Physiopathology notes: arrhythmias associated with cancer, due to cancer and due to cancer therapy
As with many other cardiovascular diseases (CVD), the relationship between arrhythmias and cancer is very tight; moreover, it shows some quite specific and interesting aspects, essentially due to the electrophysiology modifications.
Maybe in the future we will create the “arrhythmia-oncology subspecialty”.
In cancer patients, arrhythmias may be due to the following conditions:
- Cardiac tumours or cardiac metastasis which, when they involve myocardial and conduction tissue, may interrupt or slow the conduction velocity of the cardiac impulse leading to sinoatrial or atrioventricular (AV) blocks or to the generation of possible re-entrant circuits and, as a consequence, to re-entrant atrial or ventricular arrhythmias.
- Tumours involving the cervical or mediastinal nervous autonomic system (Pancoast syndrome) may impair the autonomous nervous system function. In the case of appropriate substrates, arrhythmias are facilitated.
- Cardiac involvement of conditions associated with cancer, e.g., cardiac amyloidosis with cardiac conduction system direct damage or paraneoplastic conditions leading to electrolyte abnormalities or production of inflammatory or other kinds of products modifying the cell action potential.
- Conditions related to the neoplastic condition of the patient, such as electrolyte abnormalities due to vomiting, diarrhoea or cachexia or to the administration of drugs with potentially pro-arrhythmic effects.
- The direct toxicity of cancer therapy which is possible with many cancer drug families leading to a direct myocardial lesion (for example immunotherapy myocarditis) or to apoptosis (such as anthracyclines) or, alternatively or at the same time, to direct modifications of ion channels or other regulatory mechanisms related to the membrane action potential.
- Radiotherapy lesions of the conduction system (which are now rare but still possible).
Moreover, every cardiac disease may co-exist together with a cancer for very simple epidemiological reasons (shared risk factors between CVD and cancer, old age, etc.).
Almost all of these conditions, frequently presenting in association, constitute the “Coumel triangle”, which is at the basis of every arrhythmia - substrate, trigger and autonomic nervous system balance.
Epidemiology
A true evaluation of the incidence of arrhythmias in cancer patients is practically impossible. This is because of the often very complicated clinical picture and as a result of the underestimation of the arrhythmic risk in these patients.
Arrhythmic events in oncologic subjects are mixed and confused due to the complexity of this condition. They may not be recognised because other types of severe symptoms may be confused with tachycardia due to anaemia or anxiety. Arrhythmias may also be the terminal event of the neoplastic disease.
Generally speaking, cancer and arrhythmic diseases are diseases of the elderly. Therefore, it may be argued that, particularly in the elderly neoplastic patient, arrhythmias are much more frequent than in the general population.
It is clear, however, that, in some cancers, arrhythmias are less common than in other conditions. For instance, the direct invasion of myocardial metastasis is less frequent, while amyloid relatively often complicates myeloma.
Clinical implications
Every arrhythmia further complicates the clinical picture of the patient with cancer.
The subject may show symptoms such as palpitations which may be, as previously mentioned, misinterpreted, or symptoms of heart failure due to the haemodynamic impairment of a high (or a low in case of AV block) heart rate. So, arrhythmias may lead to a deterioration of a precarious clinical equilibrium, accelerating the evolution of the cancer course. In parallel, arrhythmias contribute to a worse quality of life for the subject.
While some conditions are quite difficult to manage and to treat, many pro-arrhythmic conditions may be predictable and easily corrected with a minimum of attention (Table 1).
Table 1. Pro-arrhythmic factors.
| Correctable | Not correctable |
|---|---|
|
Electrolyte imbalance
Hypothyroidism
|
Family history of sudden death (“occult” arrhythmogenic heritable diseases)
An updated list of QT-prolonging drugs may be found at: |
The other interesting (and in some instances manageable) aspect is the direct arrhythmic effect of many cancer drugs (Table 2). The real incidence of the problem is difficult to evaluate. In any case, patients undergoing some specific treatments should undergo a careful cardiologic evaluation, which should be periodically repeated with a frequency according to the drug itself and to the clinical condition.
These drugs may act directly, influencing the action potential of myocardial cells.
Table 2. Chemotherapy drugs and specific arrhythmic conditions.
| Arrhythmia | Drug |
|---|---|
| Sinus bradycardia |
Arsenic trioxide, bortezomib, capecitabine, cisplatin, cyclophosphamide, doxorubicin, epirubicin, 5-FU, ifosfamide, |
| Sinus tachycardia |
Anthracyclines, carmustine |
| AV block |
Anthracyclines, arsenic trioxide, bortezomib, cyclophosphamide, 5-FU, mitoxantrone, rituximab, taxanes, thalidomide |
| Other conduction defects |
Anthracyclines, cisplatin, 5-FU, imatinib, taxanes |
| Atrial fibrillation |
Alkylating agents (cisplatin, cyclophosphamide, ifosfamide, melphalan), anthracyclines, antimetabolites (capecitabine, |
| Supraventricular tachycardia |
Alkylating agents (cisplatin, cyclophosphamide, ifosfamide, melphalan), amsacrine, anthracyclines, antimetabolites (capecitabine, 5-FU, methotrexate), bortezomib, doxorubicin, IL-2, interferons, paclitaxel, ponatinib, romidepsin |
| Ventricular tachycardia/fibrillation |
Alkylating agents (cisplatin, cyclophosphamide, ifosfamide), amsacrine, antimetabolites (capecitabine, 5-FU, gemcitabine), arsenic trioxide, doxorubicin, interferons, IL-2, methothrexate, paclitaxel, proteasome inhibitors |
| Sudden death |
Anthracyclines (reported as very rare), arsenic trioxide (secondary to torsade de pointes), 5-FU (probably related to ischaemia and coronary spasm), interferons, nilotinib, romidepsin. |
The cell action potential and its electrophysiologic properties may be modified affecting the ion currents by a direct modification leading to a “gain” of function or a “loss” of function of Na, K and Ca ion channels. The same modifications may be due to intracellular mechanisms impairing Ca homeostasis/Ca handling, creating an overload of intracellular Ca ions, modifying SERCA, calmodulins, calcineurins and other pathways or through modifications of the Inositol-3P, a regulator of function of some ion channels. hERG ion channel function may be modified directly by some chemotherapy agents or indirectly, acting on the hERG “trafficking”, which is the very complex process of production and catabolism of these cell structures.
The consequences of the variation of the action potential consist in the modification of conduction velocity and in refractoriness of myocardial specific conduction or common fibres, leading to a favourable condition for the creation of a functional re-entry circuit, the basis of most of the common arrhythmias.
The most common example of modification of the action potential is the occurrence of a long QT and of the severe complication of a torsade de pointes which may lead to a sudden arrhythmic death.
Anyway, it may be hypothesised that other kinds of arrhythmic conditions may also be induced by cancer drugs acting on the ion channels with a “loss of function” instead of a “gain of function” and vice versa and, as a consequence, with the phenotypic appearance of a Brugada pattern or a short QT, instead of a long QT. Research in this field is required to go into more depth concerning these hypotheses.
More research is also needed about the true occurrence of clinical events due to these conditions. The most consistent data concern chemotherapy-induced long QT syndrome (LQTS). Apart from arsenic trioxide with a significant occurrence of LQTS and, in some instances, also of torsade de pointes, the number of events relative to other drugs seems very low.
The mean prolongation of the QTc period shown in the literature varies according to the different drugs from 3 to 36 ms, a % increase of the QTc >60 msec in 0.34-23.8% and a QTc of more than 500 msec in 4.3-8%. The occurrence of torsade de pointes seems very low, at the level of case reports.
Sinus bradycardia and AV block
Sinus bradycardia is generally a rare and transitory complication of some chemotherapies.
Paclitaxel
Paclitaxel induces transitory episodes in about 30% of treatments [1]. Generally, it goes without symptoms and is unrecognised.
- Generally, sinus bradycardia and/or AV block occur during the 1st and 2nd cycle of therapy and disappear spontaneously after 48-72 hours of drug discontinuation.
- Cardiac monitoring is required during the first hours of infusion of the drug.
- Drug withdrawal should be considered if AV block occurs.
- A pacemaker (PM) implant (temporary or permanent) should be considered according to symptom severity or if no alternatives to the treatment are possible.
- Antihistamine and corticosteroids seem to reduce the risk.
Thalidomide
Thalidomide sinus bradycardia occurs in as many as 50% of patients treated with multiple myeloma. Only one single case report showed syncope due to thalidomide. Caution should be paid to concomitant treatment with beta-blockers, verapamil, diltiazem, digoxin and other drugs potentially inducing sinus bradycardia. Previous exposition to doroxubicin, cyclophosphamide or radiotherapy seems to enhance sinus bradycardia risk.
From a practical point of view:
- Caution should be exercised concerning symptoms such as fatigue, vertigo, syncope
- Thalidomide should be reduced with a heart rate of 50-60/min with symptoms.
- Thalidomide should be withdrawn with heart rate <50/min.
- The condition disappears after drug suspension. In myeloma patients without alternatives to thalidomide, an advanced AV block is an indication for a PM implant.
- The exclusion of a concomitant hypothyroidism should be carried out by dosing thyroid hormones.
Tyrosine kinase inhibitors (TKIs)
Sinus bradycardia may occur with pazopanib, or bevacizumab in combination with vorinostat. Sunitinib may induce hypothyroidism and sinus bradycardia as a consequence [2].
Anaplastic lymphoma kinase (ALK) inhibitors
With ALK inhibitor use, 15% of patients treated with crizotinib and 4% with ceritinib may show sinus bradycardia.
Immunotherapy
Concerning immunotherapy, advanced AV block may be seen during the occurrence of myocarditis induced by these drugs. The Treatment with corticosteroids generally leads to the resolution of the condition, but its persistence is an indication to a PM implant (and/or an automated implantable cardioverter defibrillator [AICD] if persistent ejection fraction [EF] depression is present according to guidelines [GLs]).
Radiotherapy
Radiotherapy may generate conduction tissue fibrosis and sick sinus syndrome or AV block. These conditions may only become apparent after many years of latency. As many as 27% of patients require a PM implant [3].
QT prolongation
QTc monitoring is one of the most important preventive measures in the treatment of many cancer patients.
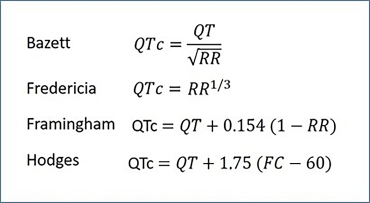
The Bazett formula is commonly used in the general population, while for cancer patients it is recommended to use the Fridericia formula according to the wide heart rate variations. An alternative is the Hodges formula, mainly for heart rates >90 bpm [4].
Figure 1. QTc calculation formula.
Arsenic trioxide
Arsenic trioxide is utilised for patients with relapsing promyelocytic leukaemia or unresponsive to other therapies. It prolongs QTc in about one third of patients by >60 ms. A QTc >500 ms may be observed in 65% of cases using the Bazett formula, but only in 24-32% using the Fridericia formula [5]. In fact, until now, only one case of torsade de pointes with spontaneous resolution has been shown in the literature.
TKIs
TKIs may induce a modest increase of QTc (about 15 msec) [6].
Vandetanib
Vandetanib QTc prolongation incidence has been reported in 18% of cases in long-lasting therapies [7]. It should not be used with a QTc >480 msec.
- By reason of its long half-life, ECG monitoring is recommended for QTc evaluation at baseline and 2, 4, 8 and 12 weeks from the start of treatment and then every three months
- Electrolytes and thyroid stimulating hormone (TSH) dosage should be checked at the same time
- Withdrawal should be considered if QTc reaches >500 msec and should be maintained until QTc is not <450 msec and, if the drug may not be exchanged with others, it may be restarted with half dosage.
Nilotinib
- Nilotinib QTc monitoring should be carried out at baseline and after 7 days from the start of treatment and at every change of dosage
- If QTc is >480 ms, therapy should be interrupted and permanently withdrawn if a long QT recurs after rechallenge, after correction of predisposing factors
- If QTc is between 450 and 480 ms, therapy should be rechallenged at half dosage or with a QTc <450 ms at full dosage.
Sunitinib
The effect of sunitinib on QTc is dose dependent. No specific recommendations apply for this drug, but an ECG control is opportune with concurrence of predisposing conditions.
Lapatinib
Lapatinib seems to lead to a dose-dependent QTc prolongation. Before its first administration, the presence of predisposing factors such as a congenital LQTS or the use of other QT-prolonging drugs should be evaluated.
Crizotinib
Crizotinib may induce sinus bradycardia with possible QTc prolongation and, before the start of this therapy, the presence of risk factors for QTc prolongation should be evaluated. ECG monitoring and electrolyte monitoring are recommended, particularly at the beginning of the treatment.
The treatment should be suspended with a QTc increase >60 msec with a QTc <500 msec, or totally and immediately withdrawn with a QTc >500 msec, particularly if arrhythmias, heart failure or other severe symptoms occur.
Ceritinib
Ceritinib rarely significantly increases the QTc interval, but its suspension or dosage reduction is recommended with a QTc >500 msec [8].
HDAC inhibitors
Romidepsin
About 10% of subjects treated with romidepsin might show a QTc prolongation which spontaneously disappears. Some sudden deaths have been reported and tight surveillance is warranted.
Vorinostat
Vorinostat prolongs QT in 3.5–6.0% of cases, dose dependently, with a greater torsade de pointes risk in females and older patients, due to a hERG channel blocking effect.
Panobinostat
Panobinostat is contraindicated in patients with myocardial infarction or unstable angina and with a
QTc >480 msec.
Vascular disrupting agents (VDAs)
VDAs have a potential but variable power to induce a QTc prolongation.
Ribociclib
Ribociclib increases of QTc are dose dependent, generally occur in the first four weeks of therapy and reverse with the drug interruption. An ECG control for QT evaluation should be carried out at 14 days and at the beginning of the second therapy cycle.
Palbociclib and abemaciclib
Palbociclib and abemaciclib do not increase QTc interval significantly.
Ventricular tachycardia
Paclitaxel, docetaxel and 5-FU
Paclitaxel, docetaxel and 5-FU may induce myocardial ischaemia, long QT and ventricular arrhythmias.
Ibrutinib
Ibrutinib ventricular fibrillation (VF) and ventricular tachycardia (VT) may also occur with a normal QTc interval. ECG monitoring and interruption of therapy should be considered with a QTc >500 msec.
Immunotherapy
Ventricular arrhythmias may be present in as many as 5-10% of subjects, are associated with a complicated myocarditis and have a mortality rate of 40%.
Radiotherapy
In young survivors of radiotherapy involving the chest, an incidence of VT of 3-5% has been observed. It increases to 8% in association with anthracyclines. Also, patients with a normal left ventricular function may have ventricular arrhythmias.
Prevention and management
All cancer patients with CVD should be considered at risk of chemotherapy-induced ventricular arrhythmias. An in-depth attempt to obtain the best treatment of the favouring condition should be tried before the cancer therapy, for example with myocardial revascularisation when required and with the optimal medical treatment of a left ventricular dysfunction.
Atrial fibrillation
AF is the most common arrhythmia in the general population (incidence 1.5-2%, prevalence up to 18% up to the age of 85). The incidence and prevalence of cancer also increase with age.
From a general point of view, AF may be considered “associated” with cancer, “due” to cancer or “due to cancer therapy”. AF and cancer association is not only an epidemiological issue. In lung resection, colectomy or oesophagostomy, AF occurs statistically more frequently, with a multifactorial genesis. Advanced age, diabetes, hypertension, CAD, obesity, obstructive sleep apnoea (OSA), valve diseases, electrolyte anomalies, and hypoxia are all risk factors for the development of AF. As we said earlier, an autonomic dysfunction due to tumour invasion of the peripheral nervous system or from pain and stress favours AF induction. Paraneoplastic conditions, inflammation and apoptosis factors are present in cancer and all may induce AF.
Finally, AF may complicate therapy with: cisplatin, 5-fluorouracile, doxorubicin, paclitaxel, docetaxel, isophosphamide, gemcitabine and mitoxantrone, ibrutinib, and high-dose corticosteroids.
Clinical consequences, prevention and management
AF may lead to worsening of symptoms and haemodynamic conditions and strongly increases thromboembolic risk, basally enhanced in the oncology situation, and its consequences. It can be found occasionally in an already severely ill multisymptomatic cancer patient or may be diagnosed after the occurrence of palpitation, dyspnoea or heart failure or syncope. The general conditions and the quality of life of the patient may be strongly impacted by AF. A high heart rate, the irregular R-R cycle, the loss of the atrial contribution to left ventricular filling reducing the pre-load of the left ventricle are all reasons for a decrease of left ventricular output and haemodynamic impairment. AF prevention includes the tight control of predisposing factors intrinsic to the patient or related to the cancer treatment itself (hypertension induced by vascular endothelial growth factor [VGEF], ischaemia induced by 5-fluorouracile), or common to the cancer condition such as electrolyte impairment or pro-arrhythmic drug use. Rhythm control may be required in seriously symptomatic patients, particularly when a rapid impairment of ventricular function occurs, requiring an urgent cardioversion. Electrical cardioversion is preferred, while anti-arrhythmic drugs may be used according to GLs only in patients without any of the multiple contraindications to these drugs, and the frequent strong pharmacologic interference of many anti-arrhythmic drug classes with cancer drugs. The same caution should be applied for long-term drug prophylaxis. In very selected cancer patients with a good oncologic prognosis and satisfying the indications of GLs, an RF ablation of pulmonary veins for rhythm control may be considered. A rate control strategy may be obtained using beta-blockers, taking into account the multiple interferences of chemotherapy with verapamil, diltiazem and digitalis.
Thromboembolic risk in AF cancer patients
Cancer commonly induces a prothrombotic condition due to the three components of the Virchow triad, blood stasis, procoagulant status, and endothelial dysfunction. Some kinds of tumours (pancreas, stomach, oesophagus, liver, breast and lung), their extension, and the metastatic condition have a higher risk. Moreover, some cancers have a high haemorrhagic risk, associated with an increased thrombotic risk. Stroke is a major and frequent thromboembolic complication in AF and in AF cancer patients but peripheral thromboembolism to the limbs or renal, intestinal, splenic and other location thromboembolism must also be remembered.
AF and stroke
Ischaemic stroke in AF patients may not infrequently be the first event of an occult cancer. Effectively it has been shown that the risk of AF development is increased in cancer patients in the first 90 days from cancer diagnosis and the risk of a new cancer diagnosis is increased in the first 90 days from an AF demonstration. Cancer incidence in stroke patients is from 4 to 8% higher than that in the general population [9].
The evaluation of the thromboembolic risk in cancer patients should follow the rules recommended by the current GLs on AF. It should be remembered that the risk scores, particularly the CHA2DS2-VASc score, although not validated in cancer, should be used to identify low-risk patients not requiring anticoagulation, while all other AF patients should undergo this prophylaxis. It should be noted that the score tends to underestimate the true risk in cancer patients who are already at high thrombotic risk. So, a patient with a score of 0 or 1 if male or of 1 or 2 if female, where anticoagulation may theoretically be delayed, often has a greater risk and, case by case, so beginning with antithrombotic therapy should also be considered with these scores.
By definition, all cancer patients have an increased haemorrhagic risk, due to some specific cancers, or due to chemotherapy inducing a low platelet level. The HAS-BLED score should not be used to establish an absolute contraindication to anticoagulation but should be used to identify particular patients who require a more in-depth monitoring and “preparation” for anticoagulation, trying to modify some conditions such as kidney function, or platelet count.
Recently, the safety and efficacy of NOACs in cancer patients have been established.
In the ENGAGE AF-TIMI 48 study, high doses of edoxaban versus warfarin showed better results independently of cancer association in terms of prevention of stroke or of peripheral embolism and major bleedings [10]. Apixaban efficacy and safety were superior to warfarin in 157 subjects with active cancer and 1,070 with cancer history enrolled in the ARISTOTLE trial [11]. Other studies have confirmed that AF subjects with cancer treated with NOACs have a lower haemorrhagic and stroke risk than those treated with warfarin [12].
It should be underlined that the thromboembolic and haemorrhagic risks vary with time.
These variations may be more rapid in cancer patients, necessitating a frequent re-assessment of the conditions. Concerning stroke patients with active cancer (who are at very high risk not only for further thromboembolic episodes due to stroke relapses, with an incidence of 7%, 13% and 16% at 1, 3 and 6 months from the first episode, but also of deep vein thrombosis [DVT], myocardial infarction and peripheral arterial thrombosis), some studies have recently been published about the efficacy and safety of rivaroxaban and apixaban for secondary prevention, showing a better profile in comparison to warfarin [11-12].
Pharmacology Interferences
Many oncologic drugs, particularly TKIs, are metabolised from CYP450 and/or by the P-glycoprotein or may inhibit or induce their function, strongly modifying the metabolism of other drugs, such as warfarin and also of many NOACs. Conversely, NOACs may interfere with oncology drugs, modifying their effects and toxicity.
The “case” of ibrutinib
This drug is the mainstay of Chronic Lymphocytic Leukaemia CLL. Anyway, also if considered with a high safety profile, ibrutinib increases the risk of AF and, at the same time, of bleeding due to a Von Willebrand defect. This is an essential factor for normal platelet function.
Therefore, during drug administration a careful cardiology surveillance with electrocardiographic monitoring is required. Generally, conduction defects occur during the first 30 days of administration and AF, ventricular arrhythmias and heart failure within 2 to 3 months. On the other hand, hypertension may occur in the first 5 months and clinical controls should be tighter during this period.
In case of invasive procedures, the drug should be withdrawn from 3-7 days before the procedure, and should be avoided in subjects requiring dual antiplatelet therapy (DAPT) or triple therapy.
In the case of manifest toxicity, generally a dose reduction or a temporary suspension is sufficient although rarely a complete withdrawal is required.
Ibrutinib may interact with many drugs metabolised by P-glycoprotein or CYP450 3A4 (calcium inhibitors, amiodarone, antibiotics, antiepileptics). Moreover, information should be given to patients about this issue and they should be advised to avoid non-steroidal anti-inflammatory drugs (NSAIDs), herbal compounds, and other auto-prescribed products considered potentially dangerous.
Due to this interaction, high plasmatic levels of dabigatran and rivaroxaban may occur, and the choice of apixaban and edoxaban may be the best. For the same reason, beta-blockers are the best choice among the drugs for rate control in AF patients in ibrutinib treatment.
In extremely selected subjects with a very high thromboembolic and haemorrhagic risk, a percutaneous device closure of the left atrial appendage may be considered.
Conclusions
|
10 essential take-home messages |
|---|
|
1. Arrhythmias may be “associated with”, “directly caused by” or “caused by therapy of” cancer. 2. There are multiple possible psychopathologic causes of arrhythmias in cancer patients. 3. The real incidence and prevalence of arrhythmias in cancer patients is probably underestimated for multiple reasons. 4. Arrhythmias contribute to a deterioration of the clinical picture of cancer patients, inducing heart failure, symptoms, reduction of functional capacity and quality of life. 5. A generally simple measure to reduce the arrhythmic risk in cancer patients is the correction of preventable arrhythmic risk factors. 6. Many cancer drugs and radiotherapy may induce bradyarrhythmias or tachyarrhythmias either through direct myocardial damage or through modification of the electrophysiologic characteristics of myocardial cells. 7. A tight clinical and electrocardiographic monitoring is indicated before and during the administration of drugs which may induce arrhythmias. 8. AF is the commonest arrhythmia in cancer patients and should be researched in depth in patients at risk with periodic screening. 9. In AF patients with cancer, the thromboembolic risk is enhanced due to the prothrombotic condition of the cancer itself and the haemorrhagic risk is also intrinsically enhanced. 10. NOACs have recently shown the best safety and efficacy profile for thromboembolic prevention in cancer patients, but they should be considered with particular attention to possible interference with oncologic drugs. |