Introduction
Accessory pathways (APs) are fibrous connections of myocardial tissue that allow direct electrical communication between the atrium and ventricle. An alternate pathway and independent of the regulatory atrioventricular (AV) nodal conduction system and Purkinje fibres, they are due to incomplete AV annular isolation during embryological development [1]. Single APs are significantly more common; however, multiple pathways are more complex and are associated with other cardiac abnormalities such as Ebstein’s anomaly [2].
Accessory pathways allow extra nodal conduction anterograde (atrium to ventricle), retrograde (ventricle to atrium) or both. They are named for the anatomical structures they connect but are further classified by their type of conduction (decremental or non-decremental) and direction of conduction (anterograde or retrograde) [2].
Anterograde conduction with an AP can allow depolarisation of ventricular tissue prior to the normal AV nodal stimulation, manifesting in a classical short PR interval ≤120 milliseconds (ms), followed by an up-slurring pre-QRS, known as a delta wave on the baseline sinus ECG [2,3]. These ECG findings describe “pre-excitation” and in the absence of associated tachycardia is known as the Wolff-Parkinson-White (WPW) pattern. This pattern may be constant, intermittent and of varying degree of pre-excitation depending on the characteristics of the pathway. When such a pathway permits a sustained atrioventricular reciprocating tachycardia (AVRT), this is then defined as WPW syndrome. That said, some APs with anterograde abilities may not manifest these ECG findings depending on conduction time or their remote location, such as the lateral left ventricle, which is far from the sinus and AV nodes. Exposure of these pathways is possible during an EPS by pacing manoeuvres or pharmacologic stimulation. Pathways conducting only anterograde are seen in <5 % of patients [2].
Retrograde conducting pathways lack baseline ECG distinguishing features, as such, they are referred to as concealed pathways. They result in orthodromic tachycardias which use the AV node and Purkinje fibres anterograde from the atrium to ventricle and traverse the accessory pathway retrograde back to the atrium, resulting in circus movement tachycardia [3]. During an EPS, this type of pathway is identified during ventricular pacing where extra-nodal V to A concealed conduction may result in an altered activation sequence, usually from concentric in sinus to eccentric. Other pacing manoeuvres are also required to further confirm the arrhythmia and rule out other similar tachyarrhythmias. Thankfully, most pathways conduct both anterograde and retrograde, allowing varied approaches to identification and treatment.
Other accessory pathways such as atriofascicular, nodofascicular, nodoventricular, and fasciculoventricular (Mahaim fibres) are less common but also result in variants of Wolff-Parkinson-White syndrome and may be seen in clinical practice [4].
Ablation techniques
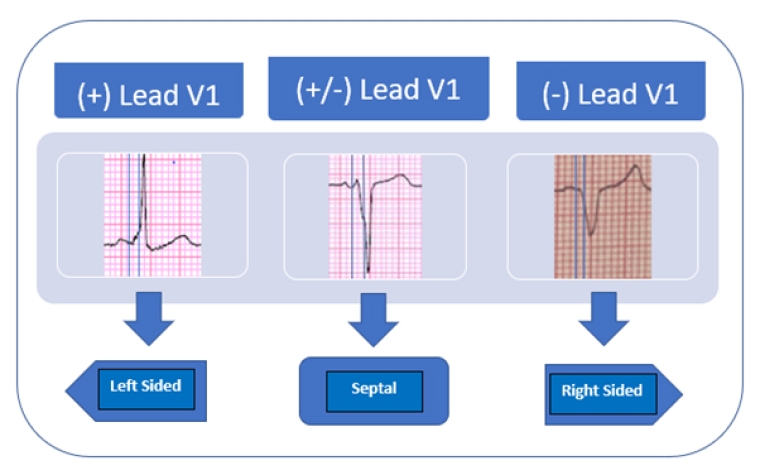
Preprocedural evaluation of baseline and tachycardia electrocardiograms (ECGs) allow proper planning of the EP study and ablation. Careful assessment of the morphology of the delta waves is used to anticipate the location of the pathway which can be in the left heart, right heart, or the septum. Several algorithms such as findings by the Arruda group have been validated to assist in identifying the location of the pathway and its implication in procedure planning. [5]. If an ECG demonstrated a positive delta wave in leads I, V1, and all three inferior leads, this would imply a left lateral pathway. This may lead operators to establish arterial access from the start of the procedure or plan a transseptal approach to access the left atrium and ventricle.
Figure 1. Simplified algorithm extracted from the Arruda article where the direction of the delta wave is used to predict the general location of an accessory pathway [4]. The different ECG patterns at defined lead V1 with the delta wave marked between the lines. (+) in Lead V1 indicating a left sided pathway, (+/-) in Lead V1 indicating a probable septal pathway, and (-) in lead V1 indicating a right sided pathway.[5].
Catheters are positioned in the high right atrium (HRA), coronary sinus (CS), His, and right ventricle (RV), in addition to an ablation catheter for mapping.
Evaluation of the His potential at baseline and HV interval during atrial (A) pacing of a patient with pre-excitation results in a shorter or even negative HV interval. This is a result of ventricular depolarisation through the pathway prior to His depolarisation. Ventricular (V) pacing will show the V to A activation sequence and in the case of a lateral pathway, the CS will show earliest A activation at the distal CS, indicating eccentric activation (lateral to medial), eliminating most other possible arrhythmias. While this may be enough in lateral pathways, it does not apply for paraseptal pathways. These septal APs will result in concentric activation (medial to lateral) and will require further manoeuvres to distinguish AVRT from other arrhythmias.
During tachycardia overdrive, V pacing and stopping should provoke a V-A-V response ruling out atrial tachycardia (AT). Additionally, immediate V to A acceleration and post-pacing interval (PPI) minus the tachycardia cycle length (TCL) of <115 ms confirms an orthodromic AVRT using an accessory pathway. The PPI represents the time from the last paced V until a complete revolution around the circuit comes back to that initial pacing point. Corrected for the TCL, a time <115 ms has been shown to be inconsistent, namely too fast, for normal physiologic conduction of the AV node and Purkinjes fibres, and therefore rules out AV node re-entrant tachycardia (AVNRT). This leaves AVRT via a pathway as the most probable explanation of the tachycardia. Additionally, Para-Hisian entrainment manoeuvres can also be used to distinguish AVRT from AVNRT.
Once AVRT via an AP is confirmed, electroanatomic mappings of the AV annulus during A pacing, with attention to the earliest ventricular (V) signal and vice versa (mapping the AV annulus during V pacing with attention to the earliest A) are performed. Differential atrial and ventricular pacing is crucial to determine the course of the pathway (namely oblique ones) [3]. As noted over the last decade, it is crucial to anticipate that most pathways run an oblique course across the AV annulus and that there may be more than one simultaneous pathway [4]. Awareness of these details is paramount to efficient and successfully ablated APs.
Differential pacing in line with the propagation wave would identify the shortest AV or VA interval, hence highlighting the territory of the pathway; however, it would mask the pathway potential [3,4].
Pacing from the opposite side of the propagating wavefront results in a longer VA interval but allows visualisation of the local accessory pathway potential of oblique pathways. Alternately, fusion of the A and V and absence of accessory pathway potential may indicate a vertical pathway [3].
As an alternative to the conventional point-by-point mapping, open window mapping can also assist in localising and treatment of the pathway [6], by acquiring the sharpest local signals of the electroanatomic map during AV re-entrant tachycardia.
A review of the unipolar recordings of the ablation catheter confirms which of the electrodes is closest to the pathway manifesting with a qS pattern and helps make fine adjustments.
Ideally, ablation therapy is delivered during atrial or ventricular pacing and not during AVRT to allow a more stable and steadier catheter position. This avoids excessive movement which is unavoidable in tachycardia and often results in mechanical suppression of the pathway and/or suboptimal lesions, ultimately leading to recurrence of conduction and requiring further ablation [3].
Targeting the pathway potential with the application of a short duration 30 - 40 Watts radiofrequency (RF) lesion should be adequate to permanently eliminate the pathway within the initial seconds; nevertheless, a 60 second lesion should be completed [3].
Review of the surface QRS morphology at this point in an anterograde pathway should show resolution of the delta wave. A 6 or 12 mg Adenosine push during A or V pacing would suppress the AV node and result in momentary heart block if the pathway was definitively eliminated. Further programmed A or V stimulation during a 30-minute waiting period would confirm lack of inducibility and the permanent suppression of accessory pathway conduction.
Accepted indications and contraindications
Ablation therapy is indicated in the chronic management of symptomatic or recurrent AVRT (Class I) [1].
Pathways with higher risk features for sudden death such as shortest anterograde effective refractory period (ERP) ≤250 ms or shortest pre-excited RR interval (SPERRI) during atrial fibrillation of ≤250 ms are also accepted indications for ablation [1].
Occasionally, pathways may be determined to be low-risk bystanders to other arrhythmias and, as such, may not require ablation.
Patient with asymptomatic pre-excitation who happen to be competitive athletes or in high-risk occupations are advised to undergo EPS for risk stratification and potential ablation (Class I) [7].
Pathways superimposed or in locations with a high likelihood of damage to the Bundle of His conduction system should be avoided or at least require a prolonged conversation with the patient about the risks of heart block, requiring permanent pacing.
Pro and con aspects
Caution is advised in patients with septal pathways as their ablation poses a higher risk of AV block (0.17-2.7%); as an alternative to RF, cryoablation might be a useful alternative to radiofrequency, due to a lower risk of permanent damage. Also, ablation at the most distal site from an identifiable bundle of His [1].
Occasionally pathways are most accessible via the CS and require coronary angiography to confirm the distance of major coronary arteries. It is recommended to identify at least a 5 mm gap to avoid heating injury. Additionally, irrigated catheters are crucial in these cases with maximum of 15 to 25 watts, again to avoid unwarranted injury [3].
The most recent recommendations from the ESC and HRS/ACC guidelines list beta blockers and calcium channel blockers as Class IIa and I, respectively (in absence of pre-excitation). They have far less success as compared to ablation, but studies showing prevention of AVRT recurrence varying between 40-70% and are generally well-tolerated [8]. Class 1c anti-arrhythmics, such as procainamide and flecainide, in patients without structural heart disease yielded recurrences in as many as 50% of patients and required up-titration [9,10].
Catheter ablation studies since the early 1990s have shown far superior success rates compared to oral therapy: as high as 99% with <2% risk of complications [11]. Further evidence supports improved outcomes with these types of ablations with incremental operator experience [12].
ESC guidelines versus other guidelines
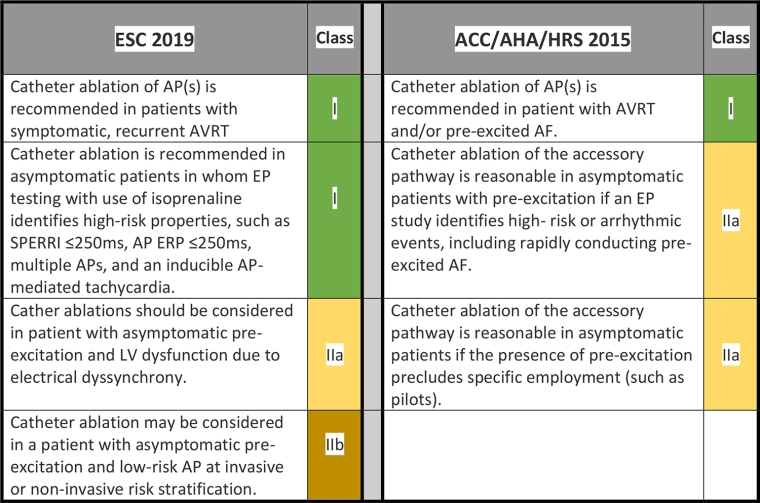
Overall, the ESC and ACC/AHA/HRS describe similar indications for EP study with minor differences in the levels of recommendation, likely reflecting the years the documents were drafted respectively. The following is a summary of the guidelines concerning ablation as a form of therapy in patients with accessory pathways [1,7].
Table 1. 2019 ESC Guidelines [13] versus 2015 ACC/AHA/HRS Guidelines [14] on AP ablation.
AF: atrial fibrillation AP: accessory pathway; AVRT: re-entrant tachycardia; EP: electrophysiology; ERP: effective refractory period; LV: left ventricular; SPERRI: shortest pre-excited RR interval during atrial fibrillation
Take-home messages
- Most pathways can conduct both anterograde and retrograde.
- Pathways are localised based on ECG review and intracardiac electrogram evaluation.
- EPS is useful in evaluating the conduction of pathways and determining their risk features to assist in the decision to ablate.
- Mapping allows specific identification of pathway potential and pinpoints a targeted approach for ablation.
- Catheter ablation is a Class I recommendation in symptomatic AVRT, and certain high-risk asymptomatic populations.
- Minimal ablation is required for permanent elimination of pathways.
- Ablation of pathways proximal to the Bundle of His pose a risk of heart block and requires careful clinical assessment, patient discussion and understanding of the risks.
- Catheter ablation in AVRT has a >95% success rate and a <2 % complication rate.
- Medical therapy has some success but is far inferior to ablation therapy.