Keywords: atrial fibrillation, comorbidities and anticoagulants, arrhythmias
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia and its prevalence increases with age reaching more than 8% in people aged ≥80 years [1]. Advancing age is associated with multiple comorbidities, increases both thromboembolic and bleeding risk and poses several challenges to antithrombotic therapy.
Trials often exclude sick and elderly patients with multiple comorbid conditions, hence limiting their generalisation to this patient group in real-world practice. There is no “one size fits all” approach and prevention of cardioembolic complications in the very elderly population needs to be balanced carefully, taking into consideration several factors.
Challenges to therapy
Very elderly patients have numerous comorbidities that increase the risk of thromboembolism and/or bleeding. These include cognitive impairment, frailty and falls, low body weight, impaired renal and liver function, intercurrent illnesses, cancer, polypharmacy, and changes in body composition that interfere with drugs pharmacokinetics and pharmacodynamics.
Elderly patients with AF have higher comorbidities and survival is worse in the presence of multiple comorbidities [2]. It has been found that the presence of four or more comorbidities in AF patients increases mortality by as much as sixfold compared to patients with AF with no comorbidities [3]. Cognitive impairment and frailty are also associated with worse outcomes. Hence the choice of anticoagulants in patients with multiple comorbid conditions is complex, and balancing the risk and benefit of different antithrombotic strategies is important [4].
Evaluation of bleeding risk
Bleeding risk should be systematically assessed using the HAS-BLED score and has shown a better prediction than an approach based only on modifiable bleeding risk factors [5]. Other bleeding risk scores have been proposed such as the ORBIT or ABC score.
Modifiable bleeding risk factors include hypertension, labile international normalise ratio (INR), medication predisposing to bleeding such as antiplatelets and non-steroidal anti-inflammatory drugs, and excess alcohol (≥8 drinks/week). Potentially modifiable bleeding risk factors include anaemia, impaired renal or liver function, and reduced platelet count or function [6].
A high bleeding risk score should not result in withholding anticoagulation as stroke risk tracks along with bleeding risk. It is important to correct modifiable risk factors in order to minimise the risk of bleeding while on anticoagulation [5, 6].
Impact of bleeding risk
The rate of bleeding in very elderly patients is higher [7, 8], with three sites of major bleeding identified - gastrointestinal, intracerebral and others [7].
Older people with AF do well with oral anticoagulation compared to no therapy and do better with novel oral anticoagulants (NOACs). Due to the higher baseline risk profile in very elderly patients, there was greater absolute risk reduction with anticoagulation than in younger patients with a number needed to treat for one year of 50 [7].
In the BAFTA trial, the occurrence of major bleeding complications including intracranial haemorrhage was similar between warfarin (INR 2-3) and aspirin in the older population. However, there are varying opinions regarding target INR with warfarin therapy in the very elderly population. While a few studies have recommended a target INR of 2-3 in very elderly or extremely elderly patients as there was positive net clinical benefit [9], other studies state that target INR should be 1.5-2 in very elderly patients at increased risk of bleeding [10]. Even amongst patients >90 years, oral anticoagulants were found to be superior to no therapy [11].
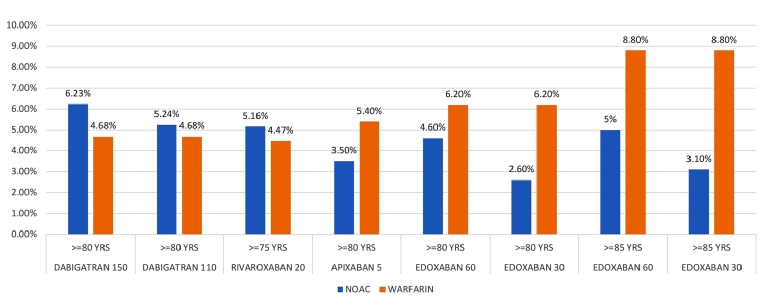
Trials of NOACs included over 27,000 older people aged >75 years. Within each trial, the absolute rates of stroke or systemic embolic events for patients aged ≥75 years were lower with NOAC regimens except for the lower-dose edoxaban regimen [12].
Individual trials show heterogeneity in terms of interaction between age and bleeding outcomes [5]. There is a significant interaction between age and increased extracranial major bleeding with both doses of dabigatran. No significant age interaction on rates of extracranial major bleeding was seen with apixaban, edoxaban or rivaroxaban [5]. The absolute rates of major bleeding were also lower with apixaban and edoxaban, but not with dabigatran or rivaroxaban [12]. In patients at high bleeding risk (HAS-BLED ≥3) apixaban and edoxaban will be safer to use.
Figure 1. Incidence of major bleeds in NOAC vs. warfarin [12].
All the NOACs evaluated together have a slightly increased risk of gastrointestinal (GI) bleeding with significant heterogeneity of effect. Factors associated with GI bleeding were anaemia at baseline, a history of GI bleeding, long-term aspirin use, increasing age and decreasing creatinine clearance [13]. Apixaban has similar rates of GI bleed to warfarin and is unique in this respect, hence it is preferred in patients with previous GI bleed.
Factors contributing to recurrent intracranial haemorrhage (ICH) include increasing age, concomitant use of aspirin or non-steroidal anti-inflammatory drugs, uncontrolled hypertension, spontaneous ICH, lobar bleed and cerebral amyloid angiopathy. Patients with lobar haemorrhage, microbleeds or cerebral amyloid angiopathy remain at higher risk for anticoagulant-related ICH recurrence than thromboembolic events and may be best managed without anticoagulants. Patients with deep hemispheric ICH and a baseline risk of ischaemic stroke >6.5% per year, which corresponds to a CHA2DS2-VASc score >5, may have a net benefit from restarting anticoagulation with a time from stroke to resumption of anticoagulation therapy of about 8-10 weeks [14].
Evaluation of comorbidities
Extrapolating trial data to real-world patients with multiple comorbidities is difficult as these high-risk patients have not been well represented in studies. High-risk patients with multiple comorbidities can account for up to 50% of patients with newly diagnosed AF.
The CHA2DS2-VASC score extends stroke prognostication in AF by including common stroke predictors additional to the older CHADS2 score (age 65-74, vascular disease, and female sex). The CHA2DS2-VASc score particularly improves the risk prediction in many patients deemed “low risk” based on the CHADS2 schema. The CHA2DS2-VASc tool has been validated in multiple independent populations and is now recommended by the European guidelines [14].
A post hoc subgroup analysis of the ARISTOTLE trial found that rates of stroke/systemic embolism, death and major bleeding increased with multimorbidity, but with no interaction in relation to the efficacy or safety of apixaban [15].
Renal disease
Patients with AF and chronic kidney disease (CKD) have increased morbidity and mortality due to their excessive risk for both thromboembolic and severe bleeding events, making risk stratification and treatment challenging. All four NOACs are at least partly eliminated by the kidneys. Dabigatran has the highest renal elimination (80%), whereas 50%, 35%, and 27% of edoxaban, rivaroxaban, and apixaban, respectively, are cleared via the kidneys.
In patients on NOACs, renal function needs to be monitored at least yearly in order to detect changes in renal function and adapt the dose accordingly. If renal function is impaired (i.e., CrCI <60 ml/min), a more frequent evaluation is recommended. The number of months after which follow up should be done can be attained by dividing the patients Creatinine clearance by 10. In patients with additional risk factors (e.g., older age, frail, multiple comorbidities, intercurrent acute illness such as infections, acute heart failure, etc.), it may be evaluated even more frequently, especially if on dabigatran.
Table 1. Renal dose modification of NOACs. Published with permission from [5]
| Creatinine clearance | Dabigatran | Rivaroxaban | Apixaban | Edoxaban |
| >50 | 150 mg twice daily | 20 mg once daily | 5/2.5 mg twice daily* | 60 mg once daily |
| 30-49 | 110 mg twice daily | 15 mg once daily | 5/2.5 mg twice daily* | 30 mg once daily |
| 15-29 | Not recommended | 15 mg once daily | 5/2.5 mg twice daily* | 30 mg once daily |
| <15 | Not recommended | Not recommended | Not recommended | Not recommended |
*2.5 mg twice daily if 2 out of 3 criteria age >80, weight <60 kg, Cr >1.5.
For patients with CrCl <15 ml/min or on haemodialysis, adjusted dose warfarin INR 2-3 may be used. Patients with severe CKD spend less time in therapeutic range or there is a higher chance of over-anticoagulation (INR >4) and require lower warfarin dosing.
Hepatic disease
Patients with significant active liver disease including cirrhosis, or those with persistent elevation of alanine transaminase or aspartate transaminase >2-3 times normal or total bilirubin >1.5 times normal were excluded from the landmark NOAC trials in AF. All four NOACs are contraindicated in patients with hepatic disease associated with coagulopathy and clinically relevant bleeding risk including Child-Turcotte-Pugh C cirrhosis. Rivaroxaban should not be used in Child B liver cirrhosis due to a more than twofold increase in drug exposure in these patients. Dabigatran, apixaban and edoxaban may be used with caution in patients with Child B cirrhosis.
Coronary artery disease
Similar to AF, the incidence of coronary artery disease (CAD) increases with ageing. Approximately 15% of AF patients have a history of myocardial infarction; 5-15% of AF patients will require stenting at some point in their life.
Co-prescription of oral anticoagulants (OAC) with antiplatelet therapy, particularly triple therapy, increases absolute risk of major haemorrhage. The addition of NOACs increases bleeding risk by 79-134%, while reducing recurrent ischaemic events only marginally in patients with AF. OAC monotherapy is recommended in AF patients with stable CAD but without an acute coronary syndrome (ACS) and/or coronary intervention in the previous 12 months. In patients treated for ACS, and receiving a coronary stent, short-term triple combination therapy of OAC, clopidogrel, and aspirin seems warranted [5].
Frailty and falls
Frailty develops as a consequence of age-related decline in multiple physiological systems, which collectively results in a vulnerability to sudden health status changes triggered by relatively minor stressor events. It is estimated that a quarter to a half of people over 85 years are frail; these people have a significantly increased risk of falls, disability, long-term care and death [16].
Increased risk of falls leading to subdural haemorrhage is a common reason for withholding oral anticoagulant therapy in very elderly frail patients. Risk of falls can be assessed prior to initiation of OAC therapy using several tools such as the “Get up and go test”, activities of daily living, and the Identification of Seniors at Risk score [17].
A Markov decision analytic model demonstrated that a patient on vitamin K antagonists (VKA) has to fall 295 times for the risk of subdural haematoma to outweigh the benefit of anticoagulation. As the risk of intracranial bleeds is even lower with NOACs, the number needed to fall would be even higher in the case of NOACs.
The risk of falls was specifically analysed in the ENGAGE-AF TIMI 48 and ARISTOTLE trials. It was found that treatment effect of the NOAC concerned was consistent even in patients at increased risk of falls. Due to a large absolute risk of events in patients at increased risk of falls, there was a large absolute risk reduction and low number needed to treat for NOACs. This benefit has been best demonstrated for apixaban and edoxaban in this patient subgroup. Also, patients with falls should be referred to fall services for management of falls [5].
NOACs reduced the risk of intracranial bleeding by 15% but lack of an easily available antidote in major bleeding due to a fall remains a drawback. Hence, anticoagulation should only be withheld from patients with severe uncontrolled falls (e.g., epilepsy or advanced multisystem atrophy with backwards falls, or in selected patients with dementia) where compliance and adherence cannot be ensured by a caregiver [6].
Low body weight
Low body weight is part of frailty syndrome, associated with cancer and renal insufficiency, and increases bleeding risk by increasing drug exposure.
Body weight ≤60 kg is a dose reduction criterion for both apixaban (if also age ≥80 yrs/creatinine ≥1.5 mg/dl) and edoxaban. Dabigatran has the same efficacy in patients with body weight <50 kg but body mass index (BMI) <23.9 can be an independent predictor of bleeding events and may be less preferable due to frequently co-existing renal insufficiency. No outcome data are available for rivaroxaban in patients with weight <60 kg or <50 kg with no recommendations regarding dose change.
VKA therapy can also lead to increased bleeding in underweight patients; patients with body weight <50 kg are underrepresented in outcome studies involving NOACs.
Dementia
The ACTIVE investigators found that a mini-mental state examination (MMSE) score <26 was associated with higher vascular events and bleeding risk. Stroke in a patient with dementia further increases the risk of cognitive and functional decline. AF is a risk factor for dementia; the use of OAC may reduce the risk of dementia in AF patients [5].
Patients with dementia spend less time in therapeutic range with warfarin therapy. NOACs may be a favourable option in very elderly individuals with cognitive dysfunction due to fixed daily dosing, no need for anticoagulation monitoring and steady pharmacokinetics. However, ensuring patient adherence is important as these drugs have a shorter half-life and missing several doses may lead to loss of protective effect. Rivaroxaban and edoxaban may offer some benefit in this regard due to once daily dosing compared to dabigatran and apixaban [17].
Cancer
The incidence of cancers increases with age as does AF. Active malignancy was usually an exclusion criterion in NOAC trials on AF and suggestions are mostly derived from trials on deep vein thrombosis (DVT). In patients with malignancy who are already on NOAC therapy for AF, the possibility of drug-drug interactions should be kept in mind. For patients who require to be initiated on anticoagulation, it is preferable to start with heparin or warfarin rather than NOACs due to greater clinical experience. Temporary cessation or dose reduction of NOACs is advised in case of myelosuppression. Frequent monitoring of complete blood counts, renal and liver function tests is advised as well as careful monitoring of signs of bleeding such as petechiae, purpura or ecchymosis [18].
Polypharmacy
The term polypharmacy means increased use of prescription and non-prescription drugs. More than half of the patients in the ROCKET-AF study and Danish anticoagulation clinic were on five or more prescription drugs. Concomitant use of >10 medications has been shown to increase the risk of major and minor bleeding. In ROCKET-AF and ARISTOTLE, patients concomitantly taking several (>5 or >9) medications experienced similar outcomes and consistent treatment effects of either NOAC relative to warfarin.
Warfarin has numerous drug interactions and a narrow therapeutic window which makes it difficult to use in very elderly individuals on polypharmacy. NOACs are easier to use in the setting of polypharmacy due to more favourable pharmacodynamics [17].
Certain groups of drugs must be avoided, particularly in case of renal impairment. In general, NOAC use is not recommended in combination with drugs that are strong inhibitors of both CYP3A4 and P-gp (e.g., verapamil, dronedarone, amiodarone, and quinidine). Conversely, strong inducers of P-gp and/or CYP3A4 (such as rifampicin, carbamazepine, etc.) will markedly reduce NOAC plasma levels; such combinations should be avoided or used with great caution. Non-metabolic clearance of apixaban is diverse (including excretion of the unchanged compound by >50%), which reduces the potential for drug interaction. Colour coding for drug interaction as per current guidelines should be followed [5].
Conclusions
Atrial fibrillation is the most common cardiac arrhythmia and its prevalence increases with age reaching more than 8% in people aged ≥80 years. Very elderly patients have numerous comorbidities that increase the risk of thromboembolism and/or bleeding and mortality.
Very elderly people with AF do better with anticoagulation than no anticoagulation at all. Antiplatelet therapy increases bleeding risk, especially dual antiplatelet therapy with bleeding rates that are similar to those on OAC. Thus, antiplatelet therapy cannot be recommended for stroke prevention in AF patients.
Warfarin has been used safely in very elderly and extremely elderly people although opinions differ about optimal target INR and the protective effect depends on time in therapeutic range.
Meta-analyses of NOAC trial data have shown no interaction between age and their safety and efficacy although the very elderly patient subgroup is under-represented in the trials. Intracranial bleeding is lower with all NOACs compared with VKA. There is a significant interaction between age and increased extracranial major bleeding with both doses of dabigatran. No significant age interaction on rates of extracranial major bleeding was seen with apixaban, edoxaban or rivaroxaban. The absolute rates of major bleeding were lower with apixaban and edoxaban. All NOACs pooled together have higher GI bleeding compared to warfarin but apixaban is unique as it has similar rates of GI bleeding.
There is a high prevalence of renal insufficiency in older patients with frequent acute decrease in renal function. Renal function should be evaluated before prescribing and monitored more frequently during therapy and during intercurrent illness to avoid the risk of bleeding. Renal clearance is highest for dabigatran and least for apixaban. Renal dose modification of all NOACs is to be followed. For CrCl <15 or on haemodialysis, warfarin is preferred but the risk of bleeding and over-anticoagulation is high.
All four NOACs are contraindicated in patients with hepatic disease associated with coagulopathy and clinically relevant bleeding risk including stage C cirrhosis. Dabigatran, apixaban and edoxaban may be used with caution in patients with Child B cirrhosis.
Rates of stroke/systemic embolism, death and major bleeding increased with multimorbidity, but with no interaction in relation to the efficacy or safety of apixaban.
In frail patients at increased risk of falls there was a large absolute risk reduction and low number needed to treat for NOACs. This benefit has been best demonstrated for apixaban and edoxaban. Patients with dementia spend less time in therapeutic range with warfarin therapy. Rivaroxaban and edoxaban may offer some benefit with regard to compliance due to once daily dosing compared to dabigatran and apixaban.
Body weight ≤60 kg is a dose reduction criterion for both apixaban (if age ≥80 yrs/creatinine ≥1.5 mg/dl) and edoxaban. BMI <23.9 can be an independent predictor of bleeding events and dabigatran may be less preferable due to renal insufficiency. There are no recommendations regarding dose change for rivaroxaban in these patients. VKA therapy can lead to increased bleeding in underweight patients.
NOACs are easier to use in polypharmacy compared to warfarin but colour coding for dose modifications in the guidelines should be followed.
Apixaban was rated FORTA-A (highly beneficial) for the treatment of AF in older people; other NOACs (including low-/high-intensity dabigatran and high-intensity edoxaban) and warfarin were assigned to FORTA-B (beneficial) [19].
An individualised approach matching the particular NOAC to the participant profile, taking into consideration the risk of bleeding and other comorbidities, should be taken rather than a generalised "one drug fits all" approach in elderly adults. Caution should still be exercised with NOACs in very elderly adults with other comorbidities (mainly renal impairment) and very low body weight. Lack of a reversal agent for the anticoagulant effects of NOAC should also be kept in mind when prescribing these agents.















