Take-home messages:
- Airborne pollution is deleterious for the cardiovascular system
- Airborne pollution is present both in- and outdoors
- Airborne pollution triggers and empowers deleterious cardiometabolic risk factors
- Exercise should be discouraged in strongly polluted conditions
Background
Fine particulate matter (PM)(≤2.5 μm in diameter [PM2.5]) is likely the uttermost environmental threat to health [1]]. PM2.5 plays a role in a large variety of noncommunicable diseases. However more than 50% of the deaths related to such diseases are cardiovascular [1]. Taken together, outdoor and indoor air pollution threaten health to a larger extent than soil contamination, water pollution, and occupational pollution [1].
Outdoor pollution
The most defenceless air pollution victims reside in middle- and low-income countries. Fossil fuel combustion, industrial power generation and manufacturing are the main sources of PM2.5 [1]. More recently, climate changes have further exposed rural areas and their inhabitants to the smoke of extensive and long-lasting wildfires, often spanning more than several hundred kilometres. These new threats exert cardiovascular effects that are PM2.5-alike [2]. As such, the risk of ischaemic heart disease has increased fivefold with coal combustion-derived PM2.5 than with the total PM2.5 [3]. These observations, among many others, underscore the urgent need to diminish fossil fuel combustion, especially coal burning.
Indoor pollution
Indoor air is often problematic as well. Almost two-thirds of airborne PM are inhaled while people are indoors [1,4]. Seasonal wood burning, whether for heating or recreational purposes, induces intense PM exposure worldwide. In middle- and low-income countries, cooking with biomass fuel is a significant source of intoxication [4]. Whereas in high-income countries, burning candles and incense, aerosol sprays and various vapours from cleaning products together with emissions from gas stoves release PM [1,4]. Compared with clean energy, solid fuels increase cardiovascular mortality by one-third and all-cause mortality by more than one-tenth [5].
Cardiovascular effects of PM
The cardiovascular effects of PM2.5 inhalation are mediated by multiple processes. Pollution-mediated oxidative stress and inflammation are initiated in the lungs [6,7]. These, in turn, induce endothelial dysfunction, vascular inflammation, coagulation and thrombosis, plaque instability, cardiac arrhythmia and epigenomic changes [1,8]. Repeated exposure to PM2.5 can trigger, empower and exacerbate the deleterious effects of well-known cardiometabolic risk factors (such as hypertension, dyslipidaemia, diabetes, etc.) and thereby accelerate the progression of atherosclerosis and end-organ damage [9].
PM pollution and the exercising patient
From a cardiologist’s perspective, one could wonder if inhalation of large amounts of PM2.5 negates the favourable effects of physical exercise on cardiovascular health. Evidence of deleterious consequences of exercise on pulmonary function and inflammation, blood pressure and vascular function suggests that exercise should be discouraged in strongly polluted conditions [10,11,12].
The future might become greyer...
An additional important matter of concern is that fossil fuel combustion, greenhouse gas emissions and climate change are mutually reinforcing (Figure 1). Rising temperatures and extreme weather conditions elicit sharp increases in environmental pollution by means of wildfires, floodings and hurricanes, which, in turn, increase PM levels, carbon monoxide and ground-level ozone gas [13,14,15].
Conclusions
Fine PM is a ubiquitous, silent and growing worldwide threat to cardiovascular health. Airborne pollution induces endothelial dysfunction, vascular inflammation, coagulation and thrombosis, plaque instability. It triggers, empowers and exacerbates the deleterious effects of well-known cardiometabolic risk factors (such as hypertension, dyslipidaemia, diabetes, etc.), and thereby accelerates the progression of atherosclerosis and end-organ damage. Until further data are available, exercise should be discouraged in strongly polluted conditions.
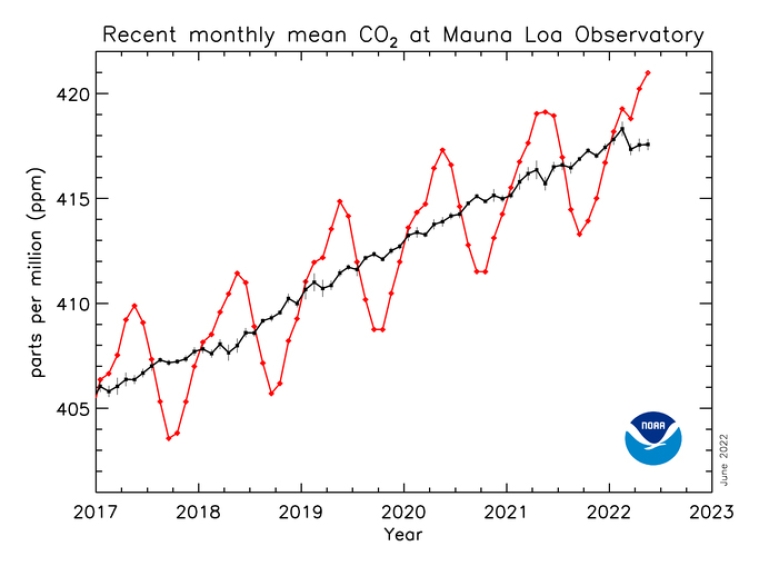
Figure 1. Trends in atmospheric carbon dioxide.
The graph below shows monthly mean CO2 measured at Mauna Loa Observatory, Hawaii. CO2 continued to rise during the world-wide COVID-19 pandemic shut-down (growth rate in ppm/year: 2018: 2.85; 2019: 2.49; 2020: 2.31; 2021: 2.38) [16].