Background
Age is a relevant risk factor for cardiovascular disease and is associated with higher event rates. If drug efficacy does not decrease with age, a preventive therapy such as lipid-lowering medication could have a potentially higher benefit (absolute risk reduction) in older adults with a reasonable life expectancy, which leads to a lower number-needed-to-treat [1, 2], and therefore argues strongly for the implementation of such therapies.
While guideline recommendations on lipid-lowering therapy for secondary prevention in older patients are the same as for younger patients, evidence on primary prevention is less clear [3]. Potential cardiovascular benefits are countered by concerns about the risk of adverse effects. Also, end-of-life situations might compromise the expected benefit of lipid-lowering therapy. Moreover, older patients are a heterogeneous patient group not only in terms of age, but also in terms of comorbidity and functionality, ranging from the robust and resilient to the frail.
Primary prevention in patients at an advanced age is a topic that has recently gained increasing importance. In this article, we will discuss the various aspects relevant to the management of lipid-lowering therapy in this complex context. While most evidence so far is derived from observational studies, and subgroups of randomised controlled trials (RCT), several RCT are underway that specifically address primary prevention in older patients.
Initiation of lipid-lowering treatment for primary prevention in old age: guideline recommendations and summary of evidence
Lipid-lowering treatment in patients with vascular diseases is recommended for older and younger patients alike (Class 1 Level A, 2019 ESC/EAS Guidelines) [3, 4].
According to the 2019 ESC/EAS Guidelines for the management of dyslipidaemias, the decision concerning whether to start lipid-lowering treatment for primary prevention needs to be adapted to the individual risk profile of the patient. For patients ≤75 years of age without atherosclerotic disease, the treatment decision should be guided by the cardiovascular risk according to the SCORE chart, displaying the ten-year risk of fatal cardiovascular disease [3]. For patients aged >75 at high or very high cardiovascular risk, initiation of statin treatment may be considered individually [3]. Several other European and North American dyslipidaemia guidelines support such a patient-centred approach in older adults, though age cut-offs and strategies for cardiovascular risk assessment vary [2].
So far, data from randomised controlled trials have been limited to sub-analyses of (mostly) non-age-specific studies in the context of primary prevention. A meta-analysis of data from the JUPITER and HOPE-3 trials showed that treatment with rosuvastatin was superior to placebo for patients ≥70 years regarding a composite endpoint of non-fatal myocardial infarction, non-fatal stroke, or cardiovascular death [1]. However, the number of patients ≥80 years included was limited. In a post hoc analysis of the ALLHAT-LLT primary prevention RCT with all-cause mortality as the primary endpoint, no benefit was seen for patients ≥65 years on pravastatin 40 mg versus standard care, with more events observed in the pravastatin group [5].
Two RCT specifically targeting the benefits of lipid-lowering therapy in the context of primary prevention in older adults are currently active - A Clinical Trial of STAtin Therapy for Reducing Events in the Elderly (STAREE), and Pragmatic Evaluation of Events And Benefits of Lipid-lowering in Older Adults (PREVENTABLE), examining the effects of atorvastatin versus placebo treatment in persons aged ≥70 and ≥75 years, respectively (NCT02099123 and NCT04262206).
Observational studies have revealed conflicting results regarding the benefit of initiating lipid-lowering treatment in older adults without overt vascular disease. A recently published retrospective study of more than 300,000 US veterans (mainly white male, among them over 55,000 statin users) aged ≥75 years showed a benefit from statin therapy regarding all-cause and cardiovascular death [6]. In contrast, in a retrospective study based on Catalan healthcare data, newly starting statins for primary prevention in non-diabetic patients aged ≥75 years was not associated with a reduction in cardiovascular disease events or all-cause mortality during a median follow-up of 5.6 years [7]. For diabetic patients, starting statins for primary prevention was beneficial if they were <85 years old. Another smaller population-based cohort study drawn from French healthcare data produced a similar finding: new users of statin for primary prevention ≥75 years old only benefited from statin therapy if diabetes mellitus or other modifiable risk factors were detectable. The latter was the case for nearly 85% of patients in the primary prevention group. Unlike other studies, this study included only acute coronary syndrome as a cardiovascular outcome, and all-cause death, so that other beneficial effects might have been missed [8].
In the Cholesterol Treatment Trialists’ Collaboration meta-analysis of 28 RCT, the evidence for patients >75 years old taking statins for primary prevention was not strong (RR 0.92 per 1 mmol/L LDL reduction, CI: 0.72-1.16), as opposed to secondary prevention with a 26% proportional reduction of major vascular events per 1 mmol/L reduction in LDL cholesterol for patients >75 years old with a history of vascular disease (RR 0.74, CI: 0.60-0.91) (excluding data derived solely from heart failure and dialysis trials) [4].
The central strategy in the question of whether statins should be initiated for primary prevention should be the concept of “de-risking”. Hence, an essential question the physician needs to consider when making recommendations to individual patients is whether the expected time-to-benefit from statin therapy exceeds the expected time-to-harm or actual life expectancy.
Non-invasive cardiovascular imaging (arterial plaque burden in ultrasound, calcium scoring in computed tomography [CT]) should/may be considered as adjunct information (IIa B and IIb B [3]). Though we are not currently aware of any data specifically addressing non-invasive imaging for risk evaluation in older patients, this approach might help in the decision-making process in the future.
How should lipid-lowering therapy in older patients be performed?
LDL-cholesterol goals should generally be in line with the 2019 ESC/EAS guidelines [3].
A reduced starting dose is recommended only for rosuvastatin (Table 1). However, there might also be other situations where a low starting dose with consecutive up-titration appears a safer option for an older patient, even more so if the statin is prescribed for primary prevention. The 2019 ESC/EAS Guidelines recommend a low starting dose in renal impairment or if there is risk of drug-drug interaction (I C [3]). This is to be understood as potential drug-drug interactions which might increase systemic statin exposure, e.g., because of CYP3A4 inhibition.
Table 1. SmPC recommendations for lipid-lowering therapy in older patients.
| Lipid-lowering | Considerations in older patients |
|---|---|
| Atorvastatin | At recommended doses efficacy and tolerability in patients >70 years comparable to total population. |
| Fluvastatin | No dose adaptation recommended. |
| Lovastatin | Efficacy in patients >60 years comparable to total population; no obvious increase of adverse events. |
| Pitavastatin | No dose adaptation recommended. |
| Pravastatin | No dose adaptation unless other risk factors are present. |
| Rosuvastatin | Starting dose of 5 mg for patients >70 years. |
| Simvastatin | No dose adaptation recommended. |
| Ezetimibe | No dose adaptation recommended. |
Summary of product characteristics (SmPC) of Sortis Filmtabletten (September 2019), Fluvastatin Hexal Hartkapseln (June 2019), Lovastatin AL Tabletten (June 2015), Livazo Filmtabletten (June 2015), Pravastatin Hexal (May 2018), Crestor Filmtabletten (June 2019), Simva Basics Filmtabletten (February 2018), Ezetab Tabletten (March 2017)
Data on lipid-lowering therapy with ezetimibe in older patients is limited. However, a recent Japanese multicentre, randomised, open-label trial showed a reduction in the composite outcome of sudden cardiac death, myocardial infarction, coronary revascularisation, or stroke. There was, however, no difference for stroke alone or all-cause mortality, with more deaths occurring in the ezetimibe group [9].
What are the potential challenges of statin therapy in older patients?
Heterogeneity in functionality and frailty status
Frailty is a medical syndrome that is characterised by a decline in functionality and increased vulnerability. Older individuals with frailty show an increased risk for developing unfavourable outcomes such as dependency or death [10]. In the care of older adults, clinicians are faced with a highly heterogeneous population ranging from robust and independent persons to frail individuals who are dependent on help in their activities of daily living. Based on these considerations, specific age cut-offs for the initiation or stopping of lipid-lowering treatment seem arbitrary.
Evidence on the benefits and risks of lipid-lowering therapy for primary prevention in old age is limited not only because of sparse data from RCT in older populations in general, but also by a lack of information regarding the study participants’ functionality and frailty status.
The PREVENTABLE trial will assess the benefits of primary prevention with atorvastatin 40 mg in 20,000 community-dwelling adults aged ≥75 years. Though only older adults independent in their activities of daily living are eligible for inclusion, the participants’ motor function will be characterised with the “Short Physical Performance Battery” (SPPB) at baseline (https://clinicaltrials.gov/ct2/show/NCT04262206). This trial might provide some evidence on the benefit of primary prevention with regard to the physical function of the older patient.
Risk of adverse effects
A review of the risk of statin-associated muscle symptoms has been published in the European Heart Journal [11]; caution is advised for patients starting at age 75, women, patients with low body mass index, hypothyroidism, or pre-existing muscle symptoms, among others. In contrast, there are different opinions about the impact of renal disease [11, 12].
Older patients should be closely monitored when statins are started, but also during statin therapy. Although, based on the available evidence, statin treatment does not have a general deteriorating impact on physical function and frailty in community-dwelling older adults, adverse muscle-related effects might still be of relevance to those individuals who already have severe functional impairment [13]. The 2019 ESC/EAS Guidelines provide algorithms for monitoring statin therapy, which should be a minimum requirement in this specific patient group [3]. However, there are also data indicating that myalgia is reported less frequently by those aged >75 years than by the younger [14]. It should also be taken into account that the symptomatology of adverse effects might be less overt than in younger patients.
Polypharmacy/potential for drug interactions
Drug interactions can increase the risk of adverse effects, such as myopathy and rhabdomyolysis. Drugs potentially interacting with statins via CYP3A4 discussed in the 2019 ESC/EAS Guidelines [3] that might be of foremost relevance in older patients are macrolides (erythromycin, clarithromycin, telithromycin), the azoles (e.g., itraconazole), calcium antagonists (verapamil, diltiazem, amlodipine), cyclosporine, and amiodarone. Patients should be reminded to refrain from grapefruit juice. Simvastatin, atorvastatin, and lovastatin are substrates of CYP3A4 [15], and most statins (except fluvastatin) are also substrates of hepatic OATP1B uptake transporters whose inhibition or genetic variation can critically increase the risk for systemic adverse events (rhabdomyolysis).
Non-adherence
Non-adherence and discontinuation in the first year of statin therapy appears to be a relevant problem. In an Australian nationwide cohort study of patients aged ≥65 years who had started on a statin, non-adherence occurred in 55% and discontinuation in nearly 45% of cases. Rates were higher in diabetic patients, and in those with comorbidities related to anxiety and pain. In contrast, polypharmacy, use of platelet inhibitors/anticoagulation therapy and cardiovascular comorbidities such as hypertension and angina were associated with less non-adherence and discontinuation of therapy [16].
Non-adherence and discontinuation of therapy should be taken seriously. While the institutional framework of the healthcare system can vary from country to country, modifiable factors at the physician and patient level should always be considered. This concerns both the first drug prescription and follow-up visits to provide patients with timely prescriptions and motivate them to continue therapy in the long term. Shared decision making is encouraged.
Is it safe to de-prescribe statin therapy in older age?
Data on discontinuing existing statin therapy are conflicting. There is little guidance on discontinuing statins beyond the reason of the occurrence of adverse effects [17]. However, the risk of unintentional or negligent statin withdrawal is high when patients move to other healthcare sectors (e.g., emergency admissions) where previous therapies are often discontinued. A number of studies have shown that after acute vascular emergencies patients can be negatively affected by acute discontinuation of statins, and cardiovascular or cerebrovascular outcomes can be worse in this patient group than in those who took statins or continued to take them [18]. Although these data do not specifically refer to an older population, they should be noted and taken seriously when taking care of older patients with a previous vascular event.
With regard to primary prevention, a French nationwide population-based cohort study of statin discontinuation in 75-year-old patients with no history of cardiovascular disease revealed a one third increased risk of hospitalisation due to a cardiovascular event [19].
A clinical parallel-group trial in patients with an estimated life expectancy of less than one year showed no inferiority in 60-day death and no significant difference in cardiovascular events after statin discontinuation. Patient-reported outcomes yielded a better psychological quality of life, better wellbeing and better support, but no relevant difference in physical quality of life [20].
In summary, we find that it is not justified to de-prescribe statin purely because of higher age. However, patient preferences, and end-of-life situations should be taken into consideration.
Conclusion
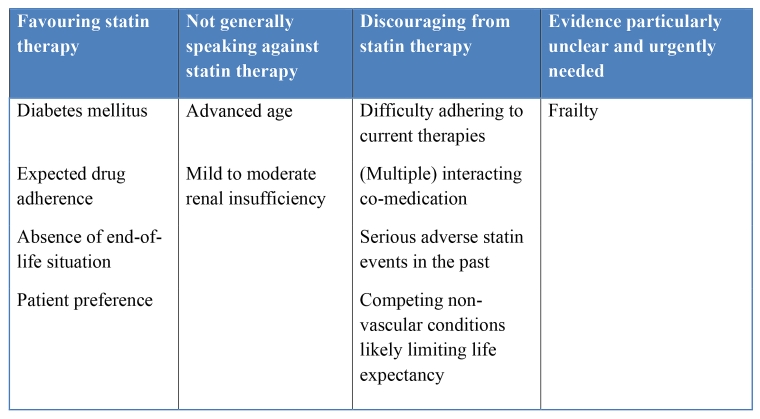
We suggest a patient-centred, individualised approach to lipid management for primary prevention in older patients. Statin therapy should not be refused on the basis of age alone. Cardiovascular risk factors (e.g., diabetes mellitus), which make statin therapy more urgent, should be considered, while (life-limiting) comorbidities may lead to a more conservative approach (Table 2). Shared decision making is encouraged.
Perspective
The results of three trials are anticipated with great interest:
- A Clinical Trial of STAtin Therapy for Reducing Events in the Elderly (STAREE): atorvastatin 40 mg compared in healthy elderly people (≥70 years)
- Statins In The Elderly (SITE): RCT on statin cessation in people ≥75 years
- Pragmatic Evaluation of Events And Benefits of Lipid-lowering in Older Adults (PREVENTABLE) (Recruiting expected to start in September 2020)
Recommended reading
Additionally, we find the following reviews helpful on the topic of primary prevention in older patients.
- Mortensen MB, Falk E. Primary Prevention With Statins in the Elderly. J Am Coll Cardiol. 2018;71:85-94.
- O'Neill D, Stone NJ, Forman DE. Primary Prevention Statins in Older Adults: Personalised Care for a Heterogeneous Population. J Am Geriatr Soc. 2020;68:467-473.
Further detail on the role of OATP in statin therapy can be found in:
- Link E, Parish S, Armitage J, Bowman L, Heath S, Matsuda F, Gut I, Lathrop M, Collins R. SLCO1B1 variants and statin-induced myopathy--a genomewide study. N Engl J Med. 2008;359:789-99.