Background
In most developed societies, as a result of reduced birth rates and improved global health care, there is a demographic shift resulting in increasingly ageing populations. Sport is recognised as a significant contributor to the accumulation of sufficient physical activity (PA) to promote and maintain physical health with additional known social and psychological benefits. This last assumption is also valid in an aging population [1].
Recognising the health implications of inactivity, the World Health Organization (WHO) in 2018 launched its Global Action Plan on Physical Activity and Health 2018-2030 [2]. Obviously, current sports policies and delivery strategies could influence sports participation in older age groups by way of “limits” that are periodically laid out by referral recommendations and/or guidelines [3]. Moreover, the broader term PA encompasses both competitive and non-competitive sports. For many individuals sports participation is the primary way to maintain a healthy mental state and to achieve the greater part of their PA over the course of a week [4].
Each day, our experience as a cardiologist and a geriatrician working respectively in a Cardiac Rehabilitation Unit and with the “elderly” in an internal medicine setting, underline the importance of PA for fighting cardiovascular risk factors (CVRF), including ageing populations and/or in subjects who have undergone CV procedures such as percutaneous coronary intervention (PCI) or surgery [5].
Moreover, in recent years we have been involved with the Biomedical Committee of the Italian Soccer Referees Association (named AIA). Frequently former and aged referees have asked about CV risk (CVR) and sports, especially in the aging population. Currently, in Italy, those above 45 years old (y/o) are not allowed to practise as referees. However, a large number of them would like to continue because many of them have no history of cardiac and/or vascular disease.
Therefore, the question proposed in the title is much debated, and not only in the “AIA”. Besides that, so many other questions need more precise answers. Is there any difference in CVR related to a specific choice of exercise and/or age? What rules should apply for each type of PA? Finally, which is the “winner” - risk or benefit? These questions are only some examples of those we might be posed by our friends and patients.
We know that all the main scientific societies periodically deliver specific recommendations and guidelines about sports participation and/or the “eligibility” of different populations - younger versus older including healthy subjects versus those with a disease history, especially CV disease (CVD). Recently, the European Society of Cardiology (ESC) has also updated the referral document regarding sports cardiology and exercise in patients with CVD [6].
While it is clear that this topic is very wide, and much more time and space is necessary than we have to fully analyse it here, we will try, in the following paragraphs to provide a brief review of the literature on the subject of “competitive sports in those aged >65”, underlining currently known pros (PRO) and cons (CONTRA).
Pro
Sport and ageing are linked much more than anyone might think.
Before analysing all the main potential effects on CVRF, it is very interesting to remember how exercise might positively influence the cognitive and psychosocial status of older people. Indeed, it is sufficiently well established that PA may contribute to health in the elderly by means of fall prevention and improving global cognitive status. Sherrington et al stated that exercise, even as a single intervention, can prevent falls in community-dwelling populations aged 65 y/o or more [7], whilst a paper by Northey et al affirms that physical exercise improves cognitive function in the over 50s, regardless of the baseline cognitive status of participants [8].
In a very recent review, Stenner et al collected a total of 1,732 studies searching for reasons why older people engage in sports [9]. Searches of the electronic databases Embase, Medline, PsycInfo, PubMed, and SPORTDiscus have revealed that aged adults practise PA mainly for maintaining health, feeling and being part of a community and taking advantage of opportunities to develop relationships. Secondarily, sport is a “method” for competing and attaining a feeling of achievement, taking advantage of opportunities for travel, and being part of a team. Finally, PA and exercise were identified as contributing to the overall experience of successful ageing.
However, older adults are a heterogeneous group and therefore require different strategies from other age groups to participate successfully in and benefit from sport [10], benefits which, most of the time, seem to be related to the CV system. In this connection, the latest ESC guidelines on sports cardiology and CVD have confirmed the importance of exercise promotion even in older people and/or in some higher CVR categories. Indeed, in the literature it is well established that regular exercise can reduce all-cause mortality and the overall burden of CVD.
Several studies have demonstrated that regular PA may bring clear benefits to CV morbidity and/or mortality rates [11]. We live in a society where many people have a sedentary lifestyle, especially in Western countries and many individuals are overweight and/or obese. Nowadays, metabolic syndrome (MS) is increasingly widespread and type 2 diabetes mellitus (T2DM) rates are also rising. Such data are alarming, but we know that exercise can contribute to better glycaemic control, avoiding, for example, the development of overt diabetes in subjects with MS only. PA also improves blood pressure (BP) values and lipid profile, and this can help weight loss.
Contra
We have already discussed the benefits of exercise even in individuals at higher CVR. Nevertheless, the latest recommendations of the ESC highlight how important it is to define the CV profile of similar populations by means of pre-participation screenings. Indeed, one of the most pivotal aims of recent guidelines is to minimise the risk of major CV adverse events (MACE) including sudden cardiac arrest (SCA) and death (SCD) during the practice of PA. All major experts have understood over the years that SCD is the main enemy for all athletes (competitive or not) and estimated incidence rates vary greatly (from almost 1 in a million to 1 in 5,000 per year) due to heterogeneous study methodology and population comparisons [12].
Nowadays, it is well known that SCA and SCD are very often related to myocardial ischaemia which causes acute coronary syndromes (ACS) and/or myocardial infarction (MI). Exercise-induced ACS rather than MI most likely affect older people including athletes, the majority of whom have no symptoms and/or history of overt coronary artery disease (CAD). Therefore, discovering subclinical CVD (especially CAD) in subjects who are preparing to participate in sports is fundamental [13]. In particular, data in the literature show that, in athletes >35 y/o, about 80% of SCA is due to unknown CAD; vigorous exercise might be catastrophic in this population, especially in those individuals with little or no background in systematic training.
However, in the literature the relationship between CAD and sport is much debated. Some studies in middle-aged and older (master) athletes with atherosclerotic risk factors for CAD reported higher coronary artery calcium (CAC) scores compared with sedentary individuals [14]. Nevertheless, very few studies have assessed the prevalence of CAD in master athletes with a low atherosclerotic risk profile.
Hence, in 2017, Merghani et al studied 152 master athletes and found that the majority of lifelong master endurance athletes with a low atherosclerotic risk profile have normal CAC scores. However, the study also revealed that plaques in athletes were predominantly calcific, indicating potentially different pathophysiological mechanisms for plaque formation in athletic versus sedentary men.
Therefore, on the basis of this paper, coronary plaques seem to be more abundant in athletes, whereas their stable nature could mitigate the risk of plaque rupture and acute events [15]. This study confirms that further assessments will be necessary in order to address the topic better.
Other silent enemies for the coronary systems of athletes may be congenital heart defects such as the anomalous origin of coronary arteries (AOCA) and myocardial bridges (MB). Nevertheless, AOCA has a very low prevalence (about 0.44%) in adolescents and very rarely causes SCD in the population over 40 [16]. Instead, the prevalence of MB is higher; however, in adult/senior individuals, it has been shown that the arterial compression in MB may be directly related to the atherosclerotic burden, proximal to the MB, and so the main objective is discovering unknown/silent CAD, as in the MB-free population [17].
Discussion
As we have argued thus far, current knowledge tells us that regular exercise may be useful for lowering CVRF even in those aged >65. Nevertheless, CVR rises with age; therefore, pre-competition screening is very important in older populations and in general in any higher CVR population [18,19].
Therefore, it is clear that, if exercise is good, avoiding MACE, SCA and SCD during sport is better. In order to meet such an objective, the ESC Sports Cardiology Task Force periodically delivers useful recommendations for controlling potential hidden dangers in PA. First of all, rules for sports eligibility are different between competitive (or alternatively agonistic) athletes and non-competitive athletes. Nevertheless, very frequently leisure-time PA and/or participation in organised sports requires a high or vigorous CV performance and so it is very important to clearly differentiate between “real” competitive and non-competitive subjects.
It is not simple to define a clear and/or unique diagnostic work-up for subjects aged >65 who want to practise competitive sports. Moreover, currently there is a relative lack of evidence in the literature about the subject.
Around the terms PA and exercise we have so many different scenarios (from leisure and/or recreational activities to real competitive sports). In the latest 2020 guidelines on Sports and CVD, the ESC Sports Cardiology team has preliminarily tried to classify exercise on the basis of:
- Frequency: sessions per week, bouts of exercise.
- Intensity: rate of energy expenditure expressed as percentage (%) of peak oxygen consumption (VO2 peak) and/or maximum heart rate (HR); HR reserve (HRR), etc.
- Time: duration of single and/or cumulative per week(s)/month(s) training sessions.
- Type: endurance, strength or resistance training, speed and speed endurance, flexibility, etc.
- Mode: metabolic (aerobic vs anaerobic), muscular (isometric, isotonic, dynamic, static, etc.), continuous vs interval, etc.
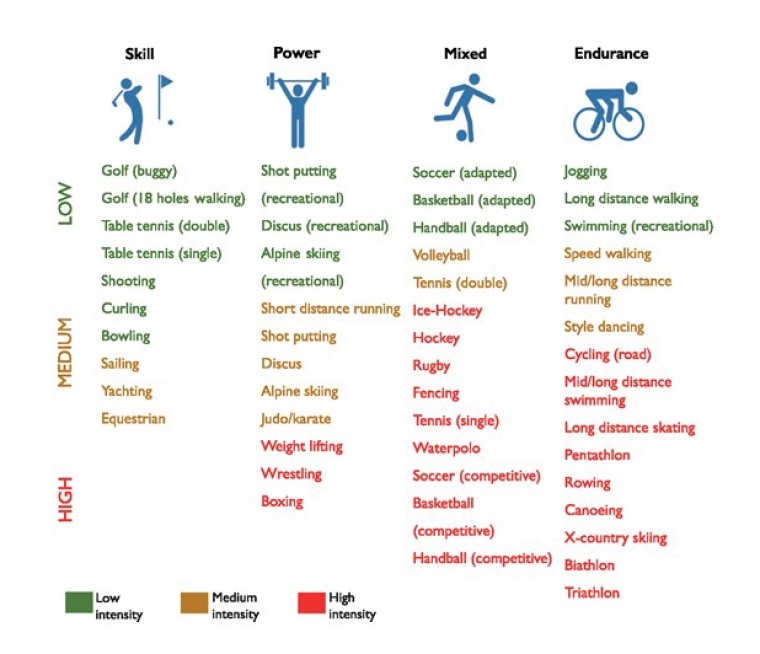
Therefore, we have 4 main categories of sporting discipline referring to the predominant component (skill, power, mixed, endurance). Within each of the above categories we can have a further subdivision on the basis of 3 different intensity levels (low, medium, high), as described in Figure 1.
From [6] Pelliccia A, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease: The Task Force on sports cardiology and exercise in patients with cardiovascular disease of the European Society of Cardiology (ESC). Eur Heart J. 2021;42:17-96 by permission of Oxford University Press on behalf of the European Society of Cardiology.
Sports Cardiology and exercise in patients with cardiovascular disease Guidelines
A similar scheme can guide physicians when they have to promote and/or advise and/or choose any type of exercise for their patients. Likewise, it can be considered an undoubtedly useful tool of choice even in the elderly sporting population.
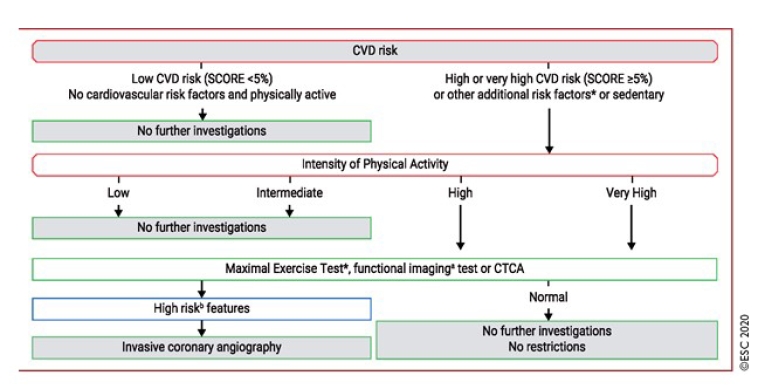
Adding to this classification, the ESC 2020 guidelines on Sports and CVD have proposed a relatively simplified algorithm for CV pre-competition assessment in asymptomatic individuals aged >35 (Figure 2). This tool, starting with well-known ESC Systematic Coronary Risk Evaluation (SCORE) charts, divides the population into low and high CVD risk, respectively, on the basis of the number of CVRF or sedentary lifestyle. If CVD risk is absent in a subject, no further investigations are compulsory.
On the other hand, in a high CVD risk population, we have to add PA intensity evaluation and, if exercise is high and/or very high intense, screening must require an ECG in addition to medical history, physical exam and SCORE. When the ECG is abnormal, an exercise maximal stress examination, and functional and/or imaging tests (especially cardiac computed tomography angiography [CCTA]) rather than invasive diagnostics such as coronary angiography are pivotal to exclude unknown myocardial ischaemia.
From [6] (Pelliccia A, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease: The Task Force on sports cardiology and exercise in patients with cardiovascular disease of the European Society of Cardiology (ESC). Eur Heart J. 2021;42:17-96) by permission of Oxford University Press on behalf of the European Society of Cardiology.
Sports Cardiology and exercise in patients with cardiovascular disease Guidelines
Consider functional test or CCTA if exercise stress test is equivocal or the ECG is uninterpretable. a See text for examples of functional imaging. b Single-photon emission computed tomography; area of ischaemia ≥10% of the left ventricular myocardium; stress echocardiography; ≥3 of 16 segments with stress-induced hypokinesia or akinesia; stress cardiovascular magnetic resonance ≥2 of 16 segments with stress perfusion defects or ≥3 dobutamine-induced dysfunctional segments; coronary computed tomography angiography (CCTA): three-vessel disease with proximal stenoses; left main disease; proximal left anterior descending disease. CVD: cardiovascular disease; ECG: electrocardiogram; SCORE: Systematic Coronary Risk Evaluation
Differently, in older athletes with symptoms, pre-participation CV exams should include an exercise ECG test such as could be considered in those subjects deemed at higher CVR according to the ESC SCORE. The usefulness of stress ECG testing can also cover diagnosis of exercise-induced arrhythmias, evaluation of BP trends during effort and quantification of preclinical symptoms such as atypical light tightness and/or initial dyspnoea.
Finally, in the latest 2020 document, the ESC confirms (as previously established in the 2017 Position Paper on Pre-participation CV screening) that elderly “athletes”, especially if naïve to moderate to vigorous PA, should be investigated by means of exercise testing or cardiopulmonary exercise testing (CPET) in order to assess CVR and measure potential performance [20].
Conclusions
Regular exercise can generate physical and psychological health. The terminology PA includes several types of possible exercise. Therefore, when a subject aged >65 asks us about practice for competitive sports, we should consider the specific type of activity that he/she would like to perform.
First of all, we should assess whether that exercise will be competitive or not. After evaluating the intensity and type of exercise chosen, physicians should advise such “athletes” and/or patients about the importance of pre-competition screening and subsequently initiate them to the most suitable diagnostic work-up, referring to the most recent recommendations.
Obviously, targeting case-by-case CVD risk more accurately can be quite difficult, so it might be necessary both to follow ESC recommendations and refer to expert sports cardiology centres if there are major doubts in order to prevent MACE and avoid SCA rather than to incur SCD.