Epidemiology
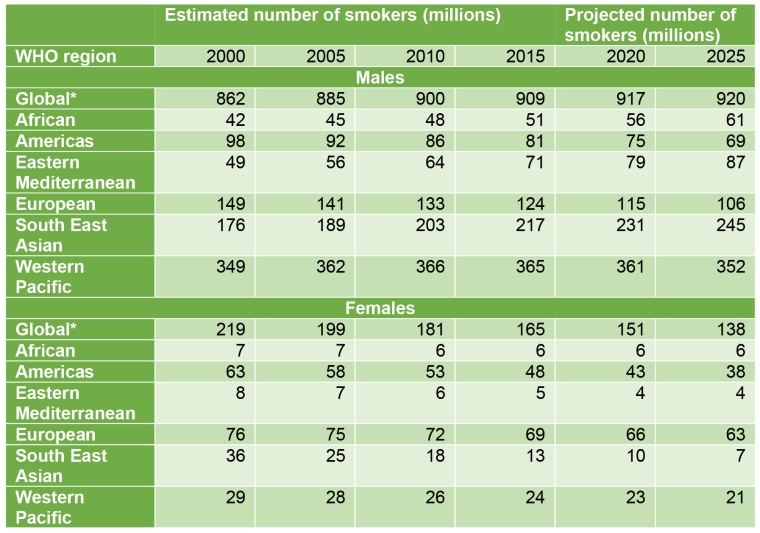
Globally, 942 million men and 175 million women aged 15 or older are current smokers. Nearly three quarters of male daily smokers live in countries with a medium or high human development index (HDI), whereas half of female daily smokers live in countries with a very high HDI [1].
Among the World Health Organization (WHO) regions, Europe has the highest prevalence of tobacco smoking among adults (28%) and some of the highest prevalence of tobacco use by adolescents. Moreover, Europe has one of the highest proportions of deaths attributable to tobacco use. The WHO has estimated that 16% of all deaths in adults over 30 in Europe are related to tobacco consumption. Even though tobacco use has been a predominantly male phenomenon for decades, the prevalence of cigarette smoking among women has increased worldwide in recent years and the gender gap has been substantially reduced in countries such as Greece, Denmark, Ireland, the Netherlands, Norway, Sweden and the United Kingdom. Although tobacco use among women is now decreasing overall, it is dropping at a much slower rate than in men and is still increasing in some areas of the European region.
Based on the WHO global report on trends in prevalence of tobacco use 2000-2025, in 2018 the prevalence for European women was 19%, the highest in the world, whereas the global rate was 9%. Even if women’s prevalence has declined in Europe from 23% in 2000, it is expected to sit at around 18% in 2025 [2], which is still a concerning picture. Tobacco consumption in women is very influenced by the socioeconomic status, with a higher prevalence in high-income countries.
According to the World Bank Report, the prevalence of smoking among women in countries with high income is 16.1%, compared to 2% in low-income countries. The lower prevalence of tobacco use in women in regions with a low HDI has offered a window of opportunity to the tobacco industry to tailor its marketing efforts in this direction. Of the 8.71 million annual tobacco deaths, 2.15 million are women (2019) [3], 71% of whom live in low- and middle-income countries [4].
There is a 30-year gap between peak tobacco use and peak tobacco-related mortality. As women’s uptake of tobacco has occurred later in the tobacco epidemic, the surge in tobacco-related female deaths has also occurred later than for male deaths. This perspective offers a relevant public health concern in many societies where the prevalence of female smoking is still rising [5].
Health effects of smoking in women
Tobacco use promotes exposure to a lethal mixture of more than 7,000 toxic chemicals, including at least 70 known carcinogens which can cause damage to nearly every organ system in the human body [1]. The risk of death and disease rises with the number of cigarettes smoked, but even low consumption can also cause significant damage.
Beyond increasing the risk of the same diseases as in men, smoking in women carries the risk of several gender-specific conditions such as cervical cancer, osteoporosis, fertility impairment, and premature menopause. The risk of preterm birth is increased in women who smoke before and during pregnancy, as is the risk of abnormal foetal growth, low birth weight, miscarriage, and foetal death [6]. Despite these well-known risks, smoking during pregnancy remains the leading cause of poor pregnancy outcome and prenatal death.
Globally, more than 50% of women who smoke daily continue doing so during pregnancy [7]. Persistent smoking behaviour in pregnant women is strongly associated with social health factors such as a young age, a lower socioeconomic status or a lower level of education [8].
An important body of evidence shows that smoking does not affect men and women equally when considering cardiovascular and lung diseases. The relative risk of lung cancer is significantly higher in women who smoke compared to male smokers [9]. Lung cancer is the leading cause of cancer death among men and, in many countries, it has also become the leading cause of cancer death in women, exceeding breast cancer [1].
Women who smoke also have a markedly increased risk of cancers of the mouth, pharynx, oesophagus, larynx, bladder, pancreas, and kidney. The risk of cervical cancer has also been shown to be higher in female smokers than in female non-smokers [10].
The worldwide prevalence of chronic obstructive pulmonary disease (COPD) has increased steadily in recent decades, with a greater rise in women than in men. A growing body of evidence suggests that female smokers are more likely to develop COPD than male smokers [11]. Women seem to be more vulnerable to lung function impairment and develop COPD at a younger age for a given amount of tobacco consumption [12].
Smoking is a more potent risk factor for cardiovascular disease in women. In a meta-analysis of 2.4 million subjects, cigarette smoking was found to confer a 25% increase in the risk for coronary artery disease in women compared with men [13]. Furthermore, oral contraceptive users who are current smokers have a tenfold increased risk of myocardial infarction and a threefold increased risk of stroke [14].
Other associated factors such as a sedentary lifestyle and obesity can increase the cardiovascular impact of smoking in women.
Electronic cigarettes and novel tobacco products
The rapidly evolving marketplace of vaping products has represented a challenge to the regulation capacity of different countries. The popularity of these products has been supported by strong marketing, targeted particularly to women and adolescents [15]. Flavourings that are currently banned in conventional cigarettes may be used to attract new young consumers who are prone to experimentation and risk-taking behaviour, facilitating the progression to regular use of e-cigarettes or other tobacco-related products.
While there is still a burning debate concerning the role of electronic nicotine delivery systems (ENDS) as a harm reduction strategy in adult smokers, from the public health perspective the main concern is that ENDS could be a gateway to nicotine addiction, particularly in adolescents [16,17]. E-cigarette use has recently been associated with the outbreak of e-cigarette or vaping product use-associated lung injury (EVALI) in the USA in 2019, with a particular impact on young e-cigarette users [18]. In any case, the long-term effects of e-cigarettes have not been established, while these products lack strict regulation in many countries and are often promoted as “socially acceptable” and “reduced-risk alternatives”.
Different “heat-not-burn” tobacco products have rapidly gained a market in recent years as the result of an aggressive promotion campaign from the tobacco industry, targeting particularly women and young consumers, and trying to evade conventional tobacco regulation. The devices heat processed tobacco in a controlled fashion instead of combusting it. As they contain tobacco, these products are hazardous and likely to be more harmful than e-cigarettes, and they lack reliable evidence of any harm reduction effect. Nevertheless, they are marketed as “less harmful”, a strategy fraught with dangers of youth uptake, unproven long-term impact, and the potential to mislead their potential users [19].
Second-hand smoke
Second-hand smoke (SHS) is the combination of smoke from the burning end of a cigarette and the smoke breathed out by smokers. SHS contains more than 7,000 chemicals, of which hundreds are toxic and about 70 can cause cancer [10]. Exposure to SHS is associated with a large number of adverse health effects and causes substantial mortality and morbidity globally.
SHS causes the death of 600,000 women every year, and 64% of annual SHS-related deaths are of women [3]. SHS can cause coronary disease, stroke, lung cancer, COPD, and reproductive effects in women such as low birth weight. SHS has also been related to sudden infant death syndrome, asthma, impaired lung function, lower respiratory illness and middle ear disease in children [10].
Lower socioeconomic groups and non-smoking women show higher exposure to SHS. It is estimated that SHS causes more deaths in women than in men globally (573,000 vs 311,000 in 2016). Homes are the main place of exposure to SHS for women and children in many populations. Therefore, regulation and preventive campaigns focusing on exposure inside the home are of paramount importance in order to reduce the burden of SHS [1].
Barriers to smoking cessation in women
One of the reasons for smoking in women has been the aggressive explicit or implicit promotion of tobacco products focused particularly on women over the past century. Despite the regulatory efforts in high-income countries, advertising continues in low-income countries, where female smoking rates are still low.
Stereotypical attractive qualities such as freedom, sophistication, self-determination, glamour, or slimness have been widely used to attract women or adolescent girls. Trying to elude the tobacco marketing and promotion regulation in developed countries, tobacco companies still use other platforms available such as social media, cinema or women influencers. Exposure to tobacco in films is strongly related to tobacco uptake among young people, and it is a subtle and difficult to combat means of promotion of tobacco use [20]. Female characters who smoke are often shown as attractive, fashionable, provocative, cool and of high social status. This form of promotion is particularly concerning as it contributes to normalise smoking in different situations of daily life. Packaging and cigarette design can also be considered as marketing tools that have been widely used by the tobacco industry to target particular profiles of consumers. Super-slim and lipstick-style cigarette packs created a misleading perception of harm reduction in female smokers [21]. The adoption of plain packaging offers a relevant opportunity to remove this promotional strategy.
The strong addictive capacity of nicotine and the faster capacity to metabolise nicotine in women make women more prone to becoming hooked on tobacco [22]. Moreover, risk awareness is lower in women than in men and women have less success at quitting [23]. Women are likely to continue smoking due to a fear of weight gain.
The solutions
Effective tobacco control is of paramount importance in order to improve health and reduce disparities at the population level in all countries. Tobacco product taxation is an effective way to reduce tobacco use rates, and one of the most powerful measures in preventing tobacco consumption by adolescents [24].
Creating smoke-free environments is also vital in tobacco control.
Smoking bans protect non-smokers from the harmful effects of SHS and facilitate the progressive denormalisation of tobacco consumption, by reinforcing the idea of non-smoking as a societal norm.
Electronic cigarettes and novel tobacco products should not undermine tobacco control efforts, and thus require an updated and proper regulation.
Public health campaigns with a focus on preventing smoking among young people should be gender-sensitive, as the reasons for starting smoking differ between boys and girls, girls being more affected by the desire to control weight or by a positive image of smoking.
Tobacco cessation is a cost-effective healthcare intervention [10]. More quitting and less initiation of tobacco use contribute to greater individual and societal well-being. Governments and healthcare providers should make available more and accessible resources to help tobacco users stop. These interventions should be able to tackle women and adolescents from a specific perspective, taking into account the particular characteristics of nicotine addiction in these populations.
The younger someone is when he/she stops smoking, the greater the benefit in terms of health gains and mortality reduction. Pregnancy is a particular teachable moment to start a smoking cessation intervention in women and their partners. Smoking cessation in pregnant women has been associated with improvements in outcomes including better foetal growth and fewer preterm deliveries, and it can avoid subsequent risks to the child. Quitting smoking is also one of the best natural ways to boost fertility in both women and men [8,10].
Conclusions
Tobacco causes an enormous health, social, economic, and developmental burden. Consistent with lower female smoking prevalence in many countries, the tobacco-related burden in women is lower than in men globally. However, recent increases in smoking prevalence among females, particularly in developing countries, might change this pattern.
- Female smokers are more vulnerable to some smoking-related pathologies than their counterparts.
- In addition to the harm caused directly by smoking, many women die because of involuntary exposure to second-hand smoke.
- Gender-specific action is needed to raise awareness of the impact of tobacco on women´s health and to tackle smoking cessation in women.
Tobacco control needs to counteract the gender-specific messaging transmitted by the tobacco industry that still tries to promote the use of tobacco and tobacco-related products by women.