the 12th century, West and Southern African countries have been mining salt and using it to trade with North Africa as well as with Europe. In hot climates, people tend to consume more dietary salt than in cold climates, probably as a result of the increased loss of sodium through excessive sweating in high temperatures. An African diet has a high salt content which is maybe one of the reasons why hypertension is highly prevalent on the continent [6].
In Roman times, salt was called ‘white gold’ as they used it to preserve meat and fish. Nowadays, in European countries, the daily dietary salt intake among most adults ranges from 7 to 13 g, which far exceeds the recommended daily dose of sodium salts [5].
In many Western countries, the high dietary salt content comes from processed food while in African countries, it comes mostly from bread, salted fish, salt added during cooking, and seasoning and spicing foods [6].
In many Sub-Saharan countries there has been a transition in the type of foods available which has resulted in a radical change of dietary habits from plant-based, traditional, and fresh food to processed and fast foods that are usually high in sugar and/or fat and high in salt content as well. These types of food are called energy dense, nutrient poor (EDNP) foods [3].
The awareness and the attitude towards salt restriction was evaluated in a study by Menyanu et al [6] who surveyed people from Ghana and South Africa. They discovered that one third of respondents did not know that a high salt intake could cause cardiovascular problems, which may explain why no actions were taken to reduce their dietary salt intake. Authors also reported that high salt consumption was mainly observed in the younger population and in males. They also noted that frequent alcohol consumption was associated with a lower desire for salt intake [6].
Another study in Austria found that most salt intake was related to table salt, cereals, meat and dairy products. They also observed that salt intake was higher in males and in obese subjects [7].
Data from the National Health and Nutrition Examination Survey (NHANES) indicated that Americans consume on average 3.4 g of sodium each day, which is higher than the recommended daily dose [8].
High salt-containing foods
The words sodium and salt are not synonymous; salt (which is commonly called table salt) is a chemical compound consisting of sodium and chloride. People often use these two words interchangeably, yet it is important to know the difference because the recommended daily doses of sodium and of salt are not the same. There are many other sodium-containing food additives that are used in food production, mainly in processed and canned foods, like monosodium glutamate (MSG), sodium bicarbonate (baking soda) and sodium benzoate.
Salt is an important constituent in our daily foods. It makes bland food tasty, and it is used as a preservative for different types of processed and canned foods. Processed food includes all foods that undergo any changes to their natural state like bread, cheese and other dairy and meat products [7]. Some foods have a high salt content, yet do not taste salty, e.g., pastries, cereals, bread, fast food, and canned and processed food. Accordingly, taste alone cannot be used to determine the level of salt content in food.
It is important to know how to read the nutrition fact labels to identify sodium content in packaged food. The nutrition fact label is usually printed on the back of the food packaging and it lists the number of calories as well as the different constituents in the product. It is crucial to understand that the nutrition information list is usually based on a certain amount of food (one serving or 100 g), not necessarily the whole amount contained in the package. In general, a low sodium content is defined as <140 mg of sodium per serving, while a high sodium content is defined as >400 mg per serving [9].
People who consume high salt-containing foods tend to be more obese than people who consume less salt in their diet. It was found that a high dietary salt intake is somehow related to increased weight gain, partly because of the high energy and fat content of salty food, and partly because salty food tastes better and this increases the desire to eat larger quantities of food [7].
Table 1. Examples of some high salt-containing foods.
| Types of food | Examples |
|---|---|
| Meat | Smoked, salted, or canned, bacon, frankfurters, sausage |
| Fish | Smoked, salted, or canned, sardines |
| Poultry | Smoked, salted, or canned |
| Dairy Products | Regular and processed cheese, cottage cheese |
| Vegetables | Regular canned vegetables and vegetable juices, olives, pickles |
| Bakery | Bread, biscuit, pancake, waffle mixes, pizza |
| Sauces | Tomato sauces, soy sauce, seasoning salt, and other sauces and marinades |
| Pasta | Processed mixes of pasta, commercially prepared pasta, cup of noodles |
| Others | Rice, salted nuts, carbonated beverages |
Salt and Hypertension
Sodium is the main cation (positively charged ion) in the extracellular fluid while chloride is the main anion (negatively charged ion). Sodium is important for many cellular functions and together with chloride, they are responsible for the osmolarity of the extracellular fluid. In addition, sodium is essential for the excitation of nerve and muscle cells, acid-base balance and the secretion of some digestive enzymes. A low-sodium diet can activate the renin-angiotensin-aldosterone system (RAAS), which consequently leads to salt retention and restoration of fluid balance [5].
Excessive intake of sodium (defined by the World Health Organization [WHO] as more than 2 g of sodium or more than 5 g of sodium chloride per day) [3] is directly linked to high blood pressure and it was found that the higher the daily salt intake, the higher the systolic blood pressure [1]. In addition, high salt intake was found to blunt the physiologic nocturnal blood pressure dipping and to increase the daytime heart rate in ambulatory blood pressure monitoring [10]. Conversely, a reduction of dietary sodium/salt intake can lead to not only a reduction in blood pressure, but also a reduction in cardiovascular morbidity and mortality [11].
There are many mechanisms that link high salt intake and hypertension:
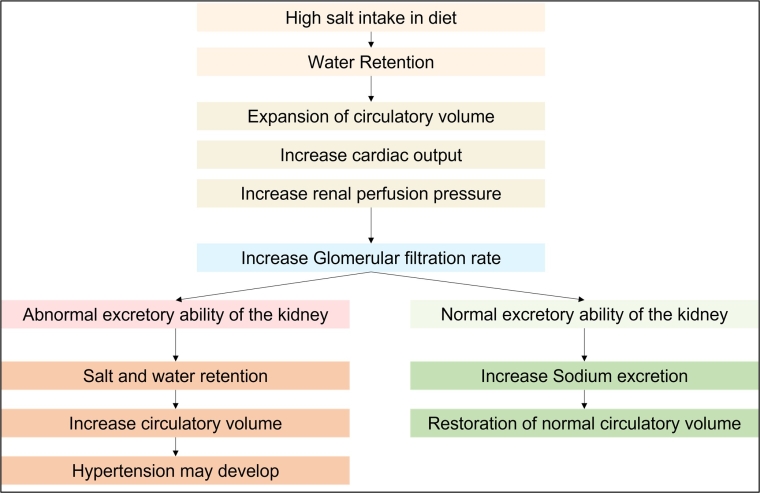
- Water retention - this was explained by the classic concept of Guyton [12], who demonstrated that high salt intake leads to more water retention, which leads to an expansion in the circulating volumes, an increase in cardiac output, and a rise in kidney perfusion pressure. When the kidney perfusion pressure is increased, the glomerular filtration rate increases and sodium excretion increases aiming to restore the fluid balance in the body. This physiological response to a high salt intake is called the pressure-natriuresis mechanism, Figure 1. When the sodium excretory ability of the kidney is compromised, hypertension may develop [1]. Yet, some other studies showed that the circulating volumes and the cardiac output were similar among salt-sensitive and salt-insensitive individuals. They explained these findings by the non-osmotic storage of sodium, meaning that sodium may be stored in the body without water retention [13].
- Increase in systemic peripheral resistance as high sodium triggers remodelling in small resistant arteries - The effect of sodium on the vascular remodelling of small resistant arteries can occur both in normotensive as well as in hypertensive individuals. It was found that the risk of developing hypertension was higher among salt-sensitive normotensive individuals when compared to salt-insensitive ones [1].
- Endothelial dysfunction - it was found that high salt intake can cause marked reduction in the endothelial nitric oxide (NO) which is responsible for endothelium-dependent vascular dilatation. Reduction of NO leads to not only elevation of blood pressure, but also to many blood pressure-independent cardiovascular complications [14].
- Changes in the structure and function of large elastic arteries - it was found that high salt intake could affect the properties of large elastic arteries leading to an increase in vascular stiffness [15].
- Modulation in the autonomic neuronal supply and the sympathetic activity of the cardiovascular system [1].
Figure 1. The pressure-natriuresis mechanism.
Salt sensitivity
Salt sensitivity is defined as the individual’s blood pressure susceptibility to dietary salt intake where changes in blood pressure parallel changes in salt consumption [16]. In salt-sensitive individuals, the physiologic pressure-natriuresis mechanism is impaired and the kidney becomes unable to excrete a sufficient amount of sodium in response to a high sodium intake [1]. People accordingly are divided into salt-sensitive and salt-insensitive individuals, and it was estimated that about 50-60% of hypertensive patients are salt-sensitive. Salt sensitivity is more prevalent in elderly people, females, obese subjects, and patients with chronic kidney disease [5]. Ethnic-specific salt sensitivity was also recognised, as salt sensitivity is more common in people of African descent and people from East Asian regions [17].
The mechanisms behind salt sensitivity are multiple. They include: the retention of sodium caused by abnormal renal excretory response to high urinary sodium, blunted suppression of RAAS, stimulation of the sympathetic nervous system, insulin resistance, genetic polymorphism, and inflammatory processes [1, 5].
Despite the clear association between salt sensitivity and pathophysiological mechanisms of hypertension, physicians cannot not use this fact in everyday clinical practice, simply because of the lack of a practical diagnostic test for salt sensitivity [16].
It is difficult for individual patients to express their daily salt intake. Studies which measured 24-hour urinary sodium excretion and then related these findings to the self-reported salt intake of the individual patients found that there was an underestimation in self-reported sodium consumption due to the difficulty of quantifying salt content hidden in processed foods. In some reports, the degree of underestimation ranged between 29% and 41% [6].
Salt restriction and blood pressure reduction
It has been shown that salt restriction can lower blood pressure, where a reduction of about 1.75 g sodium per day (4.4 g sodium chloride/day) was associated with a mean reduction in systolic/diastolic blood pressure of 4.2/2.1 mmHg, respectively. There was a more pronounced effect (5.4/2.8 mmHg reduction) in patients with hypertension [18].
Many trials suggest that reducing salt intake to moderate amounts is associated with a lower risk of cardiovascular events, yet no definitive evidence has been provided by prospective randomised controlled trials about the optimal sodium intake to reduce cardiovascular events and mortality [2].
Generally, salt reduction to moderate amounts (daily sodium 2.3-4.6 g, equivalent to 5.75-11.5 g sodium chloride) is considered a cost-effective method to reduce high blood pressure and reduce cardiovascular complications accordingly [6, 15].
It is worth mentioning that non-compliance to salt restriction is considered one of the most important causes of difficult-to-control and resistant hypertension.
Salt and antihypertensive medications
A recent metanalysis showed that a calcium channel blocker combined with a hydrochlorothiazide were the most effective antihypertensive drugs in reducing blood pressure in salt-sensitive individuals [19]. In treated hypertensive patients, effective salt restriction could help to reduce the number and/or the doses of the antihypertensive medications [2].
Low salt intake: is it really dangerous?
Prospective cohort studies reported that reducing dietary sodium intake (below 2 g of sodium per day) could reduce blood pressure but was associated with an increased risk of adverse events (all-cause and cardiovascular mortality) in both normotensive and in hypertensive people, suggesting a J-shaped curve phenomenon [2, 20]. On the contrary, epidemiologic studies did not show any adverse effects of low salt in diet.
Currently, there is no convincing evidence, from randomised controlled trials, favouring low sodium intake (<2 g/day) over moderate intake (2.3-4.6 g/day) in terms of reduction of cardiovascular risks and adverse outcomes [15].
Sodium salt versus potassium salt
Many studies have shown the direct relationship between high sodium and hypertension and the inverse relationship between high potassium and hypertension [11]. It has also been repeatedly shown that a reduction in sodium salt and an increase in potassium salt consumption can reduce blood pressure, improve general physical health, and reduce salt sensitivity [21], which is why it is advisable to replace sodium salts with potassium salts. Foods rich in potassium include dried fruits (raisins, apricots), lentils, beans, potatoes, spinach, broccoli, avocados and bananas.
Current recommendations in different guidelines
The 2020 International Society of Hypertension Global Hypertension Practice Guidelines recommend reducing the quantity of salt added when cooking and at the table, and to avoid or limit the consumption of high salt containing foods, such as fast foods, soy sauce and processed food (including breads and cereals). They also recommend population-based efforts to reduce salt intake and encourage consumption of fresh vegetables and fruits [17].
The 2018 European Society of Cardiology Hypertension Guidelines [2] and the WHO 2020 statement [3] recommend that sodium intake should be limited to <2 g per day (equivalent to <5 g salt per day) in the general population as well as in hypertensive patients.
Plan of action
A reduction in salt consumption should be a public health priority that requires collaborative efforts between governments, food manufacturers and the general population [2].
WHO proposed a plan of action to reduce salt intake globally by a relative 30% by the year 2025. To achieve this target, they recommend introducing regulations for food manufacturers to produce healthier and lower salt containing food and they also recommend increasing consumer awareness about the risks of high salt consumption and the healthier alternatives [3].
Conclusion
High salt intake is deleterious to the cardiovascular system both in normo- as well as in hypertensive individuals. Many food products contain salt, and one should be aware of the salt content in their diet to avoid high consumption. The association between high salt intake and hypertension is well established and all guidelines recommend reducing dietary salt as one of the proven measures to reduce high blood pressure. It is recommended to limit salt consumption to moderate amounts as too little salt in a diet may lead to adverse cardiovascular events. Population-based campaigns should increase the public awareness about the risks of high dietary salt and about the available measures to replace an unhealthy diet with a healthier one.















