Introduction
Amyloidosis refers to the extracellular deposition of fibrils that are composed of low molecular weight subunits of a variety of serum proteins [1]. Amyloid can occur in a variety of organs, with the involvement of heart, kidney, liver and autonomic nervous system being most often responsible for the observed morbidity and mortality. Risk factors that increase the risk of amyloidosis include advanced age, male gender, black race, coexistent chronic or infectious diseases and family history (given that some types of amyloidosis are hereditary).
Cardiac amyloidosis is a disorder caused by amyloid fibril deposition in the extracellular space of the heart [2]. Among the different types of amyloidosis, nearly all cases of clinical cardiac amyloidosis (>95%) are caused by light chain amyloidosis (AL) and transthyretin amyloidosis (ATTR) [3,4]. The infiltrative process in the heart leads to progressive dysfunction of the cardiac muscle, while the conduction system of the heart is also affected [5]. Amyloid cardiomyopathy is emerging as an important and often underdiagnosed cause of heart failure and cardiac arrhythmias, especially in older adults [3,6].
Advances in cardiac imaging and improved awareness among physicians have facilitated the diagnosis of cardiac amyloidosis over the last decade. Involvement of the heart in the setting of amyloidosis carries an adverse prognosis. Timely diagnosis is of the greatest importance for appropriate treatment modalities that may crucially modify the natural history of the disease [6].
Forms and epidemiology
AL amyloidosis results from the deposition of immunoglobin light chains produced by a plasma-cell dyscrasia. It is a rare condition with an incidence of approximately 2,500 to 5,000 new cases in the USA per year [1]. A recent study reported a significant increase between 2007 and 2015 in the incidence and prevalence rates of AL amyloidosis among individuals aged 18-64 years; it is estimated that nearly 12,000 patients with AL amyloidosis live in the USA [7].
Hereditary ATTR amyloidosis is caused by a genetic mutation predisposing to instability of the tetrameric structure of transthyretin. Transthyretin is a liver synthetised protein that transports thyroid hormone and retinol (vitamin A). There is no evidence that there is a link between thyroid disease and amyloidosis. There are more than 120 identified amyloidogenic transthyretin mutations, with some genetic variants being endemic in specific geographic regions or ethnic groups. Different transthyretin mutations are associated with diverse age of onset and risk of cardiomyopathy. The most frequently described transthyretin mutation is the Val30Met variant, while the Ile68Leu and Leu111Met variants are associated with a predominantly cardiac phenotype [8-10].
Published data on the epidemiology of cardiac amyloidosis are based mainly on single-centre studies or population registries. A recent study among Medicare beneficiaries aged 365 years in the USA showed an increase in both the incidence and prevalence rates of cardiac amyloidosis from 2000 to 2012. Among hospitalised patients with heart failure, men and women were equally affected; 85% of patients were white [11].
Data from the THAOS registry showed that ATTR amyloidosis primarily affects elderly men with a cardiac predominant phenotype [12]. The prevalence of wild type (non-hereditary) ATTR amyloidosis increases with age with nearly all patients being >60 years of age. Patients with wild-type ATTR are mostly men, though data from recent studies suggest that a significant proportion are women [13]. Cardiac amyloidosis is the dominant feature of wild-type ATTR [3,11].
Clinical presentation and diagnosis
Cardiac involvement in amyloidosis, termed cardiac amyloidosis or amyloid cardiomyopathy, typically presents with heart failure symptoms and signs with prominent features of right ventricular failure (peripheral congestion) including lower extremity oedema, jugular vein distention, hepatic congestion and ascites as well as dyspnoea. In addition, patients may present with syncope or pre-syncope as the conduction system may be affected by amyloid deposits [14]. Extracardiac involvement varies among different types of amyloidosis; the clinical manifestations of AL and ATTR amyloidosis are summarised in Table 1.
Table 1. Clinical manifestations of AL and ATTR amyloidosis (in order of frequency).
| Amyloidosis subtype | Clinical manifestations |
|---|---|
| AL amyloidosis |
|
| ATTR amyloidosis |
|
The diagnosis of cardiac amyloidosis depends on a high degree of clinical suspicion and is often delayed due to the lack of disease awareness and the heterogeneity of symptoms at presentation. Most patients are asymptomatic until a late stage of disease and, even then, symptoms may be non-specific [4,6,14].
When to suspect cardiac amyloidosis
Some of the most common settings in which clinical suspicion of amyloidosis should be raised include (i) patients with unexplained left ventricular hypertrophy (with or without heart failure or syncope); (ii) patients with heart failure and symptoms/signs of amyloidosis such as bilateral carpal tunnel syndrome, peripheral neuropathy, renal dysfunction, and others; (iii) patients with aortic stenosis and echocardiographic features associated with cardiac amyloidosis including low-flow, low-gradient aortic stenosis, myocardial granular sparkling, abnormal left ventricular global longitudinal change and others [6,14].
Diagnostic work-up
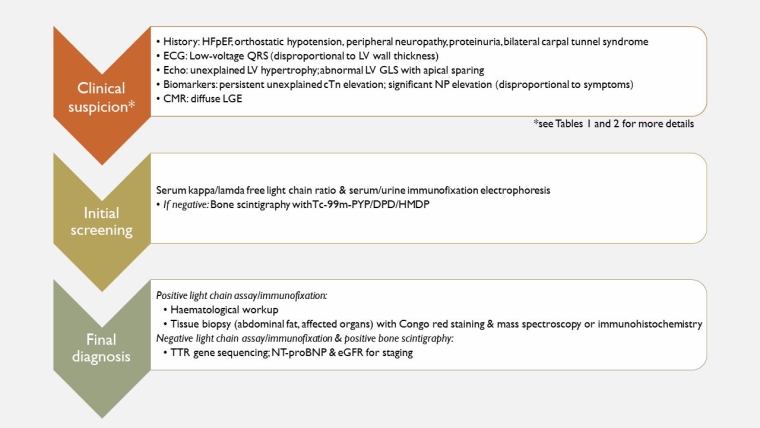
The initial diagnostic evaluation of a patient with suspected cardiac amyloidosis includes a thorough clinical examination and history taking to identify and assess cardiac and extracardiac symptoms and signs of amyloidosis, as described in Table 1.
The main cardiac findings are summarised in Table 2. Low QRS voltages in the electrocardiogram, discordant to left ventricular wall thickness, raise the suspicion of cardiac amyloidosis, whilst an echocardiogram is the initial cardiac imaging test for patients with suspected cardiac amyloidosis [6,15]. Echocardiography may reveal several abnormalities, including left ventricular hypertrophy with or without right ventricular free-wall hypertrophy, bi-atrial dilatation, myocardial granular sparkling in non-harmonic imaging, thickening of mitral and tricuspid valve leaflets and atrial septum, low-flow/low-gradient aortic stenosis, diastolic dysfunction of varying severity and abnormal left ventricular global longitudinal strain, typically with apical sparing. Tissue characterisation with cardiovascular magnetic resonance (CMR) imaging may typically reveal diffuse subendocardial or transmural late gadolinium enhancement as well as increase in extracellular volume with T1 mapping.
Table 2. Main findings in cardiac amyloidosis.
| Type of assessment | Main findings |
| Clinical |
|
| Electrocardiography |
|
| Echocardiography |
|
| Biomarkers |
|
| Cardiac magnetic resonance |
|
AV: atrioventricular; cTn: cardiac troponin; GLS: global longitudinal strain; HF: heart failure; LGE: late gadolinium enhancement; LV: left ventricle; NP: natriuretic peptide; RV: right ventricle
As far as laboratory tests are concerned, abnormal kidney and liver function tests are found in the context of kidney disease or congestive hepatopathy. Cardiac biomarkers (natriuretic peptides, cardiac troponins) are commonly elevated in patients with amyloid cardiomyopathy. Slightly and persistently elevated cardiac troponins in the absence of myocardial ischaemia, especially in patients with AL amyloidosis and a significant increase in natriuretic peptides disproportional to heart failure symptoms are “red flags” for cardiac amyloidosis [3,4,6]. Elevation of these cardiac biomarkers in asymptomatic patients highlights their role as disease markers.
In the presence of cardiac and other findings suggestive of amyloidosis, the next step is to perform serum kappa/lamda free light chain ratio analysis, serum protein immunofixation and urine protein immunofixation. If monoclonal protein is identified by one or more of these tests, referral to a haematologist is recommended for evaluation and further assessment. Non-cardiac tissue biopsy (fat pad, liver, kidney) and CMR findings consistent with amyloid cardiomyopathy confirm the diagnosis. If monoclonal protein is not identified by any of the three tests mentioned above, further management is based upon the results of bone tracer scintigraphy with technetium 99m (99mTc-pyrophosphate [PYP], 99mTc 3,3-diphosphono-1,2-propanodicarboxylic acid [DPD], or 99mTc-hydroxymethylene diphosphonate [HMDP]) to identify the presence and extent of cardiac uptake. Bone tracer cardiac scintigraphy is a hallmark test for identifying ATTR amyloidosis, and the presence of grade 2 or 3 scintigraphy has high sensitivity and specificity for cardiac amyloidosis compared with tissue biopsy. In patients with suspected AL amyloidosis, evaluation typically includes bone marrow biopsy and other tissue biopsy [6,14]. Progress in diagnostic techniques, including echocardiography, cardiac magnetic resonance and bone scintigraphy, has led to a non-invasive diagnostic approach, thus limiting the need for endomyocardial biopsy. If the diagnosis of cardiac amyloidosis is not confirmed by either non-invasive methods or tissue biopsy other than myocardium, endomyocardial biopsy is recommended. Moreover, endomyocardial biopsy is indicated in cases where there is a need for differential diagnosis from cardiomyopathies.
Α proposed diagnostic algorithm for cardiac amyloidosis is shown in Figure 1.
Therapy
The cornerstones of amyloidosis management are heart failure therapy and treatment of the underlying disease.
Heart failure management in amyloidosis
Loop diuretics constitutes a mainstay of the management of heart failure in amyloidosis. There are no data to suggest that the three life-saving therapies in heart failure with reduced ejection fraction (angiotensin-converting enzyme inhibitors/angiotensin receptor blockers/angiotensin receptor neprilysin inhibitors, beta-blockers and mineralocorticoid receptor antagonists) improve survival, symptoms and quality of life in patients with cardiac amyloidosis. In addition, these medications are often poorly tolerated, resulting in hypotension [16]. A possible explanation for these findings is the complex pathophysiology of alterations in the heart muscle by amyloid infiltration; the combination of small to normal ventricular size, significant diastolic dysfunction and impaired atrial contraction results in decreased stroke volume and cardiac output while the intracardiac pressures are frequently elevated. Heart transplantation in carefully selected patients can be an effective therapeutic option.
Treatment of underlying disease
Specific therapy for AL amyloidosis
The main modalities of treatment in AL amyloidosis are chemotherapy and/or autologous stem cell transplantation targeting the underlying plasma-cell clone responsible for AL amyloid formation. Bortezomib, cyclophosphamide and dexamethasone constitute the most common initial chemotherapy regimens resulting in satisfactory haematological response rates.
Specific therapy for ATTR amyloidosis
For patients with ATTR cardiomyopathy with New York Heart Association Class I to III, tafamidis is an effective therapy. Tafamidis stabilises the transthyretin tetramer leading to reduced formation of TTR amyloid. Tafamidis was found to reduce mortality and cardiovascular-related hospitalisations while it further improved quality of life and reduced declines in functional capacity [16].
Patients with hereditary ATTR cardiomyopathy may also undergo evaluation for liver transplantation. Liver transplantation removes the mutant amyloidogenic TTR in hereditary ATTR cardiomyopathy, as the source of amyloidogenic protein is the liver. Transplantation of the liver is not however indicated in wild-type ATTR amyloidosis.
Several agents for ATTR amyloidosis are under investigation in trials, but their effect in amyloid cardiomyopathy has not been established. Patisiran and inotersen are RNA-targeted therapies interfering with TTR synthesis in the liver and thus reducing the ability of misfolded monomer to form amyloid deposits. The drugs used in ATTR cardiomyopathy are summarised in Table 3.
Table 3. Drugs for the treatment of ATTR amyloidosis.
|
Mode of action
|
Drug
|
Route of administration
|
Current indications
|
|---|---|---|---|
| TTR protein stabilisation | Tafamidis | Oral | Cardiomyopathy |
| Diflunisal | Oral | Off-label usage | |
| AG10 | Under investigation | ||
| TTR protein synthesis silencing | Patisiran | Intravenous | Neuropathy |
| Inotersen | Subcutaneous | Neuropathy | |
| TTR fibril degradation | Doxycycline/TUDCA | Oral | Off-label usage |
| PRX004 | Under investigation |
TUDCA: tauroursodeoxycholic acid
Conclusions
Cardiac amyloidosis is a challenging clinical entity to diagnose and treat. Recent advances in cardiac imaging and diagnostic strategies allow the early identification of the growing population confronted in the clinical practice, while the emergence of effective therapies will likely translate into improved clinical outcomes.