Introduction
The disease originated by the SARS-CoV-2 virus has infected about 24,428.88 million people around the world, causing about 524 million deaths [1]. In addition, a great number of comorbidities and complications persist after recovery in hospitalised patients. COVID-19 survivors present diverse sequelae, the most outstanding of which include pulmonary dysfunction, chronic illness, and physical limitations [2,3], as well as neurologic, psychological, and cognitive alterations [4,5].
Heart rate variability as a viable means of assessing autonomic function
It has been observed that patients affected by COVID-19 present sympathetic hyperactivity which generates increased production and release of cytokines [5]. These proteins trigger major disturbances in the respiratory system but can also affect the cardiovascular system [6]. This damage continues after discharge from the hospital. In addition, survivors also manifest peripheral alterations from imbalances in the brain and the autonomic system. These include vagal function and other elements of the system [7] that, together with other biochemical alterations, generate greater dysautonomia [6]. Moreover, the systemic impact on other organs and tissues increases the risk of worsening health and a less complete recovery [4].
A non-invasive method of evaluating autonomic function is the use of such biomarkers as heart rate variability (HRV), which is associated with changes in the relaxation and stress status of individuals [8,9]. This biomarker reflects the interaction of the respiratory, cardiovascular, and neurologic systems. Its evaluation is not only associated with different aspects of autonomic function, but also with aspects of cardiovascular and neurologic health [10]. HRV is a physiological response that is sensitive to the autonomic changes observed to be altered in diverse medical conditions, including infectious and immune diseases [11].
HRV is defined as the time variation that occurs in the interval between heartbeats (microseconds). When the organism confronts diverse situations, HRV is conditioned for the respiratory process of inspiration and expiration and depends on autonomic modulation. HRV analysis is an effective, rapid, and non-invasive tool to evaluate the autonomic response in a quantitative way [6,12,13].
There are different methods for the data analysis of HRV. The most common is density power spectrum analysis, also known as spectral analysis. This technique measures the changes in the heart rate in the frequency domain and makes it possible to see the rhythms and the components that form the total rhythm of heart activity. The spectrum division in bands can be used to quantify the potential of each one, or to determine the frequency relationship between bands, each one of which has a specific physiologic correlation [13]:
- High Frequency (HF) band. This has a rank of between 0.15 and 0.4 Hz. It is related to the modulation of the efficacy of gas exchange, respiratory sinus arrythmia, parasympathetic nervous system activity and innervation of the vagus nerve.
- Low Frequency (LF) band. Its rank is between 0.04 and 0.15 Hz. This band is influenced by the sympathetic nervous system, including the parasympathetic component, and is also associated with the activity of baroreflex function.
- Very Low Frequency (VLF) band. Between 0.0033 and 0.04 Hz, it is linked to parasympathetic deactivation, the influences of thermic and visceral regulation, and activity in the renin-angiotensin-aldosterone system [12,13]
COVID-19 and its psychophysiological sequelae
Hospitalised patients with SARS-CoV-2 infections who present a decrease in HRV, particularly in the high frequency domain [6], have been found to have worse prognoses. It is noteworthy that with dysautonomia, stress (physiological and psychological), and the adaptations that are generated by the acute viral period, psychological disturbances are common. It has been observed that survivors of different types of coronavirus infections have presented symptoms related to diverse mental illness such as anxiety, depression, panic disorder, post-traumatic stress disorder and obsessive-compulsive disorder during their recovery period or even up to 50 months afterwards [9,10].
Although at present there is little research focusing on the psychological effects specific to COVID-19 survivors, it has been reported that there is a high prevalence of symptoms associated with anxiety, insomnia, depression, post-traumatic stress disorder (PSD) and obsessive-compulsive disorder (OCD) [9]. These alterations are the result of the interrelationship between the nervous and immune systems, which, in conjunction with the psychological stress generated by the disease, can induce psychiatric symptoms during recovery [5,9].
HRV has been associated with different aspects of health and is a predictor of morbidity and mortality in many conditions [14]. For example, in patients with cardiorespiratory illness, due to the alteration in responses such as heart rate and the inability to breathe properly, HRV is often decreased and associated with a higher mortality rate [14]. Moreover, HRV is also a factor involved in mental health. Some psychological alterations such as anxiety and depression impair the modulation of the autonomic nervous system, and cause this biomarker to decrease [15]. For example, patients with cardiovascular imbalances that present symptoms associated with anxiety also present the lowest levels of HRV compared to patients with the same illness without anxiety [16].
The autonomic alterations generated by chronic or infectious illness also manifest effects on the central nervous system due to sympathic-vagal imbalance [17]. This has consequences such as cognitive impairment that tends to intensify when cardiovascular and autonomic dysfunctions coexist [18]. For this reason, individuals with low levels of HRV have been found to have the worst results in neuropsychological evaluations, especially involving attention and memory [19].
HRV alterations in COVID-19 survivors
One of our investigations into this topic included 434 COVID-19 survivors evaluated three months after their hospital discharge. Two general aspects were assessed. 1) A psychological evaluation focusing on anxiety, depressive symptomatology, and sleeping disturbances. 2) A psychophysiological evaluation measuring HRV in 4 phases: a) open eyes, b) closed eyes, c) natural relaxation, and d) induced relaxation through diaphragmatic breathing. To obtain the total level of HRV, the following formula was used: (VLF+LF)/HF. The results were classified into three groups: high HRV (0-0.89), medium HRV (0.90-1.1) and low HRV (>1.1), with the objective of identifying the proportion of sympathetic and parasympathetic activity, or the predominance of either of these.
The main results of this research are in agreement with other recent findings. These patients presented a high prevalence of chronic diseases such as systemic hypertension (32.6%) and diabetes (30.4%) [3,4], as well as psychological alterations such as anxiety (12.2%), depression (6.8%) and sleep disturbances (40%). Regarding the last, 41.5% of patients referred to having problems falling asleep or difficulty sleeping, 45% had continued awakenings, and 25.5% still experience recurrent dreams related to the virus or the hospitalisation.
From the psychophysiological point of view, 67-81% of these patients had low levels of HRV, and even during the phase associated with relaxation, just 13 to 28% presented high levels of HRV (Figure 1). This result could be explained by a possible autonomic disturbance or dysautonomia also associated with psychological aberrations. This is consistent with the findings in hospitalised COVID-19 patients [6] who presented decreases in the frequency domains compared to control subjects and the lowest HRV levels, which correlated with the worst health outcome [11].
Figure 1. Total level of heart rate variability in COVID-19 survivors during the psychophysiological test.
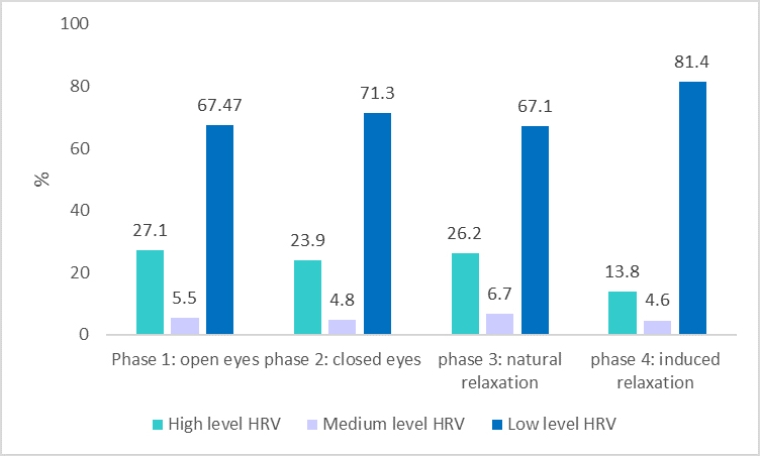
Note on figure: In all the phases of the test, most patients showed a low level of HRV (between 67% to 81%) In addition, patients showed a higher prevalence of this level during the “open eyes” and the induced relaxation phases. Moreover, a small proportion of them (between 13 % to 27%) showed a high level of HRV during all the phases, but saw an even sharper decrease during the relaxation induced phase, where it decreased to 13.8 per cent. The medium level of HRV was minimal in these patients (4% to 6%). These results can be associated with the presence of a possible autonomic disturbance, which the sympathetic overactivation can lead to lower HRV levels, a high cardiac involvement and, in consequence, a worsening health prognosis.
HRV: heart rate variability
Modulation of autonomic functioning through HRV biofeedback training
Different behaviour strategies exist to decrease autonomic hyperactivity and improve its modulation in order to improve quality of life and reduce comorbidities and mortality. One of these types of treatment is biofeedback training, a psychological and behavioural intervention technique. It is defined as a set of procedures focused on giving patients accurate and real time information about some aspect of their physiological responses, with the aim of teaching them to regulate or control these responses in a voluntary way [20].
HRV biofeedback training is an intervention with both long- and short-term results. Its effects can be seen in increased cardiac homeostasis, as well as baroreflex activity. This is because the stimulations generated through the vagus nerve and decreased sympathetic hyperactivity, induce a higher level of relaxation. This supports the modulation and control of the production and release of inflammatory cells. The outcome is an increased anti-inflammatory status and regulation in different systems such as the cardiovascular system [21], improved autonomic functioning, increased HF index and enhanced HRV levels. It can also increase emotional and behavioural regulation, and cognitive functioning and decrease psychological alterations such as anxiety, and depression in patients with different chronic diseases, including cardiovascular diseases [6,22].
The common protocol for HRV biofeedback training uses a diaphragmatic breathing practice that promotes a respiratory rate of 6 breaths per minute. Training six weeks with one visit a week. It involves biofeedback software that gives visual and auditory reinforcement when the patients achieve cardiac coherence and increased HRV, while it records their heart rate and their abdominal breath. In addition, they are provided with psychoeducation and/or cognitive-behavioural techniques for the treatment of emotional or cognitive conditions.
The application of this protocol has been shown to produce important changes in autonomic function assessed by HRV in patients with heart failure and other chronic diseases [22,23]. In one representative case, a female COVID-19 survivor with low HRV levels was selected for a psychophysiological evaluation, as already described. During the post-evaluation period, a different pattern was observed compared to the first evaluation (Figure 2). The percentage of high frequencies was increased in all the phases, while low frequencies were significantly decreased. Better modulation compared to the level was observed during the first evaluation, and higher HRV levels were evident in all the phases. The findings of this patient are consistent with the results reported in patients with other chronic diseases that used the same HRV biofeedback training protocol [22,23], with comparable long-term changes.
Figure 2. Frequency spectrum of heart rate variability at baseline and during the post-evaluation period (COVID-19 survivor).

Note on figure: This figure shows the frequency spectrum of HRV in a COVID-19 survivor during a psychophysiological test. In blue the first evaluation before starting the HRV biofeedback training is seen, the percentage present in each frequency component; the HF decreased in all phases (14 to 28%) also, the VLF showed a higher percentage in all the phases (32% to 50%), and the LF presented a high percentage during the first and last phase (44.1% and 31.57% , respectively), but showed an important decrease during the second phase (16.04%) and a moderate decrease in the third phase (22.24%). Moreover, the second evaluation after the end of the HRV biofeedback training demonstrated a higher HF percentage in all the phases (46 to 66 %) showing the largest increase during the third phase (natural relaxation), while the VLF presented a percentage diminished (8% to 16%) in all the phases. The LF, although it had a low percentage during the first three phases (14.16%, 20.06% and 6.83%, respectively), in the last phase (natural relaxation) this frequency showed a slight increase (34.86%). The results prove that the HRV biofeedback training manages to improve the autonomic functioning and generate a better sympathetic-vagal and cardiovascular regulation.
HF: high frequency; HRV: heart rate variability; LF: low frequency; VLF: very low frequency
COVID-19 survivors present autonomic alterations very similar to those of patients with chronic or cardiovascular diseases. Consequently, they can benefit from a treatment such as HRV biofeedback with equally promising results.
Given the findings reported, it is of interest to know the psychophysiological status of COVID-19 survivors. This would not only make it possible to evaluate the autonomic and emotional disturbances of these patients but would also provide a means of detecting alterations that could jeopardise recovery. Moreover, it would allow the creation of different multidisciplinary therapeutic plans and provide the opportunity to test the efficacy of previously successful treatments in other patient populations. Heart rate variability biofeedback training that could help to decrease or prevent other comorbidities in this population.
Conclusions and take-home message
COVID-19 survivors present autonomic disturbances related to cardiovascular sequelae that can deteriorate in conjunction with concurrent physical and emotional sequelae. An evaluation of autonomic function not only provides information about this specific functional status but also offers a type of intervention that can decrease the deleterious impact of cardiovascular, autonomic, physical, and emotional alterations. HRV biofeedback training is a treatment that has been shown to be effective and capable of modulating HRV and enhancing the autonomic function of patients with chronic cardiovascular diseases. For this reason, it should be considered as part of the multidisciplinary treatment of COVID-19 survivors.















