Background
Mitral regurgitation (MR) is a growing international chronic disease phenomenon. The epidemiological data demonstrate that moderate or severe regurgitation is the most frequent valve disease in the USA [1] and the second most common form of valvular heart disease in need of surgical repair in Europe. MR remains a growing international public concern despite a significant reduction in worldwide rheumatic heart disease. Moderate to severe MR increases in prevalence with increasing age, with nearly 2.0 to 2.5 million people in the USA affected in 2000, which may almost double in number by 2030 attributable to an ageing population [1].
When assessing chronic MR, the regurgitation has been divided into two “simple” categories: primary and secondary MR. In secondary MR, the mitral valve apparatus is “normal” and the MR is associated with severe left ventricular dysfunction. Left ventricular function may be further characterised into ischaemic chronic secondary MR or idiopathic chronic secondary MR. The abnormal and dilated left ventricle (LV) displaces the papillary muscles, causing leaflet tethering and eventual mitral annular dilation which prevents leaflet coaptation. In chronic secondary MR, the restoration of the mitral valve (MV) competence is not curative; the causes of secondary chronic MR are multifactorial [2].
The AHA/ACC Guidelines of 2017 [2] state that the Doppler methods using transthoracic echocardiography (TTE) are the standard for calculations of the effective regurgitant orifice area (EROA) by the flow convergence method, even though this may underestimate the severity due to the crescentic nature of the mitral annulus. The mitral valve apparatus is a dynamic structure with complex interactions with surrounding anatomy. Therefore, multiple parameters must be used to determine MR severity. The current recommended definition of severe secondary MR is now the same as for primary MR (EROA ≥0.4 cm2 and regurgitant volume ≥60 mL), with the understanding that the EROA cut-off of >0.2 cm2 is more sensitive and >0.4 cm2 is more specific for severe MR [2]. A prospective study of 456 patients with asymptomatic severe MR reported increased mortality and cardiac events as the degree of regurgitation increased, with the poorest outcome when the EROA was ≥0.4 cm2 [2,3]. The new ESC/EACTS guidelines recommend surgery in patients with severe primary MR and symptoms, or in asymptomatic patients with an LV ejection fraction (LVEF) ≤60% and/or LV dilatation (end-systolic diameter [ESD] ≥45 mm) (class I), new onset atrial fibrillation or pulmonary hypertension (PHT) (class IIa) [4].
The 2017 ESC valvular guidelines have similar indications for surgery in severe chronic primary MR. Surgery is indicated in symptomatic patients with severe primary MR and an LVEF <60% or LVESD >45 mm, atrial fibrillation and a systolic pulmonary pressure >50 mmHg. These predict a worse postoperative outcome independent of the symptomatic status and have therefore become triggers for surgery in asymptomatic patients. In patients with flail leaflet, an LVESD of 40-44 mm has been reported to predict a worse outcome compared with LVESD <40 mm [5].
“Mitral regurgitation begets mitral regurgitation”. The perpetual cycle of primary MR causing LV wall stress, LV dilatation and “stressing” the mitral valve apparatus causing more severe MR with increasing LV volumes seems inevitable. Longstanding volume overload leads to irreversible LV dysfunction and a poorer prognosis. The LV eventually forms a more spherical shape, leading to decreased ventricular function with reduced myofibre content and interstitial fibrosis [6].
The most common cause of primary MR is myxomatous degeneration of the MV leaflets eventually leading to MV prolapse. The spectrum of severity of myxomatous degeneration ranges from fibroelastic deficiency, with thin leaflets and focal prolapse, to Barlow’s disease, with diffusely thickened and redundant leaflets [7]. Primary MR can also occur from leaflet perforation and cleft leaflets, which are deep indentations that extend to the annulus. Rheumatic disease, drugs, radiation, and connective tissue disease can cause restricted leaflet motion from thickening of the leaflet edges and subvalvular apparatus [8,9]. In an ageing population, mitral annular calcification leads to eventual degeneration of the MV and primary MR.
Patients with severe MR who develop an EF ≤60% or LVESD ≥40 mm have already developed LV systolic dysfunction [2]. One study has suggested that, for LV function and size to return to normal after MV repair, the LVEF should be >64% and LVESD <37 mm [10].
Natural history studies of MR have shown a poor outcome of untreated severe primary MR. Overall, 90% of patients who presented with severe MR due to a flail leaflet were dead or required surgery at 10-year follow-up [11]. There is a 30% incidence of atrial fibrillation and 63% incidence of heart failure, both of which were shown to be independently associated with reduced survival [3]. The outcome of patients with severe MR depends on the initial symptoms and the presence or absence of ventricular dysfunction. Patients with severe MR and New York Heart Association functional Class I and II who did not undergo operation had a mortality rate of 4.1% per year compared with 34.0% in those with Class III and IV symptoms. Moreover, when stratified according to EF, patients with an EF <60% had markedly lower 10-year survival compared with those with an EF ≥60% [9].
Therefore, longitudinal follow-up is necessary in patients with mitral regurgitation and the timing of surgical intervention is critical. Early intervention in primary severe MR can result in positive long-term outcomes. To determine accurately severe MR from lesser degrees of MR is the crucial clinical issue. Many clinical trials and publications support the use of more than one imaging modality to quantify the regurgitant volume accurately in order to manage MR.
In this review, we hope to address novel imaging modalities currently being used to assess this challenging task!
Transthoracic echocardiography (TTE)
The current ACC/AHA guidelines [2] state that the “gold standard” for assessment of valvular heart disease is TTE. Transoesophageal echocardiography (TEE) has excellent spatial resolution for leaflet morphology and mobility. However, the quantitative methods for assessment of MR severity, such as flow convergence-based EROA and regurgitant volume, pulse Doppler-based regurgitant volume, and the vena contracta, have some important limitations [12,13]. The role of TTE is as follows: 1) to identify the aetiology of the MR; 2) to quantify the severity of the regurgitation; 3) to assess the response of the LV to the volume overload; and 4) to determine the feasibility of durable repair. If, at any step, the TTE is non-diagnostic, a transoesophageal echocardiogram is indicated [2]. It is important to obtain quantitative measurements of the severity of the MR. Regurgitant volume (RVol) and EROA can be calculated through either the proximal isovelocity surface area (PISA) or the continuity method. The PISA method estimates the EROA at peak MR velocity and extrapolates flow through this EROA for the duration of systolic flow (as determined by the MR tissue velocity integral) to calculate RVol. The PISA method does have limitations: 1) the EROA is not static throughout systole and varies as prolapse worsens dynamically throughout systole; and 2) the assumption of a hemispherical shape for PISA calculation may not be accurate with complex EROA shapes, such as with prolapse or flail, or with eccentric jets. If there is only a late systolic jet of MR, EROA will overestimate MR severity, and the RVol is more reflective of MR severity [9,14,15].
The lack of a single reproducible echocardiographic parameter for the severity of MR and the need to integrate multiple parameters, which can often be discordant, lead to difficulty in quantifying MR with accuracy and precision [16]. In the era of recommending surgery in asymptomatic patients, the accurate assessment of MR severity is imperative with the assessment of cardiac magnetic resonance imaging (MRI).
Cardiac MRI (CMR)
Cardiac MRI (CMR) is a unique tool for measuring the severity of MR and haemodynamic contributions to left ventricular volume and function. Uretsky et al [17], in a prospective multicentre trial, compared TTE to CMR in 103 patients. The data suggest that MRI is more accurate then echocardiography in assessing the severity of MR. The authors concluded by saying that MRI should be considered in patients when surgical evaluation is a consideration. CMR provides highly accurate and reproducible assessment of left and right atrial and ventricular size and function and has become the gold standard for evaluating cardiac chamber size [18]. Ventricular volumes can be indexed to body surface area and referenced to published normal ranges. Left ventricular end-diastolic and end-systolic measurements as well as ventricular function are the established parameters for intervention in MR [2]. The reproducibility of CMR measurements is ideal for following MR longitudinally.
Advantages of CMR include the naturally occurring contrast between the blood pool and the myocardium using steady-state free precession (SSFP) imaging without the use of intravenous contrast; the ability to image the whole chest, in which the plane of imaging can be chosen without limitations of body habitus; and the fact that CMR evaluation of MR does not rely on the characteristics of the mitral regurgitant jet [19]. The quantification of MR is based on determining the blood pool from the myocardium by using the technique of SSFP imaging in order to quantify left ventricular stroke volume. A second technique, phase-contrast imaging, allows quantifying left ventricular forward stroke volume. Figure 1 illustrates an example of an SSFP short-axis stack and demonstrates accurate assessment of both left ventricular and right ventricular volumes (panel A end-diastole, and panel B end-systole) and systolic function. Figure 1, panel C, demonstrates phase-contrast imaging with a flow graph. Figure 2 demonstrates long-axis SSFP with a mitral valve regurgitant jet in a patient with mitral valve prolapse of the posterior leaflet. To ensure the accuracy of the quantification of MR, high-quality SSFP and phase-contrast images need to be obtained. Phase-contrast imaging should be performed perpendicular to the ascending aorta and pulmonary artery with maximum encoding velocity values obtained to ensure accuracy.
Figure 1. Quantification of left ventricle systolic function and aortic stroke volume for assessment of MR. End-diastolic (A) and end-systolic (B) segmentation on a SAX stack in SSFP cine images, showing the LV (red) and RV (yellow) tracing to estimate the systolic function and stroke volume. C) Phase contrast images of the proximal aorta with flow curve demonstration.
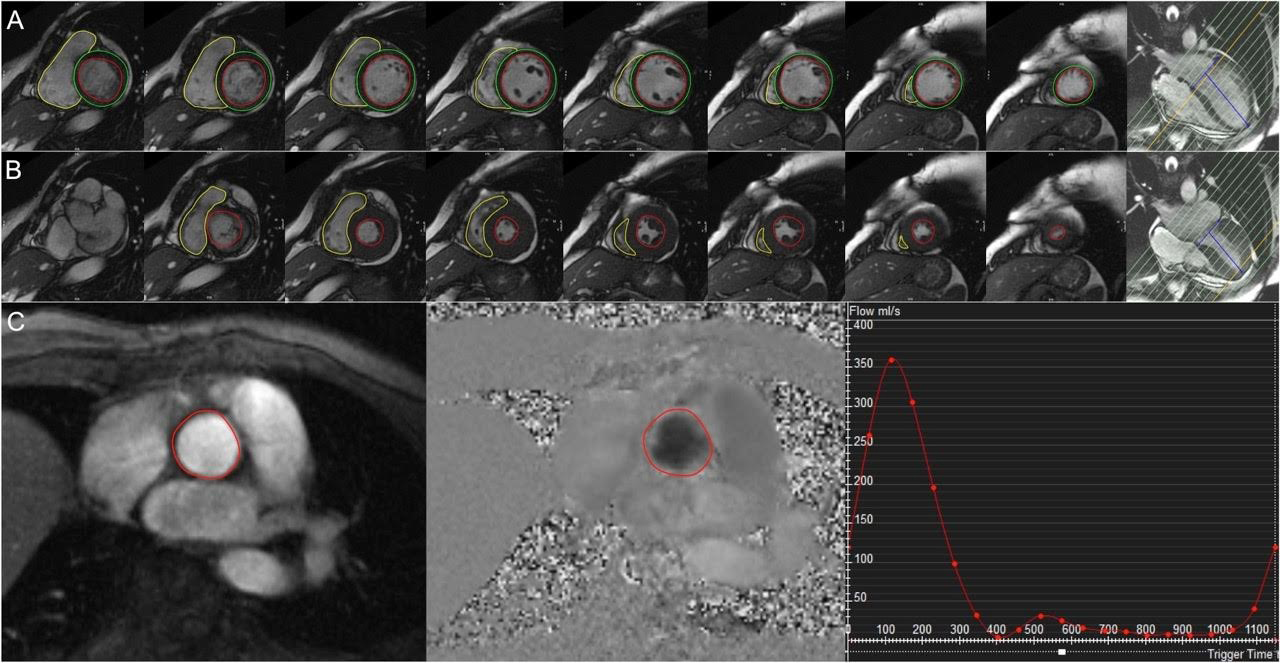
LV: left ventricle; RV: right ventricle; SAX: short-axis view; SSFP: steady-state free precession
Figure 2. Left ventricular outflow tract in 3-chamber CMR view with MVP and eccentric MR. Panels A and B: CMR SSFP cine LV outflow tract long-axis view in a patient with posterior MVP (arrowhead) and secondary mitral regurgitation with eccentric regurgitant jet (arrow).
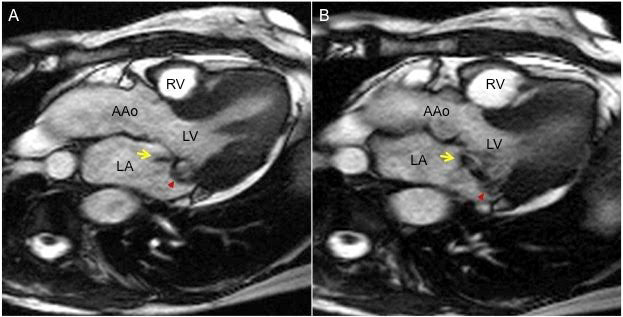
AAo: ascending aorta; LA: left atrium; LV: left ventricle; LVOT: left ventricular outflow tract; MR: mitral regurgitation; MVP: mitral valve prolapse; RV: right ventricle
Phase-contrast imaging is a velocity-encoded image which assesses “flow” through vessels, predominantly through the great vessels (ascending aorta and main pulmonary artery). This technique determines “forward flow” and is useful in assessing intracardiac shunts in order to determine a quantitative evaluation of the aortic and pulmonary flows (i.e., Qp/Qs). Phase contrast can also be applied at the level of the atrioventricular valves in order to obtain degrees of mitral and tricuspid regurgitation. This has been validated in a few studies measuring phase-contrast images and ventricular stroke volume as the reference [20]. In phase-contrast imaging, applications of gradient pulses induce phase shifts in moving protons that are directly proportional to their velocity along the direction of the gradient. Phase contrast is capable of measuring velocities, and thus flow, in the “through plane” orientation. The imaging plane is acquired perpendicular to the desired vessel. This technique allows measurement of blood flow in vessels and is particularly suited to quantifying flow in the ascending aorta and main pulmonary artery [19]. Caution should be taken with the use of phase contrast in patients with cardiac arrhythmias; acquiring the aortic and pulmonary artery phase-contrast sequences two or three times each decreases the likelihood of using erroneous data.
In a publication by Zoghbi et al [16], the method for assessing MR severity by CMR focuses on quantifying regurgitant volume and regurgitant fraction. The most studied technique is left ventricular stroke volume (LVSV) - forward stroke volume (FSV). LVSV can be quantified again by using SSFP short-axis images representing the total stroke volume (regurgitant volume + forward stroke volume). The FSV is quantified using phase-contrast images of the ascending aorta and main pulmonary artery in the absence of aortic regurgitation or intracardiac shunt [19].
In patients with lone MR, the LVSV is larger because it contains both the FSV and the mitral regurgitant volume. The mitral regurgitant volume is the difference between the LVSV and the aortopulmonary artery flow. When aortic regurgitation is present, this may be accounted for using the diastolic flow in phase-contrast imaging and subtracting the degree of aortic regurgitation. The mitral regurgitation is then calculated as LVSV – (aortic regurgitation + FSV) [19]. In patients with MR and tricuspid regurgitation, the MR is the difference between LVSV and FSV, while the tricuspid regurgitation is quantified by the difference between the RVSV and the FSV [19].
Other techniques used to assess MR include calculating the difference between the LVSV and the RVSV or the mitral inflow and the aortic flow. Both of these methods rely on the same concept as LVSV-FSV, in that LVSV and mitral inflow will contain both the mitral regurgitant volume and the FSV, and the RVSV and the aortic flow represent FSV. These calculations are valid in patients without aortic regurgitation or a cardiac shunt. In addition, regurgitant fraction can be calculated using the regurgitant volume and the LVSV [19].
Caution should be when using the aortic phase-contrast flow in patients with aortic stenosis and aortic sclerosis in whom the blood flow in the ascending aorta is non-laminar and ejected at a high velocity. In these patients, it is often better to use the pulmonary artery flow when quantifying MR [19].
Other novel techniques use semi-quantitative methods using the signal void method, size of the regurgitant jet and regurgitant orifice area by phase-contrast imaging. These are less studied and not as reproducible as quantifying stroke volume [21].
When comparing cardiac MRI to TTE, the discordance only occurs when the MR is considered severe. Several studies compared two-dimensional (2D)-TTE flow convergence-derived and Doppler-derived regurgitant volumes with CMR regurgitant volume [17,22,23]. In these studies, there was a moderate to good agreement (range of r=0.60 to 0.92) between CMR and echocardiography, with an absolute agreement ranging from 47% to 87%. When considering agreement among patients diagnosed with severe MR by either modality, the agreement worsened, with a range of 26% to 66%. Almost the same held true for 2D-TEE. When comparing 2D-TEE-derived regurgitant volumes to CMR, studies found a moderate absolute agreement between TEE and CMR (66% and 70%) with poor agreement among patients diagnosed with severe MR [24,25]. In a prospective multicentre study, Uretsky et al [17] reported excellent reproducibility of CMR that was superior to that of echocardiography (CMR intraclass correlation coefficient [ICC]: 0.9; echocardiography ICC: 0.65).
In a recent publication by Myerson et al [26], CMR quantification accurately identified patients who progressed to symptoms or other indications for surgery: 91% of subjects with regurgitant volume ≤55 mL survived to five years without surgery compared with only 21% with regurgitant volume >55 mL (p<0.0001). A similar separation was observed for regurgitant fraction ≤40% and >40%. CMR-derived end-diastolic volume index showed a weaker association with outcome (proportions surviving without surgery at five years, 90% for left ventricular end-diastolic volume index <100 mL/m2 versus 48% for ≥100 mL/m2) and added little to the discriminatory power of regurgitant fraction/volume alone.
We conclude that CMR is a reproducible technique with low interobserver variability compared to 2D-TTE and 2D-TEE for quantifying the degree of MR severity. CMR should be the preferred imaging modality when referring patients to mitral valve surgery.
Late gadolinium enhancement (LGE) in CMR
Cardiac MRI with late gadolinium enhancement imaging (LGE CMR) is a well-established technique to assess infiltrative or inflammatory myocardial disease as well as myocardial scar or fibrosis. The presence of delayed gadolinium enhancement may be associated with poorer prognosis in ischaemic, non-ischaemic as well as valvular cardiomyopathies. Han et al [27] described the presence of focal myocardial fibrosis in the papillary muscles of 10 out of 16 patients (63%) with mitral valve prolapse and various degree of MR using 3D high-resolution LGE CMR. They concluded that cardiovascular MRI can identify MVP by the same echocardiographic criteria and can identify myocardial fibrosis involving the papillary muscle in MVP patients. Hyperenhancement of papillary muscles on LGE is often present in a subgroup of patients with complex ventricular arrhythmias. More recently, Van De Heyning et al [28] prospectively described 39 patients with at least moderate primary MR and LGE CMR. Among them, 12 (31%) had late contrast uptake of the LV wall. LGE CMR showed an infarct pattern in three patients, a pattern of mid-wall fibrosis in seven patients and two patients had a combined pattern. Patients with delayed enhancement on CMR had significantly higher LV diameters (LV end-systolic diameter 39±4 vs. 34±5 mm, p=0.002; LV end-diastolic diameter 57±5 vs. 50±5 mm, p=0.001) [28]. LV remodelling seems to be associated with the presence of delayed enhancement on CMR in primary MR.
Although CMR is a well-established and valuable technique for the assessment of MR quantification, it may not be cost-effective. Echocardiography remains the first-line imaging modality for assessment of valvular anatomy and longitudinal evaluation of MR.
Conclusion
Cardiac MRI, as demonstrated in this article, is an excellent imaging tool to assess MR severity with reproducible measurements in experienced medical centres. The assessment of MR relies upon the differences between left ventricular stroke volume and forward stroke volume using the standardised CMR techniques mentioned. The assessment of MR by CMR is more accurate than 2D-TTE and should be strongly considered prior to referring a patient to mitral valve surgery.















