Introduction
Resting echocardiography is the most important tool for diagnosing valvular heart disease; however, the decision for intervention is primarily based on exercise-induced symptoms. Therefore, functional testing is helpful to assess symptoms with exertion, especially in patients with discordance between symptoms and the severity of valve disease. Moreover, mitral valve disease has a dynamic component, being load-dependent or increasing with exercise. Exercise echocardiography may provide the necessary clues in determining changes in cardiac haemodynamics. In this document, the additive diagnostic and prognostic value of stress testing in native mitral valve disease and the effect of pharmacologic therapy on lesion severity will be discussed.
Mitral regurgitation
Mitral regurgitation (MR) has a variety of aetiologies and is characterised by an insidious progression. Primary (organic) MR is a disease of one or more components of the mitral valve apparatus, whereas secondary (functional) MR results from geometric disturbance of the left ventricle (LV) in the presence of a structurally normal valve [1].
Rationale for exercise testing in mitral regurgitation
In the compensated stage, patients with severe MR remain asymptomatic for years to decades. The onset of symptoms represents a key development since symptom presence is a well-known predictor of adverse outcome and a class I indication for surgery [2-4], yet symptom status is highly subjective. Many patients with severe MR may not recognise their slowly and insidiously progressing symptoms, may deny them, or may adopt a sedentary lifestyle to remain asymptomatic. Therefore, in allegedly asymptomatic patients, a standard exercise stress test is helpful to confirm or disprove the absence of symptoms with daily life activities, can be used to objectively assess functional capacity, and can provide the baseline for future symptom assessment. Patients with symptoms provoked by exercise testing should be considered symptomatic with potential therapeutic implications, even if the patient history is equivocal. Markedly reduced functional capacity is associated with a higher rate of events under medical management and should lead to consideration of mitral valve surgery [5].
Symptoms of chronic primary MR usually occur during physical activity. Nevertheless, echocardiographic assessment has conventionally been made in the resting state. When symptomatic status and standard echocardiographic measurements are discordant, or the magnitude of left heart enlargement seems to be out of proportion to the severity of resting MR, it may be useful to take measurements during or after exercise under the notion that only under conditions of cardiovascular stress does the degree of MR increase and exercise-limiting symptoms develop. The same concept underlies the detection of exercise-induced ischaemia and diastolic stress testing.
Exercise modalities
Exercise echocardiography can be performed using either a treadmill or a bicycle. When a treadmill exercise test is performed, scanning during exercise is not feasible, and has to be accomplished immediately post-exercise after placing the patient in a left lateral decubitus position. The most important advantage of bicycle exercise testing is the chance to obtain images during various levels of exercise rather than relying on post-exercise imaging. With the development of ergometers that permit a supine position of the patients with leftward tilting, the feasibility of image acquisition has been further improved. Nevertheless, obtaining good echocardiographic data during exercise can be a challenging task due to tachypnoea and tachycardia, and, when obtained post-exercise, should be done immediately after the treadmill exercise is terminated (ideally within 60-90 seconds) as severity of MR and pulmonary hypertension can rapidly decrease [6-8]. These circumstances undoubtedly require a higher level of experience than that needed for performing an echocardiographic study at rest. Provided that the acoustic window is acceptable, and the necessary expertise is available, exercise echocardiography has the advantages of its wide availability, low cost, and diagnostic accuracy for assessment of the dynamic component of MR.
Dobutamine stress echocardiography (DSE) should not be used instead of exercise to assess the dynamic behaviour of MR because the effect of dobutamine on loading conditions is a major confounding variable and administration of the drug does not simulate day-to-day physiologic stress [9]. In fact, paradoxically, the severity of MR can decrease during dobutamine provocation if LV size decreases at the same time [8]. Although there is no general role for pharmacologic stress echocardiography to evaluate the severity of MR or direct its management [6], one exception to this is when inducible ischaemia is suspected in a patient who cannot perform a physical exercise test, as ischaemia may be the mechanism of MR [10]. Low-dose DSE may also be useful in ischaemic heart disease by identifying viable myocardium, which in turn may influence management of ischaemic MR (ESC 2017; ACC/AHA 2014: Class I, Level of Evidence: C).
There are no published studies on the use of acute volume challenge as a diagnostic manoeuvre in patients with non-severe MR to aggravate the degree of MR for clinical decision making.
Doppler imaging modalities
Two-dimensional (2D) and Doppler echocardiography can elucidate the mechanism and assess the severity of MR. Colour Doppler echocardiography is an important cornerstone supplemented by pulsed and continuous wave Doppler for exact quantification [6]. Poor left ventricular contractile function with a lower driving pressure encountered in functional MR results in a lower jet momentum reducing the jet size in the left atrium and, thus, can cause underestimation of MR severity by visual assessment alone.
Vena contracta
The vena contracta (VC) is the narrowest portion of the regurgitant flow that occurs at or immediately downstream of the regurgitant orifice and corresponds to the effective regurgitant orifice area (EROA). The VC is typically imaged in a view perpendicular to the commissural line (e.g., in the parasternal long-axis or apical four-chamber view) using a careful probe angulation to optimise the flow image, coupled with the zoom mode to improve resolution and measurement accuracy [11]. The size of the hydraulic VC is independent of flow rate and driving pressure for a fixed orifice and provides a semiquantitative approach to evaluate MR severity at rest and during exercise [6]. However, given the small values of the width of the VC, small errors in its measurement may lead to a large percent error with the potential for misclassification of the severity. Therefore, this parameter is only useful in cases with large exercise-induced increases in mitral regurgitant flow; quantitative methods should be utilised whenever possible [12].
Quantitative Doppler methods
The severity of MR can be quantified at rest and during exercise by measuring the EROA or the regurgitant volume (RV) either through the proximal isovelocity surface area (PISA) method or the quantitative Doppler method by subtracting the aortic from the mitral (= total) stroke volume equal to the stroke volume derived from the biplane method of discs (Simpson’s method) [7,13]. Both methods are reproducible and have been validated, but also rely on some simplifications and assumptions [6]. For example, the quantitative Doppler method assumes that the aortic valve does not suffer from substantial aortic regurgitation. The PISA method is based on the assumption of a hemispheric flow convergence zone, which may be at variance with elliptical regurgitant orifices frequently encountered in functional MR and the potential to underestimate the severity when only the vertical and not the horizontal length of the PISA zone is used for calculation [6]. Moreover, because of the phasic variation of the regurgitant orifice area during systole, both overestimation and underestimation of the mitral regurgitant stroke volume are possible, particularly in functional MR [14]. However, during an exercise echocardiography each patient serves as his or her own control and some errors may cancel out. The limitations of an exercise echocardiographic study are predominantly of a technical nature and can be overcome with a diligent examination.
Left ventricular function in asymptomatic patients with severe primary mitral regurgitation
When MR is severe at rest, there is no need to reassess the severity during exercise. Instead, an exercise stress test can be performed for prognostic reasons to assess the kinetic changes in LV contractility. Generally, the preload-dependent LV end-diastolic volume reflects the severity of chronic MR, while the afterload-dependent LV end-systolic volume is a more sensitive measure of LV contractility. One of the major concerns in asymptomatic MR patients who are followed medically is latent LV dysfunction which is predictive of poor prognosis after MV surgery but may not be detected with resting echocardiography. Stress echocardiography can be of value in minimally symptomatic patients with MR by disclosing latent LV dysfunction as manifested by an inadequate increase in ejection fraction and a larger end-systolic volume at exercise, which would imply that the limits of cardiac compensation have been reached [15]. Moreover, the absence of LV contractile reserve in patients with asymptomatic severe primary MR defined as a post-exercise ejection fraction increment of <4% [16] or global longitudinal strain increment <2% [17] confers a poor prognosis. In daily practice, a widely available and easy to perform symptom-limited exercise test provides valuable prognostic information based on exercise parameters alone: in asymptomatic patients with significant myxomatous MR, reduced exercise capacity and impaired heart rate recovery after exercise were independently associated with adverse long-term clinical outcomes in addition to known factors such as atrial fibrillation, pulmonary hypertension, and reduced LV ejection fraction [18]. Conversely, in asymptomatic patients with significant myxomatous MR achieving >100% predicted metabolic equivalents, delaying surgery by ≥1 year does not adversely affect outcome [19].
Clinical implications
Although exercise stress echocardiography is useful for unmasking latent LV dysfunction and predicting post-operative LV ejection fraction [20], the lack of contractile reserve as a marker of more severe disease has not been included in the guidelines for clinical decision making [2-4]. Myocardial deformation imaging including global longitudinal strain could be of potential interest for the detection of subclinical LV dysfunction at rest or assessment of LV contractile reserve with exercise to better define the optimal timing of intervention. However, this novel approach has not yet been translated into firm clinical recommendations, partly because of inconsistent algorithms used by different echocardiographic systems pending further studies [2-4].
Exercise-induced changes in the severity of primary mitral regurgitation
Primary MR results from a disease of the mitral valve apparatus and appears to have an important dynamic character during exercise in up to one third of patients [7]. The increase in the severity of MR during exercise assessed by the EROA may result from changes in mitral annular area or may possibly be related to an exercise-induced reduction in LV systolic volume by increasing the extent of the leaflet prolapsed, but cannot be explained by an increase in the transvalvular pressure gradient related to an elevated systolic blood pressure. Importantly, the exercise-induced changes in MR severity could not be predicted from the resting values [7], and the severity of MR at rest has only a weak association with functional capacity [5], emphasising the incremental benefit of exercise echocardiography. In addition, a marked exercise-induced increase in MR severity was associated with reduced symptom-free survival and may identify a group of patients at risk of rapidly developing symptoms to be followed up more closely. Changes in MR severity are associated with exercise-induced changes in systolic pulmonary artery pressure (SPAP) [7,21]. When suboptimal acoustic windows do not allow accurate quantification of MR, the simple measurement of SPAP may be less demanding and still provides helpful information.
Systolic pulmonary artery pressure and tricuspid annular plane systolic excursion
The utility of obtaining the peak tricuspid regurgitant (TR) jet velocity as an estimate of mean left atrial pressure (LAP) is based on the fact that elevated SPAP during exercise is strongly suggestive of elevated LV filling pressures resulting from an exercise-induced increase in MR severity provided that no pulmonary parenchymal or vascular disease is present. SPAP can easily be determined from the systolic right ventricular–to–right atrial gradient (calculated from the peak velocity of the systolic trans-tricuspid regurgitant flow using the modified Bernoulli equation) augmented by the right atrial pressure that can be estimated from the dimension of the inferior vena cava and its collapsibility in the subcostal view. For practical purposes, it can be assumed that the right atrial pressure remains unchanged from rest to exercise. Exercise SPAP is more accurate than resting SPAP for predicting the occurrence of symptoms in patients with asymptomatic MR [7,21,22].
Tricuspid annular plane systolic excursion (TAPSE) is a readily available and feasible validated parameter of global right ventricular (RV) function. Limited RV contractile recruitment defined as TAPSE <18 mm provides incremental prognostic information in patients with moderate or severe asymptomatic mitral regurgitation in addition to exercise-induced pulmonary hypertension [22].
Clinical implications
Until now, American and European guidelines have never considered isolated moderate regurgitant valvular lesions indications for surgery. In contrast, the case for surgery or intervention in moderate MR that further worsens during exercise seems easier to make. In addition, exercise echocardiography may add additional prognostic value beyond conventional exercise treadmill testing in patients with asymptomatic moderate or severe chronic primary MR. Nevertheless, an exercise-induced increase in MR severity has not yet been incorporated into the European Society of Cardiology (ESC) and American College of Cardiology/American Heart Association (ACC/AHA) guidelines [2,3], partly because of potential errors in quantitative Doppler methods and paucity of outcome data. Likewise, the development of pulmonary hypertension on exercise echocardiography has been proposed for clinical decision making regarding intervention in primary MR. Nevertheless, this criterion - in contrast to resting pulmonary hypertension (PHT) - is currently not included in the guidelines [2,3], due to possible confounding factors such as LV diastolic dysfunction and intrinsic pulmonary disease.
Chronic secondary (functional) MR
In contrast to primary MR, secondary MR is not a disease of the mitral valve itself but rather a disease of the left ventricle [1]. Secondary MR (Carpentier classification types I and IIIb) results from a functional imbalance between increased tethering forces (annular and left ventricular dilation, segmental or global left ventricular dysfunction with papillary muscle displacement/dysfunction) and decreased closing forces (reduced left ventricular contractility or synchrony) during systole with incomplete leaflet coaptation [23]. The term secondary MR includes both ischaemic and non-ischaemic functional causes and could be a mere marker for more advanced LV dysfunction with a higher cardiac event rate, a possible contributor to myocardial disease progression through additional LV volume overload, or both. This frequently occurring entity needs to be distinguished from the much rarer type of exercise-induced MR resulting from inducible myocardial ischaemia in coronary artery disease due to reversible regional wall motion abnormalities usually in combination with severe worsening of LV function [10].
Chronic ischaemic mitral regurgitation (IMR) as a result of myocardial infarction with an EROA ≥20 mm2 (defined as severe in the ESC guidelines and moderate in the ACC/AHA guidelines [2,3]) is a powerful independent predictor of heart failure and death [24]. This value differs from the 40 mm2 cut-off traditionally used in primary MR [2] and may account for the dynamic nature of secondary MR, which is frequently underestimated at rest. Secondary MR is phasic throughout systole and dynamic during exercise and with changing loading conditions as a result of pharmacologic therapy. Secondary MR increases during exercise in the majority of patients with LV dysfunction, both with ischaemic and non-ischaemic aetiology, but may also remain unchanged or even decrease [23,25]. The direction and magnitude of exercise-induced changes in MR severity are more related to local LV remodelling with concomitant mitral valve shape change rather than changes in LV volumes [25]. In non-ischaemic cardiomyopathy, the severity of secondary MR sometimes decreases with exercise because of contractile recruitment. The degree of ischaemic MR at rest is unrelated to exercise-induced changes in EROA or RV [12,25]. Thus, resting evaluation of ischaemic MR may underestimate the full severity of the lesion and its consequences. In patients with ischaemic heart disease and LV dysfunction, large exercise-induced increases in MR severity (increases in EROA ≥13 mm2) have been shown to be associated with symptoms and to identify patients at high risk of mortality and morbidity [26,27].
Clinical implications
An exercise-induced increase in secondary MR severity is associated with a reduced exercise capacity in both ischaemic and non-ischaemic cardiomyopathy [28]. Possible mechanisms include a blunted increase in forward stroke volume and increases in left atrial and pulmonary artery pressure with exercise. Furthermore, this backward haemodynamic cascade triggered by exercise-induced increases in MR severity may even contribute to the development of acute pulmonary oedema [13].
Drug effects in mitral regurgitation
Chronic functional MR develops as a consequence of LV systolic dysfunction (heart failure with reduced ejection fraction [HFrEF]). Randomised controlled trials have shown that pharmacologic therapy targeting pathological LV remodelling with beta-blockers (BB), angiotensin-converting enzyme inhibitors (ACE-I), angiotensin receptor blockers, neprilysin inhibitors, aldosterone antagonists, angiotensin receptor neprilysin inhibitorhydralazine plus nitrates, and diuretics independently improve symptoms and/or reduce mortality in symptomatic patients with HFrEF [29]. Despite the widespread use of these drugs, haemodynamic and volumetric data on the effects of the agents in chronic functional MR are relatively sparse. In HFrEF, combined preload and afterload reduction with vasodilators and diuretics in the short term produced an increase in forward stroke volume despite a decrease in LV end-diastolic volume, at least in part through a redistribution of mitral regurgitant flow via a reduction in EROA [30,31]. Of note, this favourable reciprocal relation between forward stroke volume and mitral regurgitant volume at rest was also maintained during upright exercise [30]. The negative impact of functional MR on prognosis in both the ischaemic and non-ischaemic category has been linked to adverse LV remodelling, partly due to the presence of ongoing volume overload. Theoretically, effective medical therapy reducing LV end-diastolic volume and leading to reverse remodelling should also improve functional MR. Supporting evidence comes from small trials in patients with HFrEF that have shown beneficial effects of short- and medium-term therapy with ACE-I [32] and BB [33] on left ventricular size and severity of mitral regurgitation in association with an increase in forward stroke volume. Interestingly, the presence of functional MR in severe heart failure was found to be a predictor for a salutary response to intense pharmacotherapy [34]. Over a longer time period, optimal medical heart failure therapy has been shown to produce a sustained reduction in severe functional MR with prevention or least attenuation of adverse LV remodelling in association with an improved long-term prognosis [35]. The evolution of functional MR has an even more significant prognostic importance than baseline severity and could be used for risk stratification, emphasising the additive prognostic value of periodic reassessment of MR severity because of the exquisite load dependence of functional MR.
Heart failure with reduced ejection fraction
In contrast to functional MR, there is no convincing evidence to support the prophylactic use of heart failure medication in asymptomatic patients with primary severe MR and normal LV systolic function since the primary process is not addressed [2,4]. However, in those patients in whom surgery is not performed or will be delayed, medical therapy for systolic dysfunction with the standard regimen for heart failure should be implemented. The same approach is reasonable for patients with persistent symptoms after mitral valve surgery. Likewise, standard antihypertensive treatment is indicated in patients with severe primary MR and concomitant hypertension to reduce the morbidity and mortality associated with hypertension and because increased LV systolic pressure by itself increases the systolic transmitral gradient and worsens the severity of MR.
Intraoperative transoesophageal echocardiography may underestimate the degree of organic and functional MR using quantitative and semiquantitative methods compared to the preoperative baseline evaluation because of the unloading effect of general anaesthesia on the LV [36]. Therefore, the evaluation and decision to treat MR should be made before surgery and not under general anaesthesia. In cases where preoperative assessment of MR is not available, intraoperative acute volume or pressure loading challenge with phenylephrine, an alpha-agonist agent, can be used to attenuate the effects of general anaesthesia to return the MR severity to values equal to or greater than baseline.
Mitral stenosis
Mitral stenosis (MS) is an obstruction to LV inflow most frequently following rheumatic fever. In developed countries, mitral annular calcification encroaching into the leaflets is increasingly recognised and congenital MS (including parachute mitral valve) belongs among the rarest causes. Two-dimensional and Doppler transthoracic echocardiography can show decreased opening of the mitral valve leaflets and increased blood flow velocity during diastole. Mitral valve area (MVA) determined by planimetry is the reference measurement of MS severity, whereas mean transmitral gradient and SPAP reflect its consequences and have a prognostic value [37]. The maximal gradient is of little interest as it derives from peak mitral velocity, which is influenced by left atrial compliance and LV diastolic function. The European and American guidelines [2,4] both suggest an intervention in symptomatic patients with an MVA <1.5 cm2 (defined as moderate in the ESC guidelines and severe in the ACC/AHA guidelines).
Exercise echocardiography in mitral stenosis
Exercise echocardiography is most valuable in MS when discordance exists between symptoms and the severity of stenosis evaluated at rest (symptomatic moderate MS or asymptomatic severe MS) [2,4,37]. In addition, because indexed valve areas are not defined for MS, stress testing may be useful for assessing MS severity in patients with large body surface area [37]. The ESC guidelines recommend an exercise test to provoke symptoms in asymptomatic patients with resting echocardiography that demonstrate severe MS to identify candidates for valvular intervention [2]. A stress test may also be useful to predict haemodynamic reserve and assess the likelihood of decompensation with increased flow prior to planned pregnancy or major non-cardiac surgery [9]. Exercise echocardiography can be performed using a supine bicycle, allowing data acquisition at various stages of exercise, or upright treadmill with images obtained immediately after stress for non-invasive assessment of clinically relevant increases in mean transmitral gradient and/or pulmonary artery systolic pressure with stress. Both of these pressures rise with exercise through an increase in cardiac output and heart rate with a consecutive shortening of diastolic filling time, resulting in exponential increases in left atrial and pulmonary capillary pressures. As in the case with aortic stenosis, the transmitral pressure gradient is related to valve area but is more sensitive to heart rate than the systolic transaortic gradient because the proportion of the cardiac cycle occupied by diastole decreases with increasing heart rate, thereby increasing the mean flow rate across the mitral valve. Therefore, heart rate should always be included in the report due to the differential impact of tachycardia on diastolic versus systolic duration. Figure 1 depicts an example of the tracings from a representative patient.
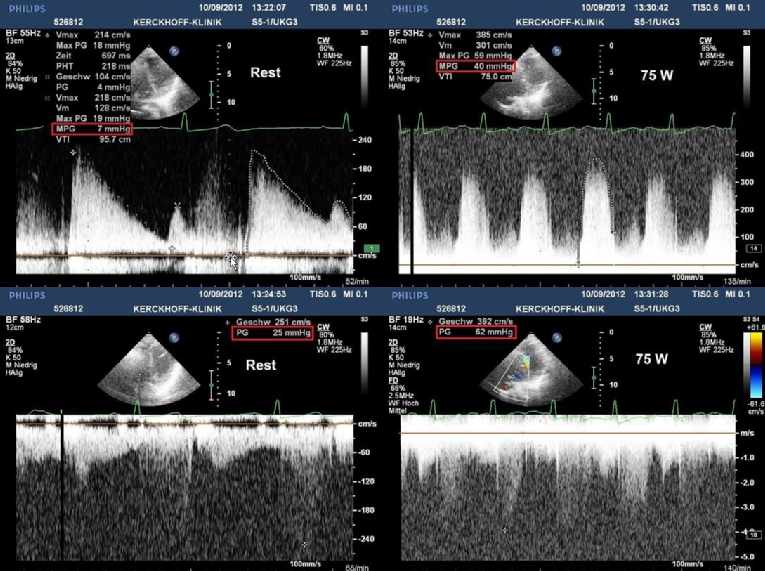
Figure 1. Exercise stress echocardiography in a patient with mitral stenosis and equivocal symptoms.
Rest (left) and peak exercise (right) continuous wave Doppler recordings across the mitral (top) and tricuspid valves (bottom). With exercise, the heart rate increased from 57 to 139 beats/min, the mean transmitral diastolic pressure gradient markedly from 7 to 40 mmHg and the SPAP (calculated as the sum of the trans-tricuspid pressure gradient and the estimated right atrial pressure) from 30 to 67 mmHg. The right atrial pressure was assumed to remain constant at 5 mmHg throughout the stress test.
While exercise is generally preferred as the more physiological test, increased chest motion in a hyperventilating patient during physical exercise can sometimes make imaging difficult. Alternatively, DSE can be used if exercise testing yields suboptimal results or cannot be performed, since it simulates the effects of exercise by increasing cardiac output and heart rate and can predict event rates in symptomatic patients with moderate disease [38]. Gradient thresholds for severe MS have been proposed as >15 mmHg on exertion or >18 mmHg during dobutamine infusion [38,39], but there are limited data to support these specific parameters over exercise-induced symptoms to be included in the society’s guidelines. Likewise, exercise-induced pulmonary hypertension, defined as an SPAP >60 mmHg, is no longer included in the guidelines for clinical decision making but is another marker of haemodynamically significant MS and should alert the clinician to consider the patient’s symptoms carefully. Interestingly, an early increase in SPAP, at low-level exercise, was found to be superior at predicting the development of dyspnoea and/or referral for valvular intervention than the presence of SPAP >60 mmHg alone [40]. Importantly, DSE is not recommended for assessment of SPAP.
Combined mitral valve disease
Particularly in rheumatic heart disease and less frequently in degenerative valve disease, significant stenosis and regurgitation can be found on the same valve. It is important to recognise that the coexistence of stenosis and regurgitation may have pathological consequences that are incremental to the effects of either of these disease states alone, and the pressure gradients become of major importance for assessment. Exercise haemodynamic studies should be considered for those patients with symptoms that are out of proportion to haemodynamic findings at rest. In particular, patients with mixed mitral valve disease and a relatively low mitral gradient at rest may be particularly susceptible to developing functional MS at higher transvalvular flow rates with exercise due to the concomitant regurgitant volume [4]. There is a paucity of data on the natural history of such a condition, which does not allow evidence-based recommendations. The decision to pursue surgical therapy should be individualised [2].
Haemodynamics after percutaneous mitral valve repair
Transcatheter mitral valve repair with the MitraClip® device (Abbott Vascular, Santa Clara, CA, USA) decreases the MVA, potentially creating an iatrogenic MS with an increase in mean transmitral gradient under resting conditions and a further increase during exercise, but without more heart failure symptoms [41]. The lack of effect on clinical status may be explained by an increase in post-procedural cardiac output after MR reduction.
Drug effects in mitral stenosis
Data on the effects of BB therapy in MS and normal sinus rhythm (NSR) are sparse and the results are conflicting. Although heart rate is reduced and consequently the diastolic filling period prolonged at rest and during exercise, functional capacity does not improve in patients with severe MS despite a decrease in transmitral gradients [42]. The guidelines do not support the general use of BB for patients with MS in NSR [2,4]. Other negative inotropic agents have not been studied in this setting.
Indications for stress echocardiography in mitral valve disease.
- Symptoms out of proportion to the severity of primary MR at rest (ESC 2017; ACC/AHA 2014, Class IIa, Level of Evidence: B)
- Establishment of symptom status and exercise tolerance in chronic primary MR (ESC 2017; ACC/AHA 2014, Class IIa, Level of Evidence: C)
- Quantification of exercise-induced changes in the severity of primary MR (of borderline significance), LV function and SPAP for individual risk stratification (ESC 2017)
- Determination of the aetiology in chronic secondary MR (ACC/AHA 2014, Class I, Level of Evidence: C) and its dynamic characteristics during exercise (ESC 2017)
- Myocardial viability testing with dobutamine in patients with secondary ischaemic MR to identify candidates for revascularisation (ESC 2017; ACC/AHA 2014: Class I, Level of Evidence: C)
- Pulmonary oedema without an obvious cause
- Severe MS in asymptomatic patients (ESC 2017; ACC/AHA 2014: Class I, Level of Evidence: C)
- Mild or moderate MS in symptomatic patients
- Combined MS and MR of uncertain significance















