Introduction
Hypertension is the leading cardiovascular risk factor in women worldwide [1], with increasing evidence that the physiological changes women experience over their lifetime, the trajectory in blood pressure increase is steeper for women. Control rates among people with hypertension were, on average, 23% for women and 18% for men, with the worst control rates (< 10%) in the lowest income countries. Although the absolute number of people diagnosed with hypertension has doubled, control rates have not changed over the past thirty years.
Despite women having greater awareness and greater use of antihypertensive medication, they have poor control of blood pressure (BP). Recent data from Canada report a worsening of hypertension awareness and treatment over the past decade for women [2]. There are important sex differences in the change in BP over the course of a lifetime: from early age onwards there is a steeper rise in BP in women that can start as early as the third decade [3]. This may have clinically relevant consequences for sex differences concerning the impact of hypertension on the development of coronary artery disease and heart failure.
Symptoms accompanying the rise in blood pressure
In middle-aged women the onset of hypertension may cause a variety of symptoms that are often mistaken for menopausal complaints. Arrythmias, such as palpitations, paroxysmal tachycardias and atrial fibrillation are frequently reported. Shear stress on the vascular wall can provoke chest pain, radiation to the jaws and pain between the shoulder blades. Other common symptoms are headaches, loss of energy, insomnia, fluid retention and shortness of breath at exercise. In elderly patients with extensive vascular stiffness, hypertension is more often asymptomatic. Specific attention is needed for women with prior hypertensive disorders during pregnancy, who often have hypertension present among family members. Many of these high-risk women develop hypertension in their forties and should be monitored more frequently than is currently happening in clinical practice [4].
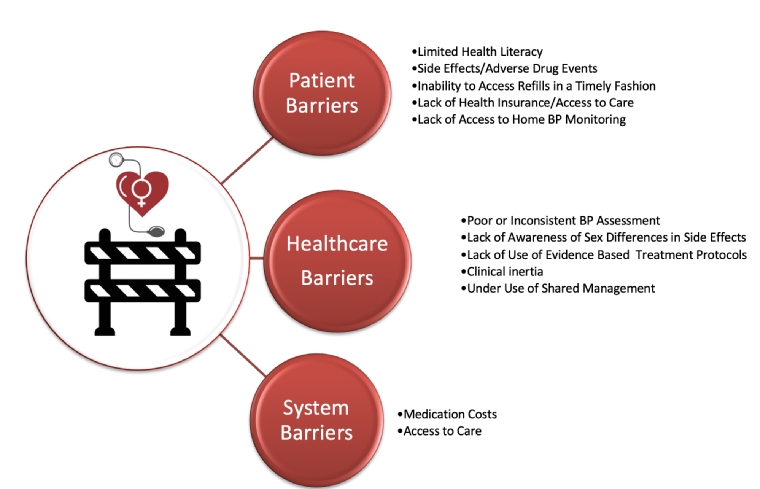
Understanding the barriers to treatment & control of hypertension
Health literacy, medication adherence and persistence
Limited health literacy, adherence and poor persistence to antihypertensive medication contribute to poor control of blood pressure. Health literacy (HL) involves the personal skills and motivation a person needs to acquire and understand in order to use the information and services that can help them make the most appropriate decisions regarding their health [5]. Adherence measures whether the person is conforming to recommended daily treatment, whereas medication persistence refers to whether they continue taking their medication [6]. Limited HL is independently associated with uncontrolled BP [7], although there are very few studies that examine sex differences in the relationship between HL and BP control with disparate outcomes. In one report, women had more limited HL than men, however their knowledge of health was higher than men [8], while another found HL more limited in men than in women [9]. There are also differences in the reporting of adherence, i.e., with no association between sex and adherence, [10] or women having lower adherence to antihypertensive medication than men [11]. Concerning medication persistence, women usually have higher rates although this changes in resistant hypertension to men having higher persistence [12].
Accurate measurement of blood pressure
How BP is measured contributes to how adequately hypertension is controlled. While measurement of BP in the clinic continues to guide management, adherence to guideline recommendations for accurate BP assessment continues to be suboptimal [13]. Further, women experience “white-coat effect” more than men [14]. If women have experienced pre-eclampsia or hypertension during pregnancy, they have a greater risk of permanent hypertension and need to be monitored even though they may have normal BP in the clinic following delivery. Hence, out of clinic measurements by ambulatory blood pressure monitoring (AMBP) or home BP measurements (HBPM) are recommended. While ABPM is considered the gold standard, referral of women may be delayed due to the physicians’ perception that there is low risk [14]. The various hypertension guidelines also recommend repeated HBPM. Further HBPM motivates patients for better treatment and has a beneficial effect on long-term medication adherence.
Sex differences in response to antihypertensives
It is estimated that women are 50-70% more likely than men to suffer from adverse drug reactions and side effects when compared with men, with women accounting for 60% of hospitalisations due to adverse drug reactions [15]. There are well-established sex differences in the pharmacokinetics of antihypertensive medications, accounting for the potential for an increase in side effects from these medications in women. Numerous sex-based factors influence the bioavailability and distribution of drugs, including increased body fat composition in women, lower body mass, circulating plasma volumes, the amount of plasma protein binding the drug, and differences in enzymes that metabolise certain drugs. As a result, drugs that are lipid soluble have a longer half-life in women, drugs that are water soluble result in higher exposures in women, and drugs that are metabolised by specific enzymes may differ by sex. Additionally, renal clearance is usually higher in biological men than biological women, also accounting for differences in bioavailability.
Specifically, studies have demonstrated that women have more adverse events with renin angiotensin aldosterone system (RAAS) inhibitors, as well as more side effects to angiotensin converting enzyme inhibitors (ACEi) [16]. Similarly, women have more adverse drug events associated with calcium channel blockers, loop diuretics, thiazine diuretics, and potassium sparing agents [16]. Men report more side effects to mineralocorticoid receptor antagonists (MRAs). The response to beta blockers differs by sex and for the same dose of a beta blocker, the heart rate and blood pressure response is greater in women than in men, with higher plasma concentrations of these drugs seen in women [17]. For nitrates and hydralazine there have not been any reported sex difference in responses or side effects to these agents (Figure 1).
Figure 1. Sex differences with antihypertensives medications.
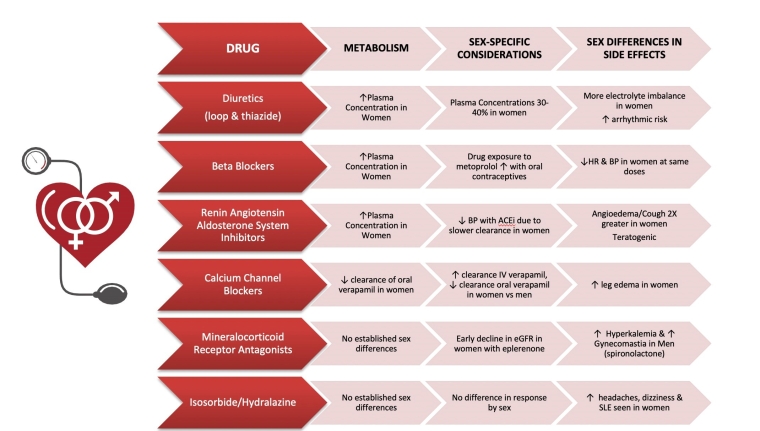
ACEi: angiotensin converting enzyme inhibitor; BP: blood pressure; eGFR: estimated glomerular filtration rate; HR: heart rate
Interestingly, despite more adverse drug events and side effects seen in women, a study from the Swedish primary care cardiovascular database has demonstrated that discontinuation of antihypertensives was more common in men, rather than women [18]. Such findings could be a confounder as to why there are more noted adverse drug events seen in women. Despite this, women over the age of 65 are less likely to have controlled blood pressure, and certainly medication intolerance may be one reason.
Impact of socio-demographics & social determinants of health
The association between social determinants of health (SDOH) and hypertension and hypertension control is well established. The National Health and Nutrition Examination Survey (NHANES) from 2011-2018, demonstrated that for both men and women, having no routine place for health care and being uninsured was associated with a lower prevalence of controlled BP [19]. Interestingly, unemployed or unmarried women were associated with better blood pressure control than women who were either employed or married. Independent of sex, the Black race was associated with a lower prevalence of blood pressure control. A study from Kenya demonstrated that when there are efforts to improved SDOH - specifically poverty and access to care - BP control can improve [20]. In this study, patients who received microfinancing combined with group medical visits demonstrated a 44% reduction in systolic BP, compared to standard care for persons with hypertension and diabetes.
Conclusions
Control of high BP is the highest priority for reducing the burden of cardiovascular disease for women, especially those with HDP. Adopting a shared decision approach with your female hypertensive patients will encourage, motivate and empower them in their health self-management. This includes assessing health literacy to personalise management and provide appropriate information support. Providing validated BP monitoring devices supported by telemonitoring will improve compliance by allowing medication adjustments to prevent adverse side effects. There also needs to be systemic changes to provide access to affordable medication. Continued monitoring, both by the individual and the healthcare team, lead to better control of hypertension (Figure 2).
Figure 2. Barriers to treatment & control of hypertension in women.
Take-home message
- Use validated BP monitors in both the clinic and home to measure BP
- Assess health literacy, cultural sensitivities and medication payment problems
- Refresh knowledge of the sex differences in pharmacokinetics of antihypertensive medications; be prepared to de-prescribe when clinically indicated
- Heightened attention is warranted in women after hypertensive disorders of pregnancy
- Incorporate lifestyle modifications such as increase in physical activity and weight reduction as part of the treatment plan















