Take-home messages
- CABG is still the preferred revascularisation modality for patients with diabetes.
- Hybrid coronary revascularisation is an effective revascularisation strategy with proven safety and efficacy for diabetes patients with multivessel coronary artery disease.
- The coronary artery anatomy dictates the suitability for hybrid coronary revascularisation, and a multidisciplinary Heart Team approach is crucial for managing complicated coronary artery disease.
Abbreviations
CABG coronary artery bypass graft
CAD coronary artery disease
DES drug-eluting stents
HCR hybrid coronary revascularisation
LAD left anterior descending
LITA left internal thoracic artery
MI myocardial infarction
MACCE major adverse cardiac and cerebrovascular events
MVCAD multivessel coronary artery disease
PCI percutaneous coronary intervention
Introduction
Diabetes mellitus is prevalent among adults worldwide [1]. The projected increase in mortality related to this disease affects societies around the globe. Patients with diabetes are susceptible to developing diffuse atherosclerotic disease involving multiple arteries [2]. Diabetic patients also constitute an increasing group of individuals who experience worse overall outcomes for coronary revascularisation. Hence, optimising revascularisation strategies for diabetic patients with multivessel coronary artery disease (MVCAD) is essential to preventing thrombotic complications. The goal of this manuscript is to examine the literature and critically assess the outcome of various revascularisation methods, with a focus on hybrid coronary revascularisation (HCR), to elucidate the optimal revascularisation modality for diabetic patients with MVCAD.
The evolution of revascularisation strategy in patients with diabetes
Globally, around 25% of patients with MVCAD who undergo coronary revascularisation have diabetes [3]. Several studies have demonstrated the benefit of coronary artery bypass graft (CABG) surgery with the use of the arterial conduit, mainly left internal thoracic artery (LITA) graft bypass to the left anterior descending (LAD) artery, to treat MVCAD in patients with diabetes. In this group of patients, CABG offers improved survival, reduced risk of myocardial infarction (MI) and repeat revascularisation, compared with percutaneous coronary intervention (PCI).
Increased interest in multivessel PCI in the 1990s led to trials comparing CABG versus PCI. These included the Emory Angioplasty versus Surgery Trial (EAST), the Coronary Angioplasty versus Bypass Revascularisation Investigation (CABRI), the Bypass Angioplasty Revascularisation Investigation (BARI), and the Randomised Intervention Treatment of Angina (RITA)-I trial. However, very few patients with diabetes were enrolled in these trials.
The landmark BARI trial showed that patients with diabetes who underwent CABG to treat MVCAD had a mortality benefit over percutaneous balloon angioplasty (PTCA) [4,5]. Based on this finding, CABG, in addition to optimal medical therapy, was recommended as the preferred approach for revascularisation in patients with diabetes [6,7]. Overall, studies for coronary revascularisation with PCI or CABG have not covered the entire spectrum of patients with coronary artery disease (CAD) and diabetes. Variations in clinical presentation, the complexity of CAD and how these variables affect outcomes in patients with diabetes have not been thoroughly investigated. Nevertheless, current data still suggest complete revascularisation as the ideal therapeutic option for diabetic MVCAD. The Arterial Revascularisation Therapies Study (ARTS) trial, designed to compare CABG and PCI in MVCAD, showed no difference in the incidence of mortality, stroke, or myocardial infarction between PCI and CABG at five years. However, there was a higher overall incidence of major adverse cardiac and cerebrovascular events (MACCE) in the PCI group, driven by the increased need for repeat revascularisation [8].
The Future Revascularisation Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease (FREEDOM) multicentre trial randomised 1,900 patients with diabetes and MVCAD to either CABG or a PCI strategy. In this study, patients in the CABG arm had a lower composite outcome of death from any cause and nonfatal MI, with a higher stroke rate during 5 years of follow-up, compared to PCI with drug-eluting stents (DES) [9].
Consistently, a subgroup analysis of patients with diabetes and MVCAD randomised to either PCI or CABG in the SYNTAX trial demonstrated a survival benefit with CABG [10]. A recent meta-analysis of eight randomised controlled trials (RCT) assessed a total of 3,612 patients with diabetes and MVCAD and compared outcomes between PCI and CABG. This study showed that during a 5-year follow-up, CABG had lower all-cause mortality than PCI, regardless of the type of stent used [11]. Importantly, CABG was associated with a higher stroke rate in virtually every comparative trial.
Overall, these studies suggest that despite the advances of modern PCI with newer-generation DESs and optimal medical therapy, revascularising patients with diabetes and MVCAD with CABG reduces long-term mortality. Therefore, CABG should still be strongly considered for these patients. Hence, defining the subset of patients with diabetes and MVCAD that would potentially benefit from PCI and the potential role of HCR is essential in managing these patients.
The hybrid strategy for coronary artery disease
HCR is defined as the combination of PCI and minimally invasive CABG for MVCAD. As previously described, patients with diabetes benefit the most from complete revascularisation with CABG, especially when a left internal thoracic artery to left anterior descending artery bypass is used [4]. Therefore, currently PCI is mostly reserved for patients with diabetes who are not acceptable surgical candidates. More recently, HCR has been shown to be a viable option, as it may provide the benefits of both CABG, most commonly with left internal thoracic artery to left anterior descending artery bypass, and PCI to the non-LAD vessels, while avoiding some of the intrinsic complications associated with each procedure.
HCR was first described in 1996 [12] by combining PCI with a minimally invasive CABG, in which the LITA was harvested and anastomosed to the LAD. This strategy provided the survival benefit of CABG, with left internal thoracic artery to left anterior descending artery anastomosis, while minimising the aggressivity of a complete multivessel CABG by completing the revascularisation with PCI to non-LAD arteries. Compared to CABG, HCR has similar short‐ and long‐term outcomes and demonstrates faster recovery and a shorter hospital stay. The subset of patients that appear to benefit the most from HCR are patients with MVCAD with a complex proximal LAD lesion (characterised by a SYNTAX score >34), suitable for left internal thoracic artery to left anterior descending artery bypass grafting, and significant but not overly complicated non-LAD lesions (SYNTAX score <22), suitable for PCI.
Outcomes of hybrid coronary revascularisation
Previous reports have focused on the safety and clinical outcomes of HCR in comparison to multivessel PCI or CABG. Of note, most studies are single-centre, retrospective, non-randomised case series. To date, the only multicentre randomised clinical trial comparing HCR with PCI was terminated prematurely due to slow enrolment [Table 1].
Table 1. Summary of major studies comparing HCR, CABG and PCI.
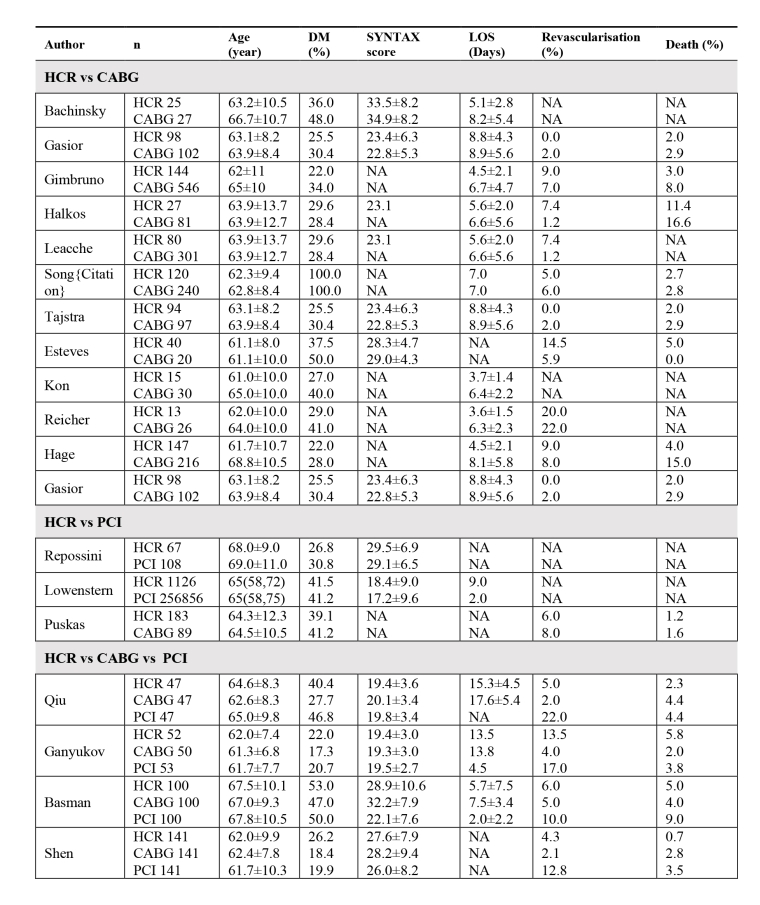
Values are mean, mean±SD, mean (range). DM: diabetes mellitus; HCR: hybrid coronary revascularisation; CABG: coronary artery bypass graft; PCI: percutaneous coronary intervention; SYNTAX: Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery; LOS: length of stay; NA: not available.
HCR vs CABG
Studies have compared HCR with different techniques of CABG. Overall, most studies consistently demonstrated superior perioperative safety metrics favouring HCR. Meta-analyses have demonstrated shorter ventilation time, fewer transfusions, reduced chest tube drainage, and a shorter ICU length-of-stay (LOS). Perioperative complications such as atrial fibrillation, renal failure, perioperative MI, or mortality were not significantly different [13,14].
Several studies reported similar rates of MACCE between HCR and CABG during short-term follow-up [15-18]. An important retrospective study by Leacche et al analysed the 30-day outcomes of 381 consecutive patients who underwent CABG (n=301) and HCR (n=80), stratified using the SYNTAX score (<32 vs >32) and the European System for Cardiac Operative Risk Evaluation score (euroSCORE) (<5 vs >5). Similar rates of MACCE were observed in all groups except the high SYNTAX/euroSCORE group (CABG 0% vs HCR 33%; p=0.001), driven by increased mortality associated with HCR. Based on this finding, HCR has been proposed to be a safe option for low-risk patients, while CABG might offer superior outcomes for more diffuse and complex CAD (higher SYNTAX score) or high clinical risk profiles (higher euroSCORE) [19].
Several studies have assessed the long-term outcomes of HCR and CABG in patients with MVCAD. In an earlier single-centre case series, Halkos et al reported that despite similar perioperative complications and MACCE during a 3-year follow-up, patients treated with HCR had numerically higher repeat revascularisations than off-pump CABG (7.4% vs 1.2%; p=0.09), consistent with the ARTS and SYNTAX trials. HCR was associated with a significantly lower in-hospital morbidity (8.5% vs 15.5%; p=0.005) and comparable mortality at 3-year follow-up (8.8% vs 10.2%; hazard ratio [HR] 0.91, 95% confidence interval [CI] 0.55-1.52; p=0.72) [20]. Tajstra et al [21] studied the 5-year all-cause mortality. The rates of MI, repeat revascularisation, stroke, and MACCE were similar in both PCI and CABG groups. MACCE was comparable between groups when stratified by the euroSCORE or SYNTAX score. Giambruno et al followed 147 patients for a median of 96 months. These patients were compared with 682 patients who underwent on-pump CABG with a median follow-up of 70 months. The adjusted analysis, not stratified by SYNTAX score, showed no statistically significant difference in survival or revascularisation.
HCR vs PCI
In a multicentre prospective study (38.6% diabetic patients) comparing HCR and multivessel PCI, the adjusted MACCE free survival was comparable at 12 months (HR 1.063; p=0.80) and 17 months (HR 0.868; p=0.53) [22]. Following the above preliminary study, the National Heart, Lung, and Blood Institute (NHLBI) sponsored the HYBRID trial, designed to compare HCR and PCI with DES for MVCAD.
This study was terminated due to slow enrolment. In a recently published case series, Repossini et al compared HCR vs PCI in patients with MVCAD involving the left main. 198 patients with comparable SYNTAX scores (around 29) were treated with either HCR or PCI. Mortality was not statistically different (p=0.6) at 30 days. MACCE-free survival at 18 months was significantly higher in the HCR group, driven by freedom from target vessel revascularisation (93.3 ± 4.6% vs 75.5±5.6; p=0.002) [23].
HCR, CABG and PCI, the three-way comparison
The HREVS trial was a prospective RCT assessing the efficacy of various modalities by evaluating residual ischemia using SPECT perfusion imaging. MVCAD patients with comparable SYNTAX scores (19.4±2.9) who were deemed to have equal angiographic and clinical feasibility for CABG, HCR, or PCI were randomly assigned to the three arms. At 12 months, there was no significant difference in residual ischemia (CABG 5%, HCR 5%, PCI 6%) [24]. Another retrospective study by Qui et al included the SYNTAX score as a covariant in the propensity matching process with comparable scores in three arms (HCR, CABG and PCI 19.4±3.5, 20.3±3.2 and 19.9±3.1, respectively). There was no statistical difference in the rate of freedom from MACCE at five years between HCR and CABG (11.4 vs 13.3%; p=0.778), but there was a reduced rate of MACCE with HCR when compared with PCI (11.4 vs 35.6%; p=0.007) [25].
A recent study evaluated 100 propensity-matched patients who underwent HCR and were compared to either CABG or multivessel PCI. The baseline SYNTAX score was significantly higher in CABG arm than in HCR arm (32.2±7.9 vs 28.9±10.6, respectively; p=0.018), and it was higher in the HCR patients than in the PCI only group (28.9 ±10.6 vs 22.1±7.6; p<0.01). There was no significant difference in the residual SYNTAX score between the HCR arm (4.5±4.4) and the CABG arm (5.2±4.7; p=0.31). However, despite a higher baseline SYNTAX score, the residual SYNTAX score was significantly lower in the HCR than PCI (4.5±4.4 vs 7.1±6.5, respectively; p=0.001). Overall, patients who underwent HCR had similar 8‐year mortality (5.0%) when compared to CABG (4.0%) or multivessel PCI (9.0%). A composite endpoint of death, repeat revascularisation, and new MI was not significantly different among groups (HCR 21.0% vs CABG 15.0%; p=0.36; HCR 21.0% vs PCI 25.0%; p=0.60) [26]. Based on this finding, HCR should be considered for patients with MVCAD when a low residual SYNTAX score can be achieved.
HCR in diabetic patients
Diabetic patients consist of a significant portion of the population in the above studies. However, studies focusing solely on the diabetic population are limited. Harscamp et al compared the outcome of 103 HCR and 515 CABG patients in a propensity score-matched fashion. While repeat operation and renal failure were comparable in these two arms, HCR demonstrated significantly fewer blood transfusions, chest tube drainage and shorter lengths of stay. At 3-year follow-up mortality was comparable [27]. Song et al retrospectively studied 120 diabetic patients who underwent HCR and were propensity-matched to 240 CABG patients. Comparable MACCE was noted over 30 months, but a significant lower stroke rate was noted in HCR (0% to 3.6%; p=0.046) [28].
Conclusion
Diabetes has significant cardiovascular mortality and morbidity. In addition to optmal medical management, complete revascularisation is associated with improved outcomes for patients with MVCAD. Recently, HCR has emerged as an alternative option to traditional CABG. By combining CABG and PCI, HCR retains the benefit of CABG with an arterial conduit to LAD, while significantly reducing the perioperative complications. Patients who benefit from this strategy are those with multivessel disease with complex proximal LAD lesions suitable for LITA-LAD grafting and non-LAD lesions amenable for PCI. Existing data demonstrate comparable in- and out-hospital outcomes. Compared to multivessel PCI, HCR is superior in reducing repeat revascularisation in selected patients. Compared to conventional CABG, for low to intermediate complexity patients (SYNTAX score <20), HCR demonstrated comparable target vessel revascularisation rates and improved hospital outcomes.















