Three-dimensional imaging
Three-dimensional (3D) imaging allows cardiac imaging in multiple tomographic planes [1]. It involves volume data set acquisition over one or more heartbeats.
The role of 3D imaging in the assessment of mitral regurgitation
Three-dimensional imaging aids in the assessment of severity of valvular regurgitation and in establishing its mechanism. Traditionally, 2D imaging requires obtaining multiple views of the mitral valve (MV) in order to make a detailed assessment of MV morphology [1]. The aforementioned technique increases the study time and requires expert interpretation. In contrast, 3D imaging allows a rapid, detailed assessment of MV morphology by obtaining real-time, surgical views of the MV. This provides information on the mechanism of the regurgitation, such as scallop prolapse, chordal rupture, clefts, leaflet perforation, restricted motion of leaflets, and so forth (Figure 1) [1]. This information facilitates planning of surgical treatment options. This aspect of 3D imaging is useful in planning MV repair and enabling newer transcatheter procedures as it allows attainment of an ‘en face’ view of the MV [1,2]. Real-time 3D echocardiography using transoesophageal echocardiography (TEE) allows rapid diagnosis of MV pathology and is therefore particularly useful during intraoperative MV repair [2]. Additionally, it enables a detailed segmental analysis of the MV by viewing it in a multiplane reconstruction format, both on transthoracic and TEE.
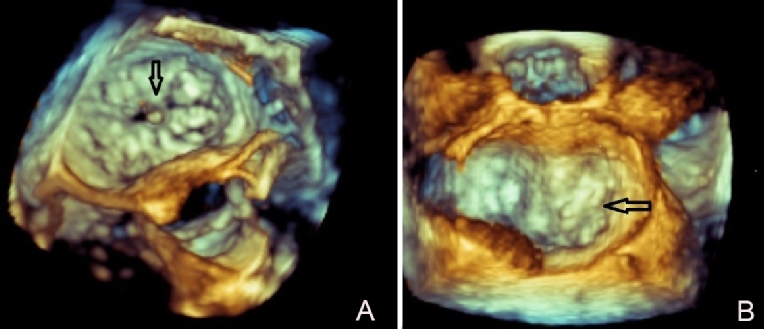
Figure 1. Three-dimensional en face views of a myxomatous mitral valve.
A) Myxomatous mitral valve with multi-segment prolapse and superimposed vegetation (arrow).
B) Prolapse of A2 and A3 scallop in a patient with myxomatous mitral valve disease.
Three-dimensional colour Doppler imaging of the MV is feasible and reproducible. It is especially useful for quantification of eccentric jets [1]. The origin, size and shape of the jets is better visualised with 3D. Severity of valvular regurgitation can be accurately quantified using 3D measurement of the vena contracta [2]. Following numerous technical issues with 2D proximal isovelocity surface area (PISA) measurement to quantify MV regurgitation, development of real-time, single-beat 3D echocardiographic colour Doppler imaging now allows measurement of PISA without geometric assumptions.
Recently, real-time 3D echocardiography has proven useful for transcatheter structural heart disease interventions. It has enabled successful outcomes for MitraClip® (Abbott Vascular, Santa Clara, CA, USA) procedures in functional mitral regurgitation (MR) [2]. In this context, it helps in optimisation of transseptal puncture, guiding of the clip delivery apparatus and, finally, positioning of the clip in relation to the valve orifice. It also aids in detection of any post-procedural residual MR by 3D colour Doppler.
The lack of dependence of 3D imaging, as compared to 2D echocardiography, on geometric remodelling and image planes allows more accurate quantification of left ventricle (LV) ejection fraction in MR [3]. This aids decisions regarding surgical timing and accurate evaluation of postoperative LV systolic function.
A few studies have evaluated 3D imaging in refining criteria for MV prolapse by studying the structure of the mitral annulus in three dimensions [3]. Three-dimensional imaging has permitted differentiation of ischaemic from non-ischaemic MR by allowing a detailed analysis of the valvular and subvalvular apparatus of the MV [3]. Functional MR is associated with dilatation of the annulus and decreased cyclic variability in the shape and area of the annulus. A detailed analysis of the annular geometry in ischaemic MR revealed an increased intercommissural and anterior posterior diameter [3]. Furthermore, there was greater tethering of the leaflets, resulting in leaflet tenting when compared to normal subjects.
The role of 3D imaging in the assessment of mitral stenosis
The main advantage of 3D echocardiography in mitral stenosis (MS) is in more precise quantification of the MV area [1-3]. Due to the funnel shape of the valve orifice in some cases, 2D planimetry is inadequate to accurately measure the valve orifice. Three-dimensional echocardiography, with the aid of multiplane reconstruction, allows the accurate location of the smallest MV orifice and thus a better quantification of the true anatomic orifice area (Figure 2). This allows accurate assessment of the severity of MS pre and post surgery, or balloon mitral valvuloplasty when gradients, calculation of MV area by pressure half-time method and 2D planimetry are of limited value due to altered compliance of the left atrium (LA) and LV [3]. Furthermore, heavy calcification of the MV can cause errors in measurements on 2D planimetry [1]. This shortcoming of 2D imaging is overcome by 3D imaging as it allows clear imaging of the orifice from the en face view which, when viewed from the LA aspect, creates less blooming artefact.
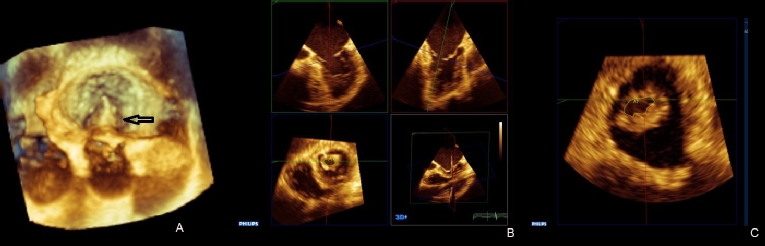
Figure 2. Three-dimensional assessment of rheumatic mitral stenosis.
A) Three-dimensional image of a rheumatic mitral valve depicting diastolic doming of the anterior mitral leaflet (arrow) prior to balloon valvuloplasty (B). C) Multiplane reconstruction of mitral valve for calculation of mitral valve area to assess the severity of mitral stenosis.
Three-dimensional echocardiography plays an important role in detailed evaluation of the valve, including the commissures, prior to balloon valvuloplasty [1]. During the procedure, it aids in transseptal puncture and in the assessment of complications, such as leaflet tear and MR. Post-procedure, it allows a more accurate quantification of the MV area, and adequate splitting of the commissures.
Limitations of 3D imaging
The 3D image quality is dependent on adequate acoustic window. Suboptimal temporal and spatial resolutions are further limitations of 3D echocardiography. In patients with disturbances of rhythm and respiratory motion, the image acquisition is prone to stitch artefacts [4].
Strain imaging
Myocardial mechanics can be assessed using strain imaging. Both tissue Doppler and speckle tracking can be used to measure myocardial displacement. Strain measures myocardial deformation. It is the fractional change in the length of a segment of the myocardium [2].
The role of strain imaging in mitral regurgitation
Chronic MR is associated with LV remodelling and dysfunction [2]. Multiple studies in chronic severe rheumatic MR have shown that a reduction in baseline global longitudinal strain (GLS) is a sign of a subclinical LV decompensation, and results in reduced LV ejection fraction post-surgery in patients after MV repair [5]. A decrease in GLS of ≥19.9% is a strong predictor of future LV dysfunction. Current guidelines do not include decline in GLS as an indication for surgery due to inconsistencies in strain measurement algorithms by different vendors [6].
In patients with asymptomatic significant MR, reduced peak LA reservoir strain and strain rate in the LA filling phase predicted a worse outcome [7]. Abnormalities in LA strain and strain rate in MR are increasingly being used as a predictor of accelerated LA remodelling and for possible risk stratification for optimal surgical timing [8].
The role of strain imaging in mitral stenosis
Few studies have explored strain imaging of the LV in MS [9]. All have noted a decline in LV GLS in MS. Some have shown that this finding may be predictive of progression of MS, whereas others have shown no correlation between LV longitudinal strain and severity of MS [9-11]. Thus, the clinical relevance of reduced LV GLS in MS remains uncertain. Decline in LA strain has been shown to be correlated with heart failure in a recent study by Chien et al [12].
Limitations of strain
Strain is affected by technical factors such as image quality, tracking, contouring, region of interest, and choice of segmentation model. Biologic factors such as race, gender, and age, as well as haemodynamic factors such as medications and volume status, are additional sources of variability in strain [13].
Intracardiac echocardiography
Intracardiac echocardiography (ICE) utilises a phased-array transducer [14]. It can be used as an alternative in patients where TEE is not an option as an imaging modality [2]. ICE can aid MitraClip implantation and mitral valvuloplasty [15]. It can guide transseptal puncture, and advancement and positioning of the MitraClip device. It can also be used to evaluate post-procedural outcome.
Limitations
Alternating between image planes that are perpendicular to depict one area is difficult on ICE [14].
Fusion imaging
Fusion imaging involves projection of cardiac images (echocardiographic and computed tomography) onto fluoroscopy for a comprehensive representation of the anatomy [2]. It can be used to guide interventions in structural heart disease. It has been used for safe guidance of transcatheter mitral repair with the MitraClip device, percutaneous paravalvular leak closures, and transcatheter MV replacement [16]. It has been shown to reduce fluoroscopy and procedure time, as well as radiation exposure and contrast dose. Further studies are needed to fully understand the role of fusion imaging in MV disease.
Limitations
To date, there is only limited evidence that fusion imaging improves the safety and outcomes of structural heart disease interventions over the standard approach [16].
Conclusion
Echocardiography plays an important role in the assessment of mitral valve disease. Advances in three-dimensional imaging, strain and emerging hybrid imaging and intracardiac echocardiography are crucial to understand mitral valve pathology and improve patient outcomes.















