Introduction
Dyslipidaemia is recognised as one of the most important risk factors for atherosclerotic cardiovascular disease (ASCVD). High levels of low‐density lipoprotein (LDL), and low levels of high‐density lipoprotein (HDL), are associated with myocardial infarction and stroke. In line with this information, LDL is considered the “bad” cholesterol, and lower levels are better, while HDL is considered the “good” cholesterol, and higher levels are better. However, the protective role of HDL cholesterol (HDL-C) has been seriously challenged by the evidence from recent genetic, epidemiologic and clinical trials.
Lower LDL is better
There is now overwhelming evidence from different types of clinical and genetic studies that higher LDL cholesterol (LDL-C) is a potent cause of ASCVD [1].
A recent meta-analysis, evaluating the safety and effectiveness of lowering LDL-C, has revealed that there is a consistent relative risk reduction in major cardiovascular events per change in LDL in patient populations starting as low as a median of 63 mg/dL (1.6 mmol/L) [2]. In addition, findings from a pre-specified, secondary analysis of the FOURIER trial found a monotonic relationship between achieved LDL-C and major cardiovascular outcomes down to LDL-C concentrations of less than 7 mg/dL (0.2 mmol/L) [3]. It seems that there is no lower threshold for LDL below which no further decline in ASCVD occurs. Of importance, such low levels have not been associated with increased adverse events.
Evidence from genetic trials also suggests that disorders of low LDL-C are associated with protection from coronary disease [4]. Moreover, Mendelian randomisation studies have shown that prolonged exposure to lower LDL-C beginning early in life is associated with a significant reduction in the risk of coronary heart disease in a log-linear fashion, and that this reduction is substantially greater than the current practice of lowering LDL-C beginning later in life [4].
Is higher HDL better?
Many observational studies have demonstrated that low levels of HDL-C are associated with an increased risk of coronary heart disease [5-7]. The Framingham Study was the first and most important epidemiologic trial showing a strong, graded, independent, inverse relationship between HDL-C and both cardiovascular disease and total mortality [5]. HDL’s cardiovascular protective effect has conventionally been attributed to its important role in the transportation of excess cholesterol from the peripheral tissues to the liver, the process also known as reverse cholesterol transport [8]. Besides, HDL seems to have anti-inflammatory [9], anti-oxidant [10], and antithrombotic properties [11] which may contribute to its atheroprotective effects.
On the other hand, recent data challenge whether HDL-C really protects against ASCVD. Mendelian randomisation studies have consistently shown that increased HDL-C levels caused by common variants in HDL-related genes are not necessarily associated with lower incidence of cardiovascular events [12,13]. Indeed, patients with certain mutations in CETP, ABCA1, LIPC, and SCARB1 were found to have paradoxically increased risk of coronary heart disease despite having very high concentrations of HDL-C [14,15]. This is in contrast to the Mendelian randomisation studies suggesting a strong association between LDL-C and increases in ASCVD [4].
Large-scale prospective cohort studies also contradict the previous finding of a linear inverse relationship between HDL and cardiovascular disease [7,16-18]. Although it is a common finding that low levels of HDL predict increased cardiovascular risk, data from several cohorts have revealed a plateau in the inverse association above certain HDL levels. There is even a suggestion of increased cardiovascular outcomes in those with extremely high HDLs.
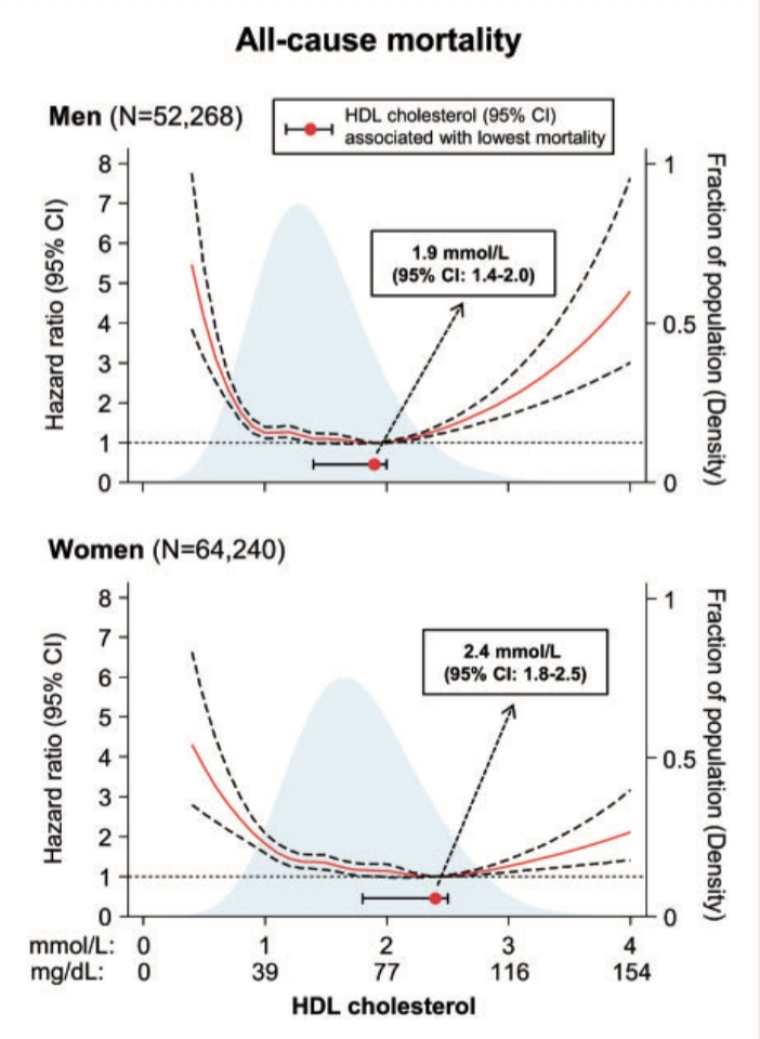
A meta-analysis of 68 long-term prospective cohort studies including 302,430 people without initial vascular disease has revealed that there is no further decrease in coronary heart disease events with HDL values higher than ~60 mg/dL (1.5 mmol/L) [7]. Likewise, in a pooled analysis from six community-based cohorts, Wilkins et al observed evidence of a plateau effect for coronary risk at HDL-C values >90 mg/dL in men and 75 mg/dL in women [16]. Recently, Madsen et al [17] examined the association of significantly elevated serum HDL-C concentrations with outcomes in two large population-based cohorts from Denmark (52,268 men and 64,240 women). For cardiovascular disease endpoints, they found a plateau around an HDL value of 58 mg/dL (1.5 mmol/L) and 77 mg/dL (2.0 mmol/L) for men and women, respectively, with no further decrease in risk with concentrations of HDL-C higher than that. Of note, the association between HDL-C concentrations and all-cause mortality was U-shaped, with both extremely high (>97 mg/dl for men, >116 mg/dl for women) and low concentrations being associated with increased risk [17] (Figure 1). A similar conclusion has been reached by Bowe et al [18], who evaluated the relationship between HDL-C and risk of death in a study involving 1.7 million United States veterans followed for over nine years. They found that HDL-C and risk of mortality exhibited a U-shaped association where risk of death is increased at low and high HDL-C levels.
The aforementioned data suggest that the old and the new observational studies yield different results regarding the cardiovascular effects of high HDL-C. At this point, it is important to highlight that the sample size of individuals with very high HDL-C (i.e., >80 mg/dL) was very small in most of the older studies, which limits the ability to draw conclusions about the risks for cardiovascular disease and total mortality associated with higher levels of HDL-C [16]. Furthermore, as mentioned by Madsen et al [17], in many of these studies individuals were categorised into larger groups, such as quintiles, and the focus was on low concentrations of HDL-C, thereby failing to elucidate associations at higher concentrations.
A similar pattern of results against the protective effects of higher HDL was obtained in randomised intervention trials carried out with niacin, fibrates, and cholesteryl ester transfer protein inhibitors. Despite being efficient at increasing HDL values, none of them was able to reduce all-cause mortality or cardiovascular events [19].
Considered together, current data establish that higher HDL-C is not necessarily protective against cardiovascular disease and may even be harmful in extremely high values. Indeed, current European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) dyslipidaemia guidelines emphasise that the risk of ASCVD appears to increase when HDL-C is above 90 mg/dL (2.3 mmol/L) [20]. On the other hand, it is not clear why very high levels of HDL-C could have negative effects while lower levels are predictive for increased cardiovascular risk. It is conceivable that plasma HDL-C concentration may not be a reliable indicator of the vascular protective function of HDL, which is very complex. Extreme elevations in HDL may represent dysfunctional HDL in some individuals, which may promote rather than protect against cardiovascular disease. Another possible explanation is that genetic mutations leading to very high HDL may also confer adverse vascular risk by unknown mechanisms.
Although the bulk of new data suggests that higher HDL-C levels are not associated with better outcomes, it should be noted that the neutral or negative effects of very high HDL have yet to be proven.
HDL cholesterol as a measure of 10-year cardiovascular risk
Current guidelines recommend the use of total cardiovascular risk assessment tools as an important step in decision making for primary prevention of cardiovascular disease. HDL-C is one of the risk measures used in commonly utilised risk tools such as the Framingham Risk Score (www.mdcalc.com/framingham-risk-score-hard-coronary-heart-disease) and American College of Cardiology/American Heart Association (ACC/AHA) pooled cohort ASCVD risk calculator (tools.acc.org/ASCVD-Risk-Estimator-Plus). The European Society of Cardiology also recommends measuring HDL-C to refine risk estimation further. We routinely use HeartScore, the electronic and interactive version of the European SCORE risk charts (www.heartscore.org).
In order to evaluate the impact of different HDL levels on cardiovascular risk estimation better, let us calculate the 10-year risk of a 53-year-old healthy man who denies having coronary artery disease risk factors, such as diabetes, cigarette smoking, hypertension, hypercholesterolaemia or family history of heart disease. Let us assume his blood pressure is 130/75 mmHg and his lipid profile is as follows:
- total cholesterol 212 mg/dL
- LDL cholesterol 115 mg/dL
- triglyceride 190 mg/dL
The estimated cardiovascular risk of this patient, with regard to different HDL-C levels, is given in Table 1. It is noteworthy that the risk of cardiovascular death decreases constantly in parallel with the increase in HDL values, without any threshold level. For example, the estimated cardiovascular mortality risk at an HDL-C level of 117 mg/dL (>116 mg/dL) corresponds to half the predicted risk at an HDL-C level of 88 mg/dL (1% vs 2%). Likewise, the risk at 88 mg/dL corresponds to half the predicted risk at 58 mg/dL (2% vs 4%). The results are more or less the same when the ACC/AHA or Framingham risk tools are applied instead of HeartScore. Apparently, existing risk assessment tools have not yet been adapted to take into account the current evidence that very high HDL-C fails to protect against ASCVD. Indeed, recent European guidelines recommend not using HDL as a risk measure when HDL-C values are above 90 mg/L (2.3 mmol/lL) [20].
Table 1. Estimated 10-year cardiovascular mortality risk of a patient by different HDL-C levels according to the HeartScore tool (www.heartscore.org).
| Gender | Age, years | SBP, mmHg | Smoking | Total cholesterol, mg/dL | HDL cholesterol, mg/dL | Estimated 10-year cardiovascular mortality risk |
|---|---|---|---|---|---|---|
| Male | 53 | 130 | No | 212 | 27 | 7% |
| 42 | 5% | |||||
| 58 | 4% | |||||
| 73 | 3% | |||||
| 88 | 2% | |||||
| >116 | 1% |
Conclusions
There is a discrepancy between recent data and the currently accepted knowledge regarding the role of higher HDL cholesterol values on cardiovascular outcomes. However, the positive, neutral or negative influence of very high HDL has not yet been fully elucidated and remains a matter of debate. Until this topic has been clarified, we should keep in mind that HDL cholesterol may not be as protective as we believe. The current risk estimation tools may underestimate the cardiovascular risk of individuals with very high HDL values which may potentially lead to underuse of cardioprotective medicines such as statins.