Introduction
Regular physical activity (PA) confers significant long-term cardiovascular benefit. Its benefit is unparalleled, with a 35% reduction in cardiovascular mortality and a 33% reduction in all-cause mortality when performed in relatively modest doses [1]. Current recommendations advise at least 150 minutes of moderate intensity physical activity on a weekly basis. Intense exercise may paradoxically provoke life-threatening arrhythmias in individuals harbouring cardiovascular disease. The drive to achieve sporting excellence exponentially increases this risk in athletic individuals. Understandably, sudden cardiac death (SCD) remains the leading cause of sports and exercise-related mortality in athletes.
Cardiac arrest is often the first presentation for most affected athletes. Only 20% report symptoms prior to an adverse cardiac event. Preventing SCD in athletes is now a priority for most sporting bodies. Pre-participation cardiovascular screening is aimed at identifying high-risk individuals at risk of SCD. The European Society of Cardiology (ESC) recommends serial cardiac screening in all competitive athletes [2]. The advised screening protocol includes a history, physical examination, and a resting 12-lead electrocardiogram (ECG). The absence of symptoms in a substantial proportion of individuals with congenital heart disease (CHD) often discourages patients from undergoing surveillance. Admittedly, most would not require a conservative management strategy. Clinical evaluation for patients keen to adopt a physically active lifestyle is advisable, as the underlying physiology may not keep up with the demand. With better clinical care of children and adolescents with congenital heart disease (CHD), the number of patients with mild or repaired CHD who would like to engage in intense physical activity is on the rise. There are now more adults than children affected by these conditions, with an estimated prevalence of one in 150 young adults [3]. This number is expected to increase further, which is why awareness about the thorough evaluation which should be carried out in athletes with CHD is essential.
Physical activity in congenital heart disease
The number of patients suffering from CHD is on the rise. High-risk individuals constitute only a small minority of this important patient population. Physicians in the past often restricted patients with CHD from engaging in regular physical activity because of a perceived risk of exercise-related complications. Patients who have survived to adulthood have been brought up in a culture advocating a sedentary lifestyle. Haemodynamic complications accelerating disease progression and SCD are the reasons behind this school of thought. In the absence of robust evidence supporting these perceptions, the challenge for clinicians is to ensure safe participation in regular physical activity that is tailored to the individual. Physical activity is safe for the vast majority of patients with CHD. The long-term implications of physical inactivity should be addressed. Children with CHD are after all more likely to be overweight compared to their healthy counterparts, reaffirming the importance of encouraging young individuals with CHD to exercise.
Sudden cardiac death and congenital heart disease
Most subjects harbouring congenital heart disease (CHD) live a normal life, possibly engaging in significant athletic activity. Moderate- to high-intensity exercise is safe in most cases of adult congenital heart disease (ACHD) [4-6]. Extreme exercise may, however, provoke arrhythmias in individuals with complex CHD. The reduced exercise tolerance in this subgroup is often not compatible with high-intensity physical activity, which is why athletes diagnosed with CHD are often low risk. The risk of SCD in CHD is in fact rare (<0.1% per year) [7], with only 8% of deaths occurring during physical activity [8].
Confirmed or presumed arrhythmic sequelae during physical activity confer significant morbidity in those with CHD. In a large population-based study of SCD in this patient group, exercise-related SCD was far commoner in those with undiagnosed CHD (18% vs 4%) [9]. SCD was 9.6 times higher amongst patients with these disorders compared with patients not harbouring congenital anomalies [9]. Both these points support cardiac screening in athletic individuals.
Screening for congenital heart disease
A comprehensive history and physical examination, as per European Society of Cardiology (ESC) recommendations, is a prerequisite for any pre-participation screening protocol [2].
Symptoms
Athletes suffering from ACHD may complain of cardiac symptoms such as exertional chest pain, dizziness, palpitations or syncope. Any drop in exercise capacity may also indicate significant cardiac limitation. Exertional symptoms in patients with ACHD may reflect inadequate cardiac output and arrhythmias.
Surgical history
Physicians should also take a detailed account of any relevant cardiac surgical history. This should include but should not be limited to age of surgery, number of procedures, location of scars, pacing devices and surgical notes if available.
Family history
In some forms of ACHD, current practice favours family screening. This is now well recognised in bicuspid aortic valve disease, Marfan’s syndrome and chromosomal/monogenic disorders which are linked to CHD [10]. This should also be explored in a screening process.
Physical examination
Physical examination may also be useful in diagnosing athletes with CHD. The signs are often non-specific. These may include clubbing, central cyanosis, surgical scars, irregular pulse, features of right and/or left ventricular dysfunction. Other uncommon signs including eye and ear abnormalities, dysmorphic facies, polydactyly, skeletal defects, neurological abnormalities, gastrointestinal and urological defects may imply syndromic disorders. Admittedly, rare syndromic disorders such as DiGeorge syndrome, Williams syndrome, Alagille syndrome and Noonan syndrome are uncommon in athletes as multi-organ involvement often limits athletic performance. These signs may however be more relevant in more common forms of ACHD such as Marfan’s syndrome.
12-lead electrocardiogram
The ECG is another important pillar in the ESC screening algorithm. Admittedly, ECG patterns are rarely specific to particular CHD phenotypes. Certain subtypes of CHD are associated with specific ECG findings (Table 1) [11]. Certain ECG patterns also offer important prognostic information. QRS prolongation is a marker of right ventricular dysfunction and dilatation in Ebstein’s anomaly [12, 13]. A QRS width exceeding 180 ms also confers a worse outcome in patients with repaired tetralogy of Fallot [11]. QRS fragmentation is linked with arrhythmogenic potential and disease severity in patients with Ebstein’s anomaly [12]. Atrial flutter and atrial fibrillation after a Senning or Mustard repair for transposition of the great arteries is also an independent predictor of SCD [14].
Table 1. Specific ECG patterns in various types of congenital heart disease.
| Congenital heart disease | ECG patterns |
|---|---|
| Dextrocardia |
|
| Situ Inversus |
|
| Right atrial isomerism |
|
| Left atrial isomerism |
|
| Ebstein’s anomaly |
|
| Surgical repaired tetralogy of Fallot |
|
| Surgical repaired transposition of great arteries |
|
General considerations in physically active individuals with congenital heart disease
The severity and prognosis of different CHD lesions vary considerably. The interindividual variation for a given lesion is also evident. A ventricular septal defect (VSD) may be small and clinically insignificant, but a large defect may lead to failure to thrive or heart failure in infancy. An atrial septal defect (ASD) may also be small with no clinical sequelae, though a large ASD may lead to right ventricular failure and pulmonary hypertension.
Patients with mild CHD (small ASD or VSD) who do not have any symptoms will not have any exercise restrictions, provided surveillance is carried out as advised. Others will require definite long-term surveillance as clinical progression is a possibility. A bicuspid aortic valve may become stenotic, regurgitant or co-exist with an aortopathy. An athlete who has a family history of Marfan’s syndrome who happens to be gene positive should also be monitored for aortic dilatation and aneurysms. An even smaller group will have undergone surgery earlier on in their life. Valve incompetence and arrhythmias are common complications in such a scenario. Arrhythmias and ventricular dysfunction assume a more prominent role with increasing age [15]. Arrhythmia ablation due to scar-related re-entry and a redo valve or conduit surgery are more apparent with increasing age [16]. Athletes with a more conservative exercise prescription earlier in their life may also be at risk of cardiovascular disease.
Physical activity in patients with CHD is safe for most patients. The increased demand during exercise, however, merits routine surveillance in those individuals who decide to engage in regular physical activity. Competitive athletes should undergo a yearly evaluation. The scope of the evaluation is to assess cardiac physiology at rest and during exercise. A risk assessment can then help the physician to prescribe exercise safely, based on the static and dynamic components of the discipline. This evaluation should include a clinical examination, 12-lead resting ECG, echocardiogram and exercise stress test, preferably cardiopulmonary exercise testing (CPET) if available [15].
Assessing a patient with congenital heart disease
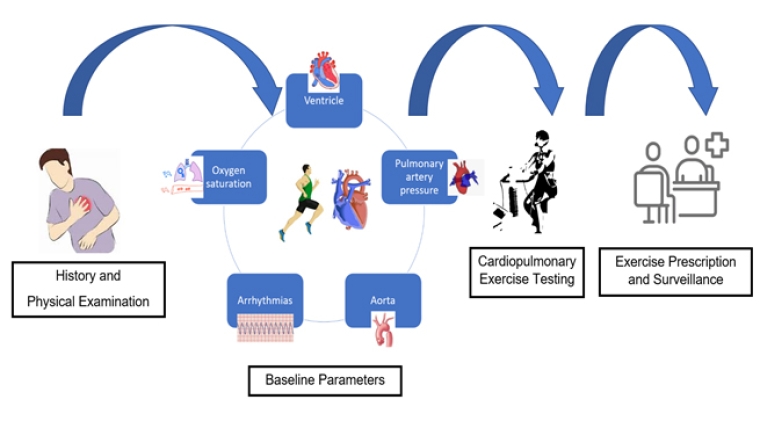
The heterogeneity in pathophysiology and functional status of patients with CHD have led to the creation of a robust individualised algorithm which aims to individualise exercise prescription in this patient subgroup. The latest ESC recommendations advise evaluating athletes with known or newly diagnosed CHD based on haemodynamic and electrophysiological parameters, rather than focusing on the specific anatomical anomaly [6,15]. The history, physical examination, physiological assessment, response during exercise and a formal prescription are the steps involved in this process. The aim of the physiological evaluation is to look at a) ventricular function, b) pulmonary artery pressure (PAP), c) aortic dimensions, d) arrhythmias at rest and during exercise, and e) arterial oxygen saturation at rest and during exercise [15]. Using an anatomical diagnosis to help prescribe exercise has been shown to correlate poorly with potential complications. A proposed five-step methodology will be discussed in the next section (Figure 1).
Step 1. History and physical examination
As outlined previously, a history and physical examination are very important. A full exercise and sports participation history should be acquired. Details about the planned and current sports activity will help to assess the static component and intensity. Assessing the environment where the sporting discipline will be performed is also key. In particular, exercise at high altitude may lead to reduced cardiac output, hypercoagulability and impaired oxygenation. The increased risk of arrhythmias and heart failure in such conditions should preclude a small group of high-risk athletes (cyanotic, unrepaired, or palliated CHD or CHD with pulmonary hypertension) from engaging in competitive sports [6].
Step 2. Five baseline parameters
Ventricular function
Ventricular function with echocardiography will help to establish whether systolic function is reduced (ejection fraction (EF) <55%). It is also used to quantify the degree of impairment classified as mild (EF 45-55%), moderate (EF 30-45%) and severe (EF <30%). Determining baseline function helps to ascertain risk, whilst it is also useful when monitoring the impact of exercise training on systolic function [15]. Echocardiography may also help to assess atrioventricular valve function (stenosis and regurgitation), outflow tract obstruction and chamber dimensions. Exercise echocardiography may help to assess cardiac reserve, dynamic outflow tract obstruction and valve function during exercise. Cardiac magnetic resonance (CMR) imaging may be a better option in complex patients, especially when evaluating the right ventricle and suspecting myocardial scar.
Pulmonary artery pressure
Pulmonary artery pressure in combination with peak tricuspid valve regurgitant velocity are two important parameters used to diagnose pulmonary hypertension (PH). It is defined as a mean PAP >20 mmHg. PH is unlikely if the peak tricuspid valve regurgitant velocity is <2.8 m/s. Intracardiac shunts may lead to volume and pressure overload in the right ventricle. Shunt reversal and increased pulmonary vascular resistance may take place years later, which is known as Eisenmenger syndrome. The altered haemodynamics and interventricular dyssynchrony may have a negative impact on contractile reserve during exercise. Athletes with significant PH rarely participate in competitive sport. The decreased aerobic efficiency and cardiac limitation will invariably limit their ability to compete at an elite level. Competitive athletes with mildly elevated PAP may however present to a clinic for sporting eligibility assessment. PAP is augmented with altitude training, age and exercise [17]. PH can also coexist with pulmonary artery stenosis or pulmonary valve stenosis. It may also be a late postoperative complication after complex CHD surgery. Surveillance with echocardiography is very important. When possible, CPET evaluation can give useful diagnostic information on oxygen consumption (VO2) and ventilatory efficiency (VE/VCO2) [15].
Aortic assessment
Aortic assessment is another important parameter in most CHD patients. Echocardiography and CMR imaging are the two main modalities used for this evaluation. Aortopathies are strongly associated with Marfan’s syndrome, tetralogy of Fallot, aortic coarctation and bicuspid aortic valve [15]. Aortic dilatation and aneurysms may develop throughout an athlete’s career. A small minority of athletes have enlarged aortic dimensions [18]; little is known on whether the cumulative effect of exercise in CHD athletes augments this phenomenon. The presence of exercise-induced hypertension should raise suspicion for aortic coarctation [19]. Contact sports should be avoided in cases of dilated aorta >50 mm or when >45 mm in the presence of a Marfanoid habitus, family history of aortic dissection or a relevant mutation in the FBN1 gene.
Arrhythmic risk
Evaluating an athlete’s arrhythmic risk is also crucial as arrhythmias account for 25% of all CHD hospital admissions [20]. Male gender, increasing age, heart failure, tetralogy of Fallot, congenitally corrected transposition of the great arteries, atrioventricular septal defect and sleep apnoea are independent risk factors. Symptoms suggestive of arrhythmias should be evaluated thoroughly. An evaluation may include exercise testing, ambulatory ECG monitoring, and loop recorder or electrophysiological testing. CMR may be necessary if scar-related ventricular arrhythmias are suspected. Patients with CHD have an increased risk of thromboembolic events, which is why anticoagulant therapy is strongly advised in cases of atrial fibrillation or flutter. Contact sports in these athletes should be discouraged. Anti-arrhythmic therapy may negatively impact on athletic performance because of the negative chronotropic effect. Treatment should be discussed on a case-by-case basis. A low threshold for ablation is strongly advised. Implantable defibrillators may be necessary in some cases. Competitive sports in these high-risk individuals are also not recommended.
Arterial saturation
Arterial saturation monitoring with pulse oximetry may help to rule in a significant right to left intracardiac shunt. Residual shunts may be present even after surgical correction of a cardiac anomaly. Oximetry monitoring during exercise is also essential as a ventilatory limitation to exercise is a possibility [15]. CPET can help to assess baseline functional capacity, breathing reserve and oxygenation during exercise.
Step 3. Cardiopulmonary exercise testing
CPET has an invaluable role in the risk stratification of patients with CHD. CPET allows assessment of PAP, contractile reserve, exercise-induced arrhythmias and altered haemodynamics [15]. It can also help to ascertain ventilatory limitations to exercise, a phenomenon which may be present in individuals with previous thoracotomy or lung disease. Peak oxygen consumption (VO2max), gas exchange efficiency (VE/VCO2), oxygenation, blood pressure, oxygen pulse and ECG monitoring are all useful for determining prognosis and risk [6]. CPET has the advantage of evaluating contractile reserve in complex CHD. VO2max is also useful for surveillance purposes as it offers excellent reproducibility.
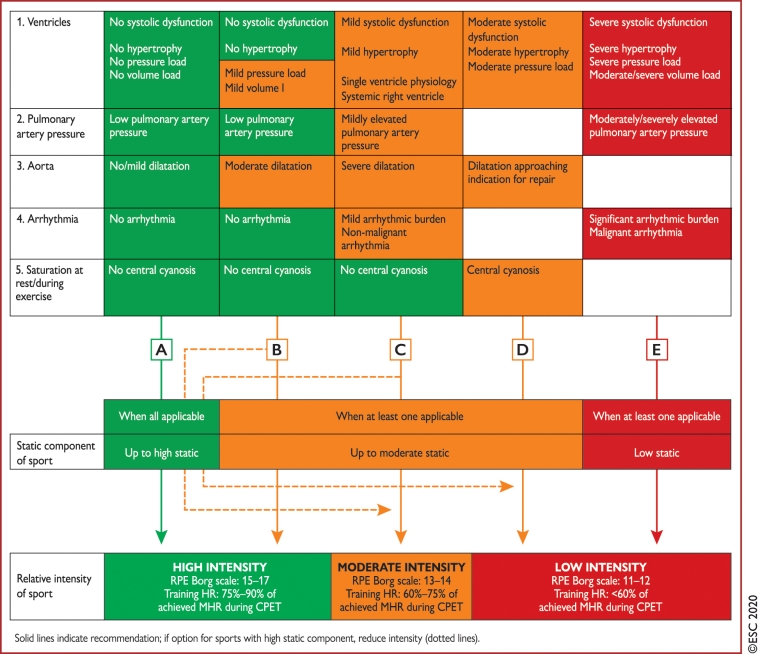
Step 4. Exercise intensity and prescription
As outlined in previous sections, the initial discussion should include a detailed sporting history. Following this comprehensive evaluation, an exercise recommendation should include the advised intensity and overall volume of exercise. The physician should also advise the individual on whether competitive sport is allowed. In the vast majority of individuals with low-risk CHD, normal physiological assessment of all five parameters should not discourage individuals from engaging in high-intensity and high static sports. As outlined in Figure 2, the presence of one or more abnormalities in this assessment should prompt the clinician to advise moderate or low static disciplines, favouring a lower dynamic component in higher-risk individuals. Individuals with severe structural, haemodynamic or electrophysiological complications should be restricted to recreational sports. Kindly refer to the full guidelines for more comprehensive guidance on competitive sport eligibility (Figure 2) [15].
Figure 2. Pre-participation assessment of individuals with congenital heart disease. Reproduced from [15] (Pelliccia A, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease: The Task Force on sports cardiology and exercise in patients with cardiovascular disease of the European Society of Cardiology (ESC). Eur Heart J. 2021;42:17-96) by permission of Oxford University Press on behalf of the European Society of Cardiology.
Sports Cardiology and exercise in patients with cardiovascular disease Guidelines
Step 5. Follow-up
Serial assessment should be performed in all patients with CHD. The frequency and method of evaluation will have to depend on the patient demographics, relevant symptoms, previous physiological assessments, the anatomical diagnosis and the level of commitment or competition.
Gaps in the literature
Several gaps in the literature still exist in this unique cohort. The relationship between exercise intensity and the arrhythmogenic potential in physically active patients with CHD is still unknown. The effects of exercise on the natural history of aortopathy has also not been explored. The optimal safe exercise dose in CHD is also relatively unknown at this point.
Conclusion
The number of subjects diagnosed with CHD is on the rise. The comprehensive assessment algorithm outlined in this document and in the relevant guidelines offers physicians a stepwise evaluation protocol [6,15]. Based on electrophysiological and haemodynamic parameters, healthcare professionals are now in a better position to provide individualised advice to athletes who wish to participate in competitive sport. Only a minority of high-risk individuals with CHD should be restricted from high-intensity physical activity, as outlined in this document.