Abbreviations
ATP antitachycardia pacing
CHD coronary heart disease
CMR cardiac magnetic resonance
CRT cardiac resynchronisation therapy
EGM electrogram
ICD implantable cardioverter defibrillator
LGE late gadolinium enhancement
LVEF left ventricular ejection fraction
PVS programmed ventricular stimulation
SCD sudden cardiac death
S-ICD subcutaneous ICD
SVT supraventricular tachycardia
VF ventricular fibrillation
VT ventricular tachycardia
Introduction
In 1980, Dr Michel Mirowski and colleagues implanted the first defibrillator in a woman who survived a cardiac arrest after myocardial infarction. After that pioneering intervention at Johns Hopkins Hospital, technology has evolved. Nowadays, implantable cardioverter defibrillators (ICDs) are routine practice for primary and secondary prevention of sudden death in selected patients with heart disease.
Notwithstanding a reduction in the general cardiovascular disease mortality in recent decades, the global burden of sudden cardiac death (SCD) has not greatly diminished [1]. The reason for this paradox is partially explained by the general ageing of the population, as the elderly have a higher risk of SCD. Despite an 80% prevalence of severe coronary heart disease (CHD) underlying SCD, the majority of cases occur in patients with unknown heart disease, who do not have a current indication for an ICD [1].
Furthermore, sudden deaths can also result from bradyarrhythmias, electromechanical dissociation and ventricular arrhythmias that are refractory to ICD-delivered therapy [2]. While many bradyarrhythmias can be efficaciously treated by common ICDs, which can be programmed with backup pacing function, the other conditions are difficult to treat even in the emergency care ward. They are often the result of a severe structural heart disease (e.g., end-stage heart failure) or comorbidities that render most resuscitation attempts ineffective.
ICD engineering has developed at a fast pace to counteract these limits (e.g., cardiac resynchronisation therapy [CRT] to improve systolic function in severe heart failure, ICDs with bicameral pacing function to prevent the pacemaker syndrome, telemetry for the early recognition of arrhythmias and device malfunctions); however, further developments are required.
About sixty percent (60%) of ICDs are implanted for primary prevention, the remaining for secondary prevention [2]. The management of patients largely depends on age, comorbidities and reason for implantation (primary vs. secondary prevention).
ICD for primary prevention
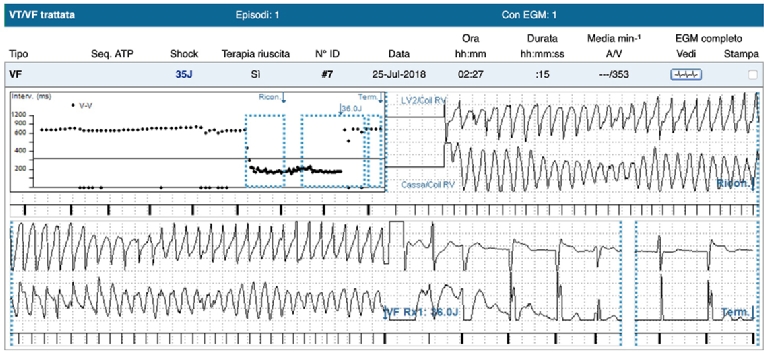
Current guidelines give a class I recommendation for ICD implantation in patients with either ischaemic or non-ischaemic cardiomyopathy with severely depressed systolic function (left ventricular ejection fraction [LVEF] ≤35% for New York Heart Association [NYHA] Class II or III, ≤30% for NYHA Class I symptoms). At five years from implantation, about 37% of primary prevention patients will have an appropriate device intervention (antitachycardia pacing or shock), against 51% of patients implanted for secondary prevention [2]. Frequent episodes of ICD appropriate therapy warrant a clinical reassessment, as it has been demonstrated that ICD shocks correlate with increased risk of heart failure hospitalisation and mortality [2]. The clinical cardiologist should therefore identify potentially reversible causes of ventricular arrhythmias (e.g., myocardial ischaemia, electrolyte imbalances, etc.) and treat them, whenever possible. Figure 1 shows an appropriate ICD shock.
Figure 1. A ventricular fibrillation is correctly classified by the ICD, which delivers a 35 J shock with restoration of sinus rhythm.
Nowadays, the sole parameter to decide on ICD implantation for primary prevention in heart failure is LVEF, even if the incidence of ICD appropriate shocks is relatively low. It is also true that only a minority of people who experience SCD have an LVEF ≤35%.
Moreover, the benefit of ICDs on all-cause mortality may be less evident in the modern era, due to the general ageing of the population and more widespread use of optimal medical therapy for heart failure and CRT, as shown by the DANISH trial [3]. In this context, clinical research should focus on the identification of clinical predictors of ventricular arrhythmias that are complementary to LVEF measurement. This finding, if cost-effective, could be particularly useful in the areas of the world where there is limited access to ICD technology, or when the decision for ICD implantation is doubtful because of perceived detrimental effects on quality of life, risks of infection, etc.
In the past, attempts to stratify patients better according to their arrhythmic risk have been performed, especially in ischaemic patients (e.g., heart rate variability analysis, programmed ventricular stimulation (PVS) to induce arrhythmias in the electrophysiology laboratory), but none of these methods has translated into effective clinical use.
Recently, there has been an increase of interest in cardiac magnetic resonance (CMR) for the prediction of ventricular arrhythmias [4]. It is well known that the presence of late gadolinium enhancement (LGE) indicates myocardial scar, which is a potential arrhythmogenic substrate, and has a negative prognostic value. The presence and extent of LGE has been found to correlate with the incidence of ventricular arrhythmias and appropriate ICD shocks in both ischaemic and non-ischaemic dilated cardiomyopathy patients [4]. Further studies will clarify the potential role of CMR imaging in stratifying the arrhythmic risk of patients with heart failure or with normal/near normal cardiac function.
Congenital heart diseases
Congenital heart diseases associated with the risk of sudden death also have an indication for ICD implantation, especially in the presence of symptoms suggestive of ventricular arrhythmias and family history of sudden cardiac death. Among them, an ICD is recommended for patients with Brugada syndrome with type 1 electrocardiogram (ECG) pattern, arrhythmogenic right ventricular cardiomyopathy, short and long QT syndromes, cardiomyopathies including hypertrophic cardiomyopathy and left ventricular non-compaction. In a recent survey of 252 patients with Brugada syndrome and an ICD implanted for primary prevention, about 77% received an appropriate ICD shock within five years of implant [5]. Risk factors for shock delivery were syncope and spontaneous type 1 Brugada ECG [5].
Given that out-of-hospital cardiac arrest in the young is not so infrequent (3.7 per 100,000 in children, 6.3 per 100,000 in adolescents) [6], with the majority of cases being attributable to arrhythmias, there is a clear need to improve the existing screening programmes to identify congenital heart diseases before symptoms develop. As SCD can be the first manifestation of a syndrome, there is a need to identify clinical predictors of the risk of SCD (e.g., genetics, electrophysiology study) to decide on ICD implantation. In Brugada syndrome patients, PVS for the induction of ventricular fibrillation (VF) may be a useful test to evaluate the risk for SCD.
Most common conditions causing inappropriate ICD therapies
Inappropriate shocks occur in a relatively high percentage of patients with an ICD. It is estimated that, in five years, 17% of patients will have one or more inappropriate ICD shocks, which is one of the major limits of ICDs [2]. Apart from reduction in quality of life and psychological distress, inappropriate ICD therapies may trigger lethal arrhythmias. It has been demonstrated that a careful device programming with the aim of reducing the risk of inappropriate therapy lowers mortality in ICD patients [7]. Table 1 summarises the most common causes of inappropriate ICD therapies and current management strategies to solve them.
Table 1. Most common conditions causing inappropriate ICD therapies.
| Problem | Manifestation | Management |
|---|---|---|
| Supraventricular arrhythmias, sinus tachycardia, atrial fibrillation or flutter with ventricular frequency in the VT or VF zone. | Inappropriate therapy (ATP or shocks). | Dual-zone therapy programming for VT and VF (e.g., programming VT only monitor or ATP for rates >180 and <200 bpm and shock for rates in the VF zone), increasing detection delays and cut-off rates. Programming parameters strongly depend on the indication for ICD, with lower cut-off rates and delays for therapy usually most indicated for secondary prevention. |
| Sensing defects due to T-wave oversensing, QRS double counting, myopotentials, lead fractures, electromagnetic interference. | Inappropriate therapy, therapy failure. Myopotentials may cause inappropriate sensing both in older unipolar leads and in bipolar leads with insulation breaches. | Check for sensing, impedances, pacing thresholds. Radioscopy if suspected lead fracture or insulation breach. In case of confirmed lead failure, discuss treatment strategy with patient (lead removal and substitution or addition of a new lead and abandonment of the damaged lead). Strict follow-up of leads having recalls, for example St. Jude Medical's Riata family of leads (which were prone to insulation breaches) and Medtronic's Fidelis, which was prone to conductor fractures. |
| Non-sustained ventricular tachycardia. | Inappropriate therapy (ATP or shocks). | Increase detection rates and detection delays (e.g., up to 60 seconds for primary prevention patients for rates <180 bpm, up to 15 seconds for secondary prevention patients). Longer detection delays will allow self-termination of non-sustained ventricular arrhythmias without painful shocks. |
ATP: antitachycardia pacing; VF: ventricular fibrillation; VT: ventricular tachycardia
Despite careful evaluation by regulatory agencies, lead malfunctioning caused by fracture of the conductor, insulator breaches, or defects in lead connection to the device is a principal cause of inappropriate delivery of shocks [7,8]. Failure occurs in approximately 0.29-0.45% of leads per year, with more than double the risk for recalled leads such as RiataTM (St. Jude Medical, St. Paul, MN, USA) and Fidelis (Medtronic, Minneapolis, MN, USA) [9]. Other problems connected with current leads are dislodgements (estimated at 1.4% at one year post implant) and ventricular perforation (0.8% at one year), which often require reintervention [10].
It is of great importance for future engineering of devices to find new materials and/or structural design to improve lead performances and reduce the current rates of failure. Other advances in lead fixation will help to prevent dislodgements or ventricular perforation: the first is more frequent with passive fixation leads, the second with screw leads. Other necessary advances in technology concern device programming: more sophisticated algorithms for oversensing exclusion and discrimination of supraventricular tachycardia (SVT) from ventricular tachycardia (VT) may considerably reduce the number of inappropriate shocks.
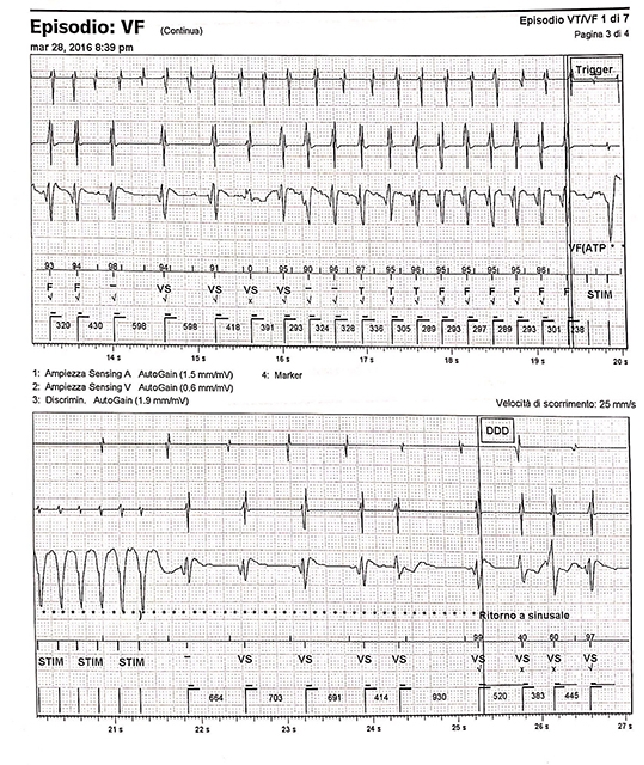
Figure 2 shows an example of inappropriate ICD therapy.
Figure 2. A dual chamber ICD delivers inappropriate therapy (antitachycardia pacing [ATP]) for atrial fibrillation with fast ventricular response that falls in the VF high-frequency zone. SVT/VF discriminators have failed.
Remote monitoring
Device manufacturers have developed remote monitoring systems for online transmission of data regarding the ICD functioning, including lead malfunctions (e.g., abrupt increase in impedances and pacing thresholds), battery end of life and appropriate/inappropriate therapy.
Real-time transmission of alerts on rhythm and technical parameters allows the clinician to make an early diagnosis and to treat most problems of ICDs, with significant reduction in mortality as shown by the IN-TIME trial, which compared remote monitoring with traditional ambulatory monitoring in Biotronik device-implanted patients [11].
Another advantage of telemetry is the possibility of monitoring parameters connected with worsening of heart failure, such as heart rate and measures of thoracic congestion (OptiVolTM index; Medtronic). Early identification of patients at increased risk for hospital admission for heart failure may prompt an ambulatory visit for reassessment of therapy.
As patients with an ICD often have ischaemic cardiomyopathy, St. Jude Medical has developed a continuous ST-monitoring function via intracardiac electrograms (EGMs). The results of a prospective study showed a high negative predictive value for ischaemia when using this algorithm, with many asymptomatic patients correctly identified as having myocardial ischaemia after perfusion imaging tests [12].
Some pacemakers have algorithms that calculate amplitude and period of respiratory cycles on the basis of changes in thoracic impedances; they have been designed for sleep apnoea monitoring. This type of sensor has allowed clinicians to correlate the sleep apnoea burden with the risk of atrial fibrillation [13]. It is desirable that the same technology should be applied to ICD engineering.
Given the complexity of heart disease and comorbidities in the majority of patients living with an ICD, it seems appropriate that future devices are capable of remote transmission of multiparameter data, together with a risk score of clinically significant endpoints (e.g., hospitalisation, arrhythmias, death) to render a clinical reassessment more rapid when it is needed. A further example of how useful the daily remote transmission of ICD-collected data can be has been shown by Shakibfar and colleagues: machine learning algorithms based on data such as percentage of ventricular pacing and daytime activity were capable of predicting electrical storms, which are three or more episodes of sustained VT or VF occurring in 24 hours which constitute a medical emergency [14].
Future cardiologists are required to become acquainted with online platforms for the follow-up of patients with ICDs; these are going to be implemented by all manufacturers. Paralleling the development of this network, engineers have to face the low but possible menace of cybersecurity breaches. Even though no cases have been reported up till now, it seems possible that hackers could interrupt the communication between the device and the remote server, with potentially dangerous clinical consequences [15]. For this reason, St. Jude Medical has developed firmware upgrades to include protection against hacking [15].
Device infections
Microbial colonisations involving the leads pose a high risk for endocarditis and sepsis. The majority of these episodes are encountered in patients with comorbidities and who are immunocompromised. These conditions increase the risk for life-threatening infections, which occur in about 1.2% of implanted patients and require long-term antibiotic therapy [16]. Device infections can occur even years after implantation, as a result of sepsis and colonisation by microbial agents [7]. In recent years, subcutaneous ICDs (S-ICDs), which are lacking transvenous leads, have been associated with a better safety profile than conventional ICDs in terms of sepsis and endocarditis [17]. In future, randomised clinical trials evaluating S-ICDs in patients at high risk of infection, or with a previous conventional ICD explanted because of infection, will clarify the utility of this new generation of devices in this subset of patients.
The use of an absorbable antibacterial envelope (TYRXTM; Medtronic) during implantation of conventional ICDs and pacemakers has shown promise in reducing the rate of electronic device infections. However, the envelope does not provide protection for transvenous leads, which are the most dangerous site of microbial colonisation, and costs, which are high (about 1,000€ per unit), limit its use to patients at high risk. For these reasons, device infections remain an issue.
Subcutaneous ICD
The most vulnerable element of the ICD is the lead, which can be damaged or constitute a source of infection [7,8]. The metallic coil itself facilitates the formation of adhesions within the vasculature, which may render extraction more difficult when it is necessary. Nowadays, both mechanical and laser methods for lead extraction have been developed.
According to the ELECTRa registry of transvenous lead extraction outcomes of the European Heart Rhythm Association (EHRA), complication rates (major complications requiring surgery or resulting in death) vary between 2% and 4%, depending on the centre’s experience. However, there are few centres that have the appropriate training to perform lead removal, which is a challenging procedure in most instances. Transvenous leads also carry the risk of subclavian vein stenosis (26% of cases) or occlusion (9%), which render more difficult not only the eventual lead extraction but also reimplantation [7].
To overcome the many limits of transvenous leads, in recent years there have been attempts to produce devices without transvenous elements.
In a clinical scenario in which leads have been removed, it remains possible to implant a subcutaneous ICD (S-ICD) [17]. The EMBLEMTM MRI S-ICD System is the latest device produced by Boston Scientific (Marlborough, MA, USA), which today is the sole manufacturer commercialising S-ICDs approved for patients. The device is MR conditional and it is entirely subcutaneous, with a subcutaneous lead positioned vertically in the precordial position. Apart from lacking a transvenous system, which renders it more suitable for patients with a history of infection and for the young, being a less invasive device, it is larger than the conventional ICD generator to ensure transthoracic shocks of 80 J (conventional ICDs produce shocks of about 35 J) and the duration of battery is usually shorter (about seven years). Technical characteristics have improved from the first-generation models. Remote transmission of data is also possible.
The principal limit of S-ICDs is the lack of permanent pacing function, a characteristic that is present in conventional ICDs [17]. For this reason, the choice of implanting an S-ICD should be carefully balanced against the risk of developing a bradyarrhythmia requiring pacing. Younger patients have a lower likelihood of developing the need for permanent pacing and are usually the best candidates for S-ICD implantation. Eligibility assessment with basal and exercise stress ECG pre-implant is recommended to avoid potential T-wave oversensing [17] and consequent inappropriate therapy, which is a problem in a relatively high percentage of patients, especially in those with Brugada syndrome and prominent T-wave alterations. The manufacturer has developed a new algorithm (SMART Pass) that seems effective in reducing oversensing, but further real-world experience with these devices is required.
Previous studies such as IDE and EFFORTLESS have launched the S-ICD in clinical practice, showing an efficacy comparable to ICDs [17]. The PRAETORIAN study, an ongoing prospective randomised clinical trial, will directly compare the S-ICD with ICDs [17].
Wireless CRT
The most recent innovation, still in phase II clinical research, is wireless cardiac resynchronisation therapy, which could be a future option for patients who are candidates for CRT-P (pacemaker) or CRT-D (defibrillator). In detail, the SELECT-LV study evaluated the feasibility of a new-generation biventricular stimulation in a few patients (n=35) with heart failure and failed conventional CRT [18]. The left ventricular stimulation WiCS-LV system (EBR Systems Inc., Sunnyvale, CA, USA) converts ultrasound impulses produced by a subcutaneous generator into electrical stimulation synchronised to right ventricular pacing via a mini-electrode implanted in the endocardium of the left ventricle [18]. This system has also been successfully applied to a patient having a right ventricular leadless pacemaker (MicraTM; Medtronic), to produce a completely leadless biventricular pacemaker [19]. Other systems are going to be developed, for example using three leadless pacemakers (for right and left ventricles and right atrium) communicating via low voltage alternating currents (conductive intracardiac communication) [20].
Costs
Costs for ICDs vary depending on function and type of implant, with the most basic device being around 6,500€ for the generator; the highest price is 12,000€. The leads cost between 150€ (atrial lead) and 700€ (ventricular lead). Costs for CRT are even higher, up to 14,000€ for the generator. The S-ICD is the highest in price, about 18,000€. It is desirable that the increase in the number of ICDs produced to meet the growing need, together with developments in materials and fabrication methods, will lead to a reduction in prices, in order to render ICDs more accessible in all areas of the world, even in developing countries.
Furthermore, a more widespread use of remote monitoring in future may help clinicians to optimise time and resources required for ambulatory visits.
Conclusions
The invention of ICDs was a milestone in cardiology, as it allowed for the prevention of sudden arrhythmic death in many patients. However, unmet needs concerning ICDs remain. The clinical cardiologist still has to face inappropriate shocks, lead failures, device infections and electrical storms. Many of these issues can be solved or improved with the use of current technology, but nowadays ICDs are far from perfect. The knowledge of ICD management and their limits is also the basis for future engineering and the development of new-generation devices such as the S-ICD and wireless CRT.















