Keywords: ICD, follow-up, private cardiologist, device specialist
Introduction
Around 108,000 implantable cardiac defibrillators (ICDs) and 63,000 cardiac resynchronisation therapy defibrillator (CRT-D) devices were implanted in 2016 with large regional differences across European Society of Cardiology (ESC) countries to prevent sudden cardiac death (SCD) [1]. As implantation rates soar or continue at a high rate, cardiologists face the considerable burden of managing such patients in their clinics. Given that the majority of ICDs (85%) are implanted in patients suffering from heart failure with reduced left ventricular ejection fraction (HFrEF), the follow-up and care of ICD/CRT-D recipients will overlap significantly with the standard practice of heart failure management [2]. This paper will give a concise and practice-oriented overview on the periodical tasks of ICD follow-up visits, especially for patients who attend their first visit after implantation. Furthermore, we highlight the clinical scenarios which warrant cooperation with a device specialist. We are going to cover complications regarding the generator pocket, interpretation of the electrocardiogram (ECG) and echocardiography findings; moreover, we will discuss how to make the best use of the diagnostic information collected by the device in order to change antiarrhythmic or heart failure management in due time, or to introduce anticoagulation to prevent thromboembolism. Finally, we deal with particular emergency situations of ICD carriers, such as lead-associated infective endocarditis or frequent shocks heralding electrical storm or device malfunction.
First visit after an ICD or CRT-D implantation
On the first appointment following ICD implantation, baseline information should be obtained and captured in the medical record of each patient. The ICD indication should be clear, whether it was implanted for the primary or secondary prevention of SCD [3]. CRT-D patients for secondary prevention will face an almost fivefold higher frequency of ICD therapy episodes than patients implanted on a primary basis [4]. Discuss again the role of ICD with the patient and trusted relatives and make clear that the ICD is only capable of preventing SCD but cannot influence the exact progression and prognosis of the underlying heart disease, CRT-D being the only exception. Reassurance and organising psychological care, if needed, is recommended. Legislation in terms of driving restrictions is not uniform across ESC countries; for the most part, professional licences are affected.
Collect baseline information regarding the implanted system! Depending on the particular healthcare system, this information can be accessed via the electronic implant register or at least one can find it on the implant identification card or leaflet. The essential information every general cardiologist should know is not really the model or the manufacturer but the implantation date, route, the ICD system, the capability of remote monitoring, and the name of the device specialist/centre to contact.
ICD system overview
A transvenous ICD can be a single-chamber, dual-chamber or a CRT-D system. A single-chamber ICD system with the shock lead in the right ventricle (VVICD) can terminate those sustained arrhythmias that the discriminatory algorithm of the ICD generator identifies as ventricular tachycardia (VT) over a supraventricular tachycardia (SVT). It is important to bear in mind that the shock lead of a VVICD cannot collect atrial signals, thus the discrimination between a rapid supraventricular and ventricular arrhythmia is based on indirect features of the ventricular intracardiac electrogram only. VVICDs are the most frequently implanted systems in sinus rhythm without pacing indication and in patients with permanent atrial fibrillation.
Dual-chamber systems (DDICD) have an additional right atrial lead in place. Therefore, DDICDs can directly detect atrial arrhythmias, and their more sophisticated VT/SVT discriminatory algorithms can directly use the atrial electrogram to avoid inappropriate ICD therapy in case of a tachycardia falling into the programmed detection zone. Dual-chamber systems collect essential information on the duration and frequency of atrial tachyarrhythmia episodes and display the atrial fibrillation (AF) burden. A DDICD is implanted when atrial pacing is indicated.
A dedicated single-lead, dual-chamber system (VDDICD) has a single shock lead with an atrial bipolar ring electrode as the lead spans through the right atrial cavity. This ring is designed only to sense atrial activity, but not to pace the atrium. Simple configuration and reliable atrial sensing performance allowing dual-chamber discrimination are the advantages of this system.
CRT-D systems have an additional, third lead to pace the left ventricle, thus providing biventricular pacing in eligible patients suffering from HFrEF [3]. The percentage of biventricular pacing is an important parameter reflecting the efficiency of CRT. If implanted in permanent AF, when atrial sensing and pacing makes no sense, a CRT-D system has only two ventricular leads.
Subcutaneous ICDs (S-ICD) are single-lead systems designed to detect fast VTs and ventricular fibrillation (VF). Since an S-ICD system cannot deliver anti-tachycardia pacing, the only treatment option is to deliver a shock, and so they are mainly implanted for primary prevention. Importantly, there is no indwelling venous component, thus lead friction and lead-related infections are no longer an issue with this system. The generator is somewhat larger and can be found in the left mid-axillary line between the 5th and 6th intercostal spaces.
On the rare occasion when baseline information is not available at all (implantation in a foreign country or ID card lost) the number and course of the leads and the position of the generator on a biplane chest X-ray can define the type of ICD system clearly for the general cardiologist.
Audible or vibratory patient alerts are programmed for a range of reasons. Battery depletion and lead malfunction alerts are the most important ones. If the patient complains of a periodical beeping sound or vibration, it is time to refer to the specialist.
Examination of the pocket
The vast majority of ICD generators are implanted subcutaneously (or intramuscularly) in the left infraclavicular region, because this configuration secures the most effective energy delivery with the shock vector oriented through the largest mass of ventricular myocardium. In the first six postoperative months, patients are usually closely followed up by the device specialist to detect any early pocket- or lead-related complication, as this period presents the highest infection and dislodgement rates. Device infection rates are around 2%; ICD generator replacement elevates this risk [5]. Implantation of more than one lead increases the risk of infection fourfold [6]. It is important to bear in mind that an ICD pocket is a particular compartment in terms of infectiology as it harbours an artificial device which is directly connected to the heart and to the central venous circulation; therefore, specific rules apply over the routine postoperative protocol of general surgery. Decreasing postoperative pain and small suffusion around the pocket are quite common and heal within the first two to three weeks without any intervention. Only reassurance is needed to settle the concerns of patients. If growing tenderness, pain, redness, swelling, ballotable effusion, wound discharge or a draining sinus develops, referral to a device specialist even without any systemic signs or symptoms is needed, as these are the signs of pocket infection (Figure 1). Skin erosion with the generator visible is the far end of this spectrum (Figure 2). Ballotable effusions early after implantation can be non-infected haematomas or postoperative seromas, which can heal without surgical intervention, but this should always be the decision of the device specialist. Percutaneous drainage of pocket effusions is strictly discouraged in outpatient cardiology or general surgery facilities, as this manoeuvre can infect a previously sterile pocket with skin-borne microorganisms and can end up in a risky complete ICD system removal due to endocarditis [7]. Even a sterile surgical incision to evacuate the pocket performed by hands inexperienced in device management can easily damage the connector portion of the lead, resulting in noise generation and inappropriate shocks.
Figure 1. Pocket infection.
The patient presented and complained about a painful pocket and redness over the lateral edge. Note the superficial generator position. Two surgical scars provide evidence of a previous generator replacement. Courtesy of Dr. Roland Papp, Semmelweis University.

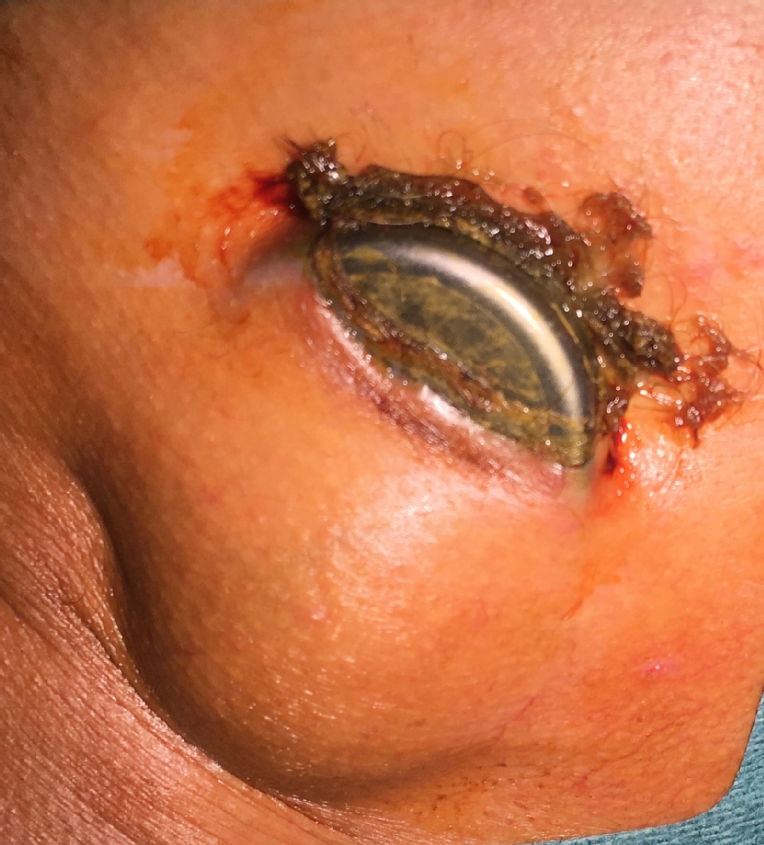
Figure 2. Eroded skin with the generator visible in the pocket.
Note the oedematous skin over the pocket. A transvenous total system explantation was carried out. Courtesy of Dr. Roland Papp, Semmelweis University.
The above-mentioned alarming signs can develop months or even years after implantation, so pocket examination should always be part of general follow-up. A thin, atrophied and slightly tender skin covering a subcutaneously placed generator implanted years before can be a common finding in elderly, cachectic patients and even a ridge caused by the underlying electrode can be seen on the skin. This is not necessarily an alarming sign of infection until local inflammatory reaction is absent and the overlying skin is movable over the generator. In this case, soft skincare and appropriate dressing avoiding friction from the seams of T-shirts should be advised. The car safety belt and strips of a backpack stretching over the area should be cushioned by a soft sponge. When the overlying skin adheres to the generator and is not freely movable anymore, refer the patient to a specialist even without any other overt signs of infection.
Pocket infections are almost exclusively bacterial: 60-80% of them are caused by staphylococci [7,8]. We strongly discourage immediate initiation of oral empirical antibiotics in an outpatient setting with a spectrum against staphylococcus aureus and coagulase-negative staphylococci before sampling blood for cultures. The recommended empirical therapy is iv. vancomycin to be started always after sampling, as methicillin-resistant strains can account for up to 50% of the cases.
Lead-related endocarditis
This type of right-sided endocarditis can develop in association with or without pocket infection even years after implantation. Lasting fever, elevated inflammatory markers, new-onset tricuspid regurgitation, bilateral patchy pneumonia of septic embolism, and a sepsis with unknown focus raise the suspicion of infective endocarditis in an ICD patient. The more leads there are in the venous system, the higher the risk of developing an endocarditis. Larger vegetations (>5 mm) can usually be seen by transthoracic echocardiography (TTE), but TTE results are frequently inconclusive. When lead involvement is suspected, transoesophageal echocardiography (TOE) is the recommended method, or positron emission tomography-computed tomography (PET-CT) can provide proof. In case of a suspected lead-related infective endocarditis, contacting a centre with an explantation facility is mandatory, because total system removal is inevitable [8]. Of note, it is important to emphasise that routine endocarditis prophylaxis of a transvenous ICD system before a dental procedure is not endorsed by guidelines [7,8].
Anticoagulation therapy post-implantation
Restarting oral anticoagulant therapy is usually safe after 24 to 48 hours if no bleeding presents and the pocket looks fine on examination. Bridging with low molecular weight heparin (LMWH) or unfractionated heparin should always be avoided as they elevate the chance of haematoma formation. Patients with a high thromboembolic risk profile, such as the ones with mechanical heart valves, should be operated on uninterrupted warfarin therapy [9].
12-lead ECG
Given that the majority of ICD patients have a sufficient heart rate, ICD generators are usually programmed to a 40 bpm back-up ventricular pacing (VVI) mode to minimise unnecessary right ventricular pacing, which can result in left ventricular dysfunction [10]. Constant, asynchronous pacing at 40 bpm with effective capture suggests pace dependency, and revision of antiarrhythmic medication or an upgrade to DDICD or CRT-D should be considered in keeping with the clinical status. This scenario is frequently seen in male HFrEF patients with a previously normal heart rate and a VVICD who start taking amiodarone. Regular pacing artefacts without effective capture with an otherwise normal heart rate reveal undersensing that is most likely caused by lead dislodgement. Referral to a device specialist is mandatory as VT/VF detection is also affected in this case. The post-implantation baseline ECG serves as a reference for possible changes in native QRS width and morphology for the future. A newly developed left bundle branch block (LBBB) in an HFrEF patient can be a clue to considering a CRT-D upgrade if other indications prevail.
Extensive ECG or ambulatory Holter monitoring to detect arrhythmias in ICD patients is unnecessary, as contemporary device memory can give all the necessary information, especially when remote device monitoring is in operation. The only exception is the search for AF episodes in VVICD carriers, since there is no lead to monitor atrial electrical activity directly.
Imaging
A slight chest pain with decreasing intensity days after implantation can be normal, but always perform a TTE, especially when the pain persists. Newly detected pericardial effusion can be a sign of lead perforation, although the tip of the lead itself is hard to visualise by ultrasound. Even if there is no sign of tamponade, refer the patient to the implanting centre, as pericardial penetration can also cause sensing/pacing failure. Tethering of the tricuspid valve by the shock lead can result in new-onset regurgitation; usually, the septal leaflet is affected. The shock lead spanning through the valve is best seen from apical 4-chamber, subcostal, and sometimes from parasternal short-axis views. If the regurgitation is graded severe, refer to a device specialist to consider repositioning. Lead-associated oscillating vegetations can also be recognised at the atrial or tricuspid level.
A postoperative chest X-ray is always performed in the implantation centre to document lead position and to rule out pneumothorax upon subclavian access. Routine X-ray follow-up is not needed in private practice. Indication for advanced imaging (TOE, CT scan, PET-CT) of the ICD system should be the task of the device specialist according to the actual clinical scenario.
The regular TTE follow-up of ICD patients should be scheduled according to their underlying cardiac condition; more frequent visits due to the ICD per se are unnecessary. Always document postoperative baseline left ventricular function to enable comparison with future scans. This is quite important in patients with >40% right ventricular pacing [10]. Improvement or even normalisation of left ventricular function can occur after CRT-D implantation, but is unlikely with a conventional ICD.
ICD-based remote monitoring
ICDs equipped with remote monitoring (telemonitoring) capability transfer daily diagnostic information to a wireless communicator interface which automatically sends encrypted signals through a landline or mobile telecommunication network to a secure server owned by the manufacturer. The database is accessible by the telemonitoring team from the implantation centre.
The system processes vast amounts of data and flags different levels of alerts based on algorithms automatically analysing different parameters. Among others, these include monitoring and trending lead and generator integrity, atrial and ventricular arrhythmia burden, ICD therapy delivery, amount of biventricular pacing, patient activity, resting heart rate, heart rate variability, and intrathoracic impedance. Trained staff overview and filter these alerts and present them to device specialists who contact the patient and modify therapy when necessary. For safety reasons, the system configuration does not allow remote programming.
The body of evidence is growing regarding the safety, utility and long-term positive impact on patient outcomes of ICDs. In case of a properly functioning ICD system, in-office interrogation visits can be scheduled less frequently in order to reduce the burden imposed on clinicians and patients. Annual in-office follow-up of a primary prevention ICD system is as safe as seeing the patient every 3 months [11]. When the information gained from remote monitoring of an ICD or CRT-D system was incorporated into a clinical response-system, earlier therapeutic decision-making and intervention (4.6 vs. 22 days) could prevent further clinical deterioration [12]. Significant reduction of all-cause mortality (3.4% vs. 8.7%; p=0.004) was observed in the telemonitored cohort over 12 months of follow-up [13]. Remote monitoring-based patient management could substantially decrease the number of appropriate and inappropriate ICD shocks by 71%, which would also result in a significant increase of battery longevity [14].
Current ESC guidelines endorse remote monitoring with a class II level A recommendation [15]. Enthusiasm generated by the randomised, controlled trials cited above was somewhat hampered by data protection and cybersecurity issues. Furthermore, everyday practice proved that delay in contacting patients after inappropriate tachycardia detection remained quite long (8 days), despite the use of remote monitoring [16]. As an outlook for the future of telemonitoring, establishing clear organisational protocols are of high importance, as well as investment in enhanced data security both on the manufacturers’ and care providers’ side.
Access to device memory
Testing the electrical integrity and longevity of the ICD system and managing system-related issues are the tasks of the device specialist. Contemporary ICDs collect data on a wide range of diagnostic parameters and they are usually equipped with remote monitoring capability. A well-organised telemonitoring framework results in improved survival [13]. Access to and use of the diagnostic memory can help the private cardiologist to recognise the subclinical manifestation of disease progression even without being a device expert. Therefore, we encourage requesting even a limited access to telemonitoring centre platforms or at least obtaining a paper or PDF printout of the parameters mentioned below. Given that a significant arrhythmia alert or impending heart failure episode alert on telemonitoring usually prompts a fast therapeutic response and patient contact, it is inevitable to set up the framework of cooperation with the implantation centre to avoid parallel actions.
Atrial fibrillation
Because the majority of ICD recipients suffer from heart failure, AF is not uncommon. As heart failure itself increases the risk of thromboembolism, early detection of asymptomatic AF episodes should usually result in initiation of anticoagulation. The atrial high rate episode (AHRE) list and the AF burden percentage are directly collected from the atrial electrode by the generator. VVICDs do not have this feature. Although the threshold for anticoagulation in terms of AF burden is still in question, even as short an episode as six minutes might increase the thromboembolic risk. An AF episode of a duration >24 hours would definitely indicate long-term anticoagulation [17].
Heart failure management
Unfortunately, no single parameter can predict impending acute heart failure, as ICDs cannot measure left ventricular filling pressure. Therefore, algorithms combining multiple indirect parameters have been developed and tested, such as number of AF and VT episodes, frequency of ventricular extrasystoles, resting heart rate, drop in daily activity, low CRT pacing, and drop in intrathoracic impedance. False positive alerts were common in the past, but contemporary algorithms are quite predictive [18]. Alerts should result in more thorough patient examination and escalation of HF therapy.
ICD shocks
On every follow-up, sensation of ICD shocks, palpitations or unexplained faints should be interpreted and explored in detail. Adherence to medical therapy should also be explored. Referral to a device specialist is recommended to judge the appropriateness of ICD therapy, unless the patient has already been contacted via the remote monitoring service. Unexplained faints are frequently caused by haemodynamically not tolerated fast VT or VF episodes with too long detection intervals. In this case, patients do not remember the terminating shock.
Multiple shocks, electrical storm
When a patient experiences multiple shocks/faints, thorough care must be taken, and the situation must always be handled as an emergency with immediate referral and transfer to a device specialist with an intensive care background. If the shocks are appropriate and occur three or more times in 24 hours, we call it an electrical storm. This can be the harbinger of fast progression of the underlying disease in heart failure patients. If left untreated, it could result in exhaustion of or resistance to ICD therapy, and finally would lead rapidly to a circulatory arrest. It is important to know that the number of shocks are universally maximised at around six attempts in a single VT/VF episode by device configuration.
Inappropriate shocks
The incidence of inappropriate shock is around 15%. Misinterpretation of fast atrial tachyarrhythmias is the commonest cause at 75%, but noise detection due to lead insulation damage, T-wave oversensing, and electromagnetic interference of various sources can also play a role. DDICDs with contemporary programming outperform VVICDs in VT/SVT discrimination, leading to fewer inappropriate shocks (8 vs. 24%) [19]. A history of AF can raise suspicion of inappropriate ICD discharge, although, the VF-triggering effect of the irregular RR intervals can manifest as a “dual tachycardia” on interrogation. The older the shock lead, the more prone to insulation damage, which is especially true for young, physically active patients with implantation via subclavian access (subclavian crush).
Multiple inappropriate shocks are just as important to handle as an emergency to prevent total battery depletion and to minimise their psychological burden, and also to avoid the loss of trust in healthcare providers. Moreover, their occurrence increases mortality risk [19].
Conclusions
Close collaboration with a device specialist is the cornerstone of the management of patients living with an ICD. History of ICD shocks, examination of the pocket, being informed about the AF episodes and markers of a possible disease progression are among the most important factors. Table 1 summarises the areas of cooperation. More widespread use of remote monitoring systems will definitely improve the standard of care of this patient population. Frequency of follow-up at a private cardiology practice should generally be based on the nature and severity of the underlying heart disease.
Table 1. Areas of cooperation between the private cardiologist and device specialist.
| Duties of Private Cardiologist | Competence of Device Specialist |
|---|---|
| Pocket examination | Pocket infection, erosion |
| Signs of systemic infection | Lead-related endocarditis |
| ECG (rhythm, QRS width and morphology) | Undersensing, pace dependence, upgrade |
| Echocardiography (lead, pericardium, LVEF) | Pericardial effusion, vegetation |
| History of shocks and unexplained faints | Electrical storm, inappropriate shocks |
| Diagnostic information from device memory | Full system interrogation, telemonitoring |
| Frequency of in-office follow-up depends on underlying heart disease | Frequency of in-office follow-up depends on telemonitoring capability, ventricular arrhythmia burden, and pocket condition |















