Introduction
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is the RNA virus responsible for the COVID-19 pandemic [1]. The clinical features of COVID-19 infection can vary from one individual to another. In some, infection can be asymptomatic, while in others it can result in life-threatening heart and lung failure [2]. Any associated cardiac complication is considered detrimental to the survival of COVID-19 patients [1].
COVID-19 has various cardiovascular consequences including alteration in cardiac biomarkers (due to ischaemic or non-ischaemic causes), myocarditis, arrhythmia, cardiogenic shock, cardiac arrest, and thromboembolism. Ischaemic myocardial injury can result in myocardial infarction (ST- or non-ST-elevation), and myocardial injury with disseminated intravascular coagulation. Non-ischaemic myocardial injury gives rise to myocarditis, stress-induced cardiomyopathy and myocardial injury with cytokine release syndrome [3].
Myocardial injury
Factors associated with myocardial injury include age, presence of comorbidities, ferritin and fibrinogen levels and kidney, liver or other organ dysfunction, especially kidney injury. Thus, optimisation of organ dysfunction is a key point in the treatment of COVID-19 with myocardial injury [4].
Several theories have been put forward to explain the mechanism of myocardial injury including the complex interaction between hypoxaemia, ischaemia and the procoagulant state in the setting of pneumonia. The cytokine storm that results from uncontrolled viral infection can lead to acute coronary syndrome. Prior coronary disease leads to higher endothelial inflammation and can even cause plaque rupture. Viral infection can even activate the coagulation process and endanger the anticoagulant property of endothelium to form thrombus. Thus, by blocking the compromised cardiac blood flow, it further exacerbates the injury [6].
Injury of cardiac valves
The viral effect on cardiac valves has also yet to be fully understood and it is still questionable if COVID-19 can impair the function of the cardiac valves. Angiotensin-converting enzyme 2 (ACE2) acts as the gateway for the SARS-CoV-2 virus to the host cells. It is also widely seen in cardiac valves, especially the human aortic valve. Stenotic valves have an extensive abnormal expression of such receptors in macrophages. ACE2 cells in heart valves can be targeted easily by COVID-19 and can cause hindrance of normal blood flow in such valves. A cytokine storm can also indirectly damage the cardiac valves. Thus, a periodic check-up of COVID-19 survivors with acquired heart disease must be encouraged [7].
Echocardiographic abnormalities
Myocardial injury and cardiac biomarker elevation have a higher prevalence of abnormal echocardiographic findings in approximately two thirds of patients undergoing transthoracic echocardiography. Specific abnormalities include ventricular wall motion abnormalities, right ventricular dysfunction, global left ventricular dysfunction, diastolic dysfunction, and pericardial effusion.
There is a higher likelihood of in-hospital mortality for patients with major echocardiographic abnormalities even after correction for other major COVID-19 complications. Thus, echocardiography can be a prognostic tool in troponin-positive patients. There is a multifactorial association between myocardial injury and mortality in such patients. Patients with myocardial injury may have clinically severe manifestations of COVID-19 and are more prone to deteriorate than others [8].
Electrocardiography variations
Manifest electrocardiographic abnormalities are associated with more severe clinical features in COVID-19. Serial electrocardiograms (ECGs) can also alert to worsening of lung infection.
Specific ECG changes associated with more serious adverse events include higher heart rate especially with a further rise at 7 days, probably due to the presence of serious infection or systemic inflammatory response. Likewise, low QRS voltages can be due to respiratory damage and a widened QRS complex due to heart injury. New-onset atrial fibrillation (AF) is also associated with an increased risk of major adverse events. A repeat ECG after one week may be of value to rule out further adverse outcomes with a definite association between seven-day ECG variations and the increased rates of intensive care, intubation, dialysis and mortality [9].
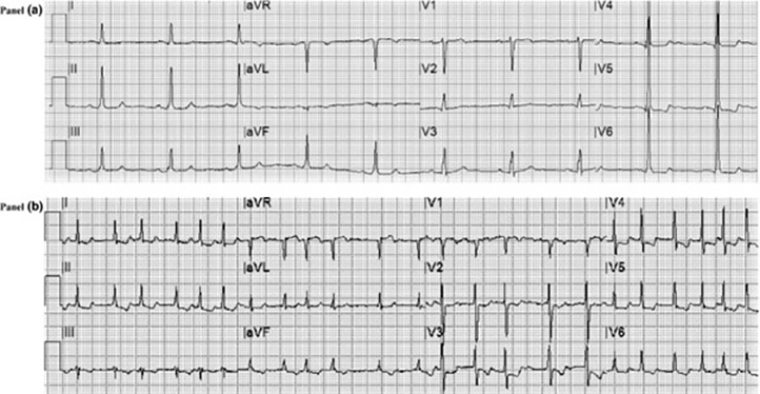
Figure 1. ECG alterations and major adverse events in COVID‐19. The value of ECG changes in the risk stratification of COVID-19 patients. From Bergamaschi et al [9].
Panel A.
Basal ECG of a patient with severe COVID‐19 with signs of left ventricular hypertrophy (according to the Sokolow-Lyon criteria with secondary ST‐T segment alterations) who had orotracheal intubation for worsening of respiratory failure with subsequent recovery.
Panel B.
ECG recorded at day 7 of hospitalisation showing AF with high ventricular rate response and ischaemic alterations (primary ST‐T segment alterations) in a patient who died due to respiratory failure.
Arrhythmias
Cardiac arrhythmias are frequent and may remain even after recovery from COVID-19. Arrhythmias such as AF, ventricular tachycardia and supraventricular tachycardia and complete heart block can appear in any phase of the disease (infective, recovery or post-recovery phase). Individualised care is the best approach for these patients [10].
Another mechanism of arrhythmias in COVID-19 is multi-drug usage and their interactions. The pro-arrhythmic state - dysfunction and altered drug clearance also increases arrhythmogenicity. Additionally, some drugs used for treatment for viral replication prolong the QT interval. Thus, torsades de pointes may occur in susceptible patients treated with chloroquine/hydroxychloroquine, lopinavir/ritonavir, macrolides (especially azithromycin) and fluoroquinolones. The latter two drugs are commonly used to treat bacterial superinfections in COVID-19 patients. Also, several of these patients have additional risk factors such as prior heart diseases, electrolyte abnormalities and usage of other QT-prolonging drugs such as anti-emetics, proton pump inhibitors, sedatives [11].
The most common arrhythmias in COVID-19-affected individuals are atrial arrhythmias which can be found in up to 17.7% of mechanically ventilated patients. The cause of death in most of these patients is asystole or pulseless electrical activity secondary to pulmonary embolus or lung failure [12]. The most common symptoms associated with arrhythmias are palpitations, syncope, dizziness, chest discomfort and fatigue which can manifest as stroke, thromboembolism, heart failure and sudden cardiac death. AF is a poor prognostic factor in those with acute respiratory illness. For rate control, diltiazem is preferred in COVID-19 patients as beta-blockers may precipitate bronchospasm in respiratory disease [10]. Ventricular tachycardia (VT) storm can present in patients in three ways – three or more ventricular tachyarrhythmias in one day, VT recurrence after cessation of another episode, or VT episodes (sustained and non-sustained) transcending normal beats within a day.
Myocarditis
In COVID-19, viral myocarditis is a common and important cause of myocardial injury and presents similarly to myocardial infarction with a rise of cardiac biomarkers, cardiomyopathy features on echocardiography and normal coronary arteries. Diagnosis of viral myocarditis is most commonly a clinical one but may require endomyocardial biopsy and histopathological examination. Alternative methods include identification of the SARS-CoV-2 genome in heart tissue or viral particles in cardiomyocytes [13, 14].
Post-vaccination myocarditis
In Israel, 62 cases of myocarditis were reported after COVID vaccine administration in five million individuals. In most cases these occurred after the second dose of mRNA vaccines. Young men are more affected, with two deaths in total. Fourteen cases of myocarditis were also reported in the United States Defense Department after administration of Pfizer-BioNTech and Moderna vaccines [15, 16].
Heart failure
Approximately a quarter of hospitalised COVID-19 individuals were diagnosed with new-onset heart failure, especially in intensive care admissions (one third of admissions) [17, 18]. An increase in natriuretic peptides is indicative of a worse prognosis.
Takotsubo cardiomyopathy
Also known as stress-induced cardiomyopathy, Takotsubo cardiomyopathy can present with acute ventricular dysfunction in a non-coronary distribution along with an increase in levels of troponin I and creatine-kinase. However, levels of interleukin-6, D-dimer and ferritin are higher in patients with non-Takotsubo myocardial injury. Vascular integrity is compromised by virus action and causes various myocardial abnormalities. Treatment is still controversial. However, ACE inhibitors, beta-blockers and diuretics are used in the treatment of such patients [1].
Cardiogenic shock
Cardiogenic shock due to cardiac tamponade, acute decompensated heart failure, acute myocardial infarction and fulminant myocarditis can be observed. Haemodynamic assessment including right heart catheterisation is very important in the recognition of cardiogenic shock [19]. Cardiac catheterisation is both therapeutic and diagnostic in cardiogenic shock following acute myocardial infarction.
Pericardial disease
Pericardial effusion and tamponade can occur as a consequence of COVID-19 infection. Transthoracic echo is important to rule out significant effusion, while cardiac magnetic resonance imaging (MRI) can visualise pericardial thickening or small effusions. Early controlled invasive treatment of large pericardial effusions is necessary to prevent haemodynamic derangement. This has to be dealt with carefully in those patients who need intubation and mechanical ventilation. Pericardial tamponade as a reason for unexplained worsening in COVID-19 patients always has to be ruled out [20].
Table 1. COVID-19 related Cardiovascular Conditions.
| Cardiovascular conditions | Treatment options |
| Acute Coronary Syndrome (STEMI or NSTEMI) | Primary PCI vs Elective PCI vs Fibrinolytic therapy |
| Azithromycin and/or HCQ, CQ use | Advise ECG during follow-ups to monitor QTc, avoid drugs that prolongs QTc |
| Controversy regarding the use of ACEI or ARB | Continue ACEI or ARB as we have not proper guidelines on this |
| Immunosuppression/Immunomodulation | It can be an option in those critically ill patients with cytokine storm |
| Mechanical Circulatory Support | Patients with cardiogenic shock - IABP and VA ECMO should be considered |
| Myocardial injury confirmed by rise in Troponin | Poor prognosis. There is a need to observe and to have serial ECG’s and Troponin levels to evaluate the trends. |
ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; CQ: chloroquine; HCQ: hydroxychloroquine; IABP: intra-aortic balloon pump; MCS: mechanical circulatory support; NSTEMI: non-ST-elevation myocardial infarction; PCI: percutaneous coronary intervention; STEMI: ST-elevation myocardial infarction; VA ECMO: veno-arterial extracorporeal membrane oxygenation
Take-home messages
- Cardiovascular complications of COVID-19 infection are a marker of poor prognosis.
- Early detection and surveillance of patients at risk of myocardial injury are essential in patients with COVID-19 pneumonia.
- Serial ECGs are helpful in identifying higher-risk patients.