Clinical context
Ischaemic mitral regurgitation (IMR) is a subtype of secondary mitral regurgitation (MR), which is a complication of ischaemic heart disease. Valvular involvement can be primary (organic) or secondary (functional). Primary occurs after the rupture of the mitral subvalvular apparatus in the context of an AMI. Secondary is when the valve leaflets and chordae are structurally normal and MR results from an imbalance between closing and tethering forces on the valve secondary to alterations in the left ventricle (LV) geometry [1,2]. In both cases, IMR is associated with a critical obstruction (>70%) of at least one main coronary vessel [3]. It is most commonly seen in ischaemic cardiomyopathies. The degree of annular dilatation is much less in IMR than in degenerative MR [4]. The anatomical and physiopathological mechanisms from which the IMR originates have not been fully clarified. However, it is known that the remodelling of the left ventricle (LV) in relation to severe myocardial ischaemia is the main factor that induces the lesion, together with the involvement of the papillary muscles. Therefore, its cause is an effect of the mitral valvular spatial disposition, due to the involvement of the LV or because of an intrinsic effect on it by coronary ischaemic heart disease. The papillary muscle displacement that creates greater tension of the leaflets is posterolateral-apical, which explains why an inferiorly located AMI can produce a significant IMR, and why the incidence of it is much lower in the anterior AMI [2]. Identifying the aetiology of MR in ischaemic heart disease is not easy, since a significant percentage of patients have previously shown MR of degenerative origin [5].
Prevalence
Currently, MR is the second most common valve disease in Europe, affecting approximately 31% of the population [6]. IMR is the second most common cause of MR (25% of cases), after degenerative (60%) and ahead of rheumatic (12%). The prevalence of IMR has increased progressively in recent years. Between 17 and 40% of patients who have suffered an AMI show early clinical or echocardiographic evidence of IMR [7]. In a large percentage of auscultations, early murmurs are heard after an AMI, often transient and disappearing at discharge [8]. IMR appears in approximately 20% of the cases and is much more likely in an inferiorly located AMI (38%) than in an anterior one (10%) [9].
Mechanisms of IMR
Echocardiography should address four elements of IMR: global and local ventricular function and remodelling, degree of mitral valve deformation, mitral valve morphology, and severity of IMR [1]. Chronic IMR, in most cases, is due to type IIIb valvular dysfunction of the Carpentier classification. The restriction of leaflet motility occurs essentially in diastole, being more frequent in patients with previous posterior infarction (asymmetric pattern). When a systolic reduction of both leaflets occurs, with incomplete coaptation, it is due to prior anterior and posterior infarction (symmetrical pattern). Less frequently, IMR is due to fibrosis and elongation of the papillary muscle (type II) [10]. Several mechanisms have been proposed to explain the occurrence of IMR. As we have already indicated, mitral tenting is directly determined by apical and posterior papillary muscle displacement. Although the majority of patients present with remote infarction and ventricular remodelling with leaflet tethering, acute ischaemia with regional wall motion abnormalities can lead to similar findings of leaflet tethering in selected patients [4]. Therefore, despite other contributing factors, the fundamental factor is the adverse ventricular remodelling that occurs after an AMI, which displaces the papillae producing “tension” of the cords, which restricts the movement of the leaflets and causes incomplete mitral closure [1].
Clinic
Patients with chronic IMR are often asymptomatic. The onset of symptoms is usually related to the causative disease and the degree of ventricular dysfunction. Given its dynamic nature, IMR can be transient, appearing and/or worsening in severity coinciding with episodes of ischaemia. In patients with acute IMR due to rupture of the papillary muscle, the IMR murmur may be inaudible. It is estimated that the existence of a pansystolic murmur characteristic of IMR, which is better heard at the apex and tends to radiate towards the axilla, is present in 4-50% of patients [8]. In the same way, the intensity of this murmur, unlike that which occurs in organic MR, correlates poorly with the degree of severity. Echocardiography of the IMR provides diagnostic and prognostic data, stratifying the risk of these patients.
Echocardiographic evaluation of IMR
Echocardiography detects mitral valve abnormalities (leaflets, subvalvular apparatus, mitral annulus and/or LV) that cause valvular regurgitation [1].
Ventricular remodelling and deformation of the mitral system
The diameters of the LV, the volume of the LV by two-dimensional (2D) biplanar imaging, or more accurately with three-dimensional (3D) imaging, and the sphericity index of the LV must be determined. The extent and location of the segmental alterations and the parietal thinning of the LV, as well as the posterior and apical displacement of the posterior papillary muscle and the distance between the papillary muscles should also be assessed. As for the deformation of the mitral apparatus, the most commonly used parameters are the size of the ring, the distance of coaptation, the angles of the leaflets and the area of tenting. The measurements are obtained in parasternal long-axis view in mesosystole. 3D echocardiography allows us to assess the volume of tenting, which seems to provide advantages over 2D.
Morphology of the mitral valve
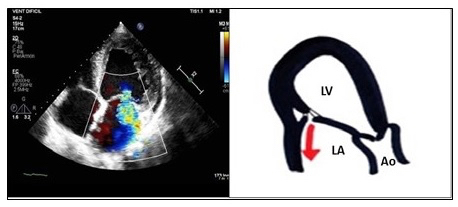
In the asymmetric closure pattern of IMR, a “hockey stick” or seagull sign is shown on the echocardiogram. The anterior leaflet in systole is below the posterior, which is also stressed, altering the coaptation. An eccentric jet of insufficiency appears, ipsilateral to the posterior leaflet, which goes to the posterior region of the left atrium (LA) (Figure 1). This pattern is typical of inferior or inferolateral infarction.
Figure 1. An apical four-chamber view, showing ischaemic mitral regurgitation with asymmetric closure: the anterior leaflet in systole is below the posterior, also stressed, altering the coaptation. The insufficiency jet is eccentric, ipsilateral to the posterior leaflet and is directed towards the posterior region of the left atrium. Echocardiographic image on the left and schematic drawing on the right.
Ao: aorta; LA: left atrium; LV: left ventricle
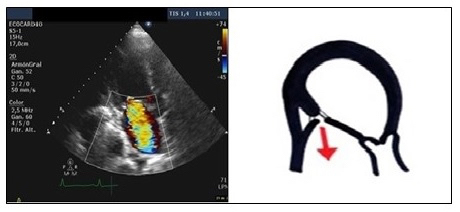
The symmetric closure is due to a global remodelling of the LV, with a spheroidal shape and greater dysfunction. There is an apical displacement of both leaflets and the coaptation point, with greater dilation and flattening of the mitral annulus. The area and volume of tenting are greater than in the asymmetric pattern, being the origin and direction of the central regurgitation jet, by a symmetrical effect on both leaflets. It is associated more with anterior infarction or multiple infarcts (Figure 2).
Figure 2. An apical three-chamber view, showing ischaemic mitral regurgitation with symmetrical closure: this is due to a global remodelling of the left ventricle, with apical displacement of both leaflets and the coaptation point. The insufficiency jet is central, due to a symmetrical effect on both leaflets. Echocardiographic image on the left and schematic drawing on the right.
Ao: aorta; LA: left atrium; LV: left ventricle
Quantification of the severity of IMR
Transthoracic echocardiography (TTE) is an excellent method for assessing the mechanism and severity of IMR, although with some limitations. The following methods are used [1].
Colour flow imaging
This is the most used and simplest method in the evaluation of IMR. It assumes that the greater the severity of MR, the greater the size and extension of the jet within the LA. However, it is imprecise, because the relationship between the extension of the jet and the severity of regurgitation is not direct, depending on many technical and haemodynamic factors. Thus, the interaction with a wall or valvular structure conditions its area, underestimating it (Coanda effect). While central flows drag flux in their path producing overestimation, a large eccentric flow that is distributed through the posterior wall of the LA goes in favour of severe IMR. Conversely, small flows that appear just behind the mitral leaflets indicate slight insufficiencies.
Limitations
This method alone is not recommended to quantify the severity of the IMR; it should only be used to detect it. When more than just a small IMR central jet is observed, a more quantitative assessment is required.
Vena contracta width
The vena contracta (VC) is the area of the jet as it leaves the regurgitant orifice; it thus reflects the regurgitant orifice area. The VC is typically imaged in a view perpendicular to the commissural line. Whenever possible, it is recommended to take an averaging of measurements taken over at least two to three beats and using two orthogonal planes. A VC width <3 mm indicates mild MR and a width ≥7 mm defines it as severe. In the case of IMR, the regurgitant orifice does not seem to be circular, but rather more extended along the coaptation line. Furthermore, the Doppler image does not give an appropriate orientation of the 2D planes to obtain an accurate cross-sectional view of the VC. An average 8 mm VC width in 2D has been reported as severe MR of any aetiology, including IMR. The VC seems to be less influenced by the load conditions of the LV and therefore be more reproducible than the flow-imaging colour methods.
Limitations
Intermediate VC values (3-7 mm) require confirmation by quantitative methods. Many times, VC is obtained in eccentric jets. In case of multiple jets, the respective values of VC are not additive. The assessment of VC by 3D echocardiography is still reserved for research.
Doppler volumetric method
This is a method used when the proximal isovelocity surface area (PISA) and the VC are not accurately applicable. The MR volume is obtained by calculating the difference between total stroke volume (product of the mitral ring area by the velocity-time integral [VTI] of the LV input tract flow) and the systemic stroke volume (product of the LV outflow tract area by the LV outflow tract VTI).
Limitations
This is time-consuming so it is not recommended as a first-line method in the quantification of MR. Its calculation is inaccurate in the presence of significant aortic regurgitation.
The flow convergence method
This is the most recommended quantitative method. The following is recommended: obtain a four-chamber apical view to determine the PISA, then align the flow with the ultrasound beam, adjust the gain and lower the wall filter, decrease the depth and reduce the sector size to increase the spatiotemporal resolution. Decrease the aliasing speed immediately, creating a longer PISA, moving the baseline in the direction of the MR flow, up to a speed of 20-40 cm/s. Measure the PISA radius in mesosystole, with the morphology of the flow as close to a hemisphere, in the first aliasing. Determine the VTI and peak flow velocity of MR with continuous Doppler. The effective regurgitant orifice area (EROA) is thus determined. This allows integrating the different severity indices, classifying MR into mild, moderate or severe (Table 1) [1]. The primary MR is considered severe if the EROA is ≥40 mm2 and the regurgitant volume (R Vol) ≥60 mL. In secondary MR, the severity threshold is lower, 20 mm2 and 30 mL, respectively, indicating a subgroup of patients with an increased risk of cardiovascular events. EROA is the most robust parameter to determine the severity of the MR, being able to determine the PISA with both central and eccentric MR.
Table 1. Quantification of ischaemic mitral valve regurgitation severity. [1] Reproduced by permission of Oxford University Press on behalf of the European Society of Cardiology. Please visit: https://academic.oup.com/ehjcimaging/article/14/7/611/2465068
|
Parameters |
Type |
Mild |
Moderate |
Severe |
|---|---|---|---|---|
|
MV morphology |
Qualitative |
Normal/abnormal |
Normal/abnormal |
Flail leaflet/ruptured PMs |
|
Colour flow MR jet |
Qualitative |
Small, central |
Intermediate |
Large central jet or eccentric jet reaching the posterior wall of the LA |
|
Flow convergence zone |
Qualitative |
No or small |
Intermediate |
Large |
|
CW signal of MR jet |
Qualitative |
Faint/parabolic |
Dense/parabolic |
Dense/triangular |
|
VC width (mm) |
Semi-quantitative |
<3 |
Intermediate |
≥7 (>8 for biplane) |
|
Pulmonary vein flow |
Semi-quantitative |
Systolic dominance |
Systolic blunting |
Systolic flow reversal |
|
Mitral inflow |
Semi-quantitative |
A-wave dominant |
Variable |
E-wave dominant (1.5 m/s) |
|
TVI mitral /TVI aortic |
Semi-quantitative |
<1 |
Intermediate |
>1.4 |
|
EROA (mm2) |
Quantitative |
c |
20–29; 30–39* |
≥40 |
|
R Vol (mL) |
Quantitative |
<30 |
30–44; 45–59* |
≥60 |
*Grading of severity of organic MR classifies regurgitation as mild, moderate, or severe, and subclassifies the moderate regurgitation group into “mild-to-moderate” (EROA of 20 to 29 mm or an R Vol of 30 to 44 mL) and “moderate-to-severe” (EROA of 30-39 m2 or an R Vol of 45-59 mL).
CW: continuous wave; LA: left atrium; EROA: effective regurgitant orifice area; LV: left ventricle; MR: mitral regurgitation; R Vol: regurgitant volume; VC: vena contracta
Limitations
In IMR there is a dynamic variation of the regurgitant orifice, with early and late systolic peaks and mesosystolic descent. Non-hemispheric PISA derived from eccentric jets, multiple or regurgitant or complex elliptical orifices may not be valid. The degree of MR could be underestimated, so a lower threshold is used in determining the severity of the functional MR.
Anterograde velocity of mitral inflow
In the absence of mitral stenosis, a peak velocity E >1.5 m/s suggests severe MR, whereas a dominant A-wave (atrial contraction) excludes it. This is applicable in patients over 50 years of age. The VTI ratio, between the mitral inflow Doppler and the aortic flow at the level of the rings in a four-chamber view, is an additional strong parameter in the assessment of MR severity. A ratio of 1.4 suggests severe MR.
Pulmonary venous flow
When MR severity increases, there is a decrease in the S-wave velocity in the pulmonary vein flow determined by pulsed Doppler, which is a sensitive but not very specific parameter of severity, since it can also appear in atrial fibrillation, ventricular dysfunction and increased LA pressure. In the most severe forms, the S-wave can be reversed, which is a specific parameter of severe MR.
Continuous wave Doppler of MR jet
Speed itself is not a parameter of severe MR. However, the intensity of the signal - dense, dashed (“notched”), triangular and with an early peak speed (“blunt”) in its morphology - indicates greater severity. All of this indicates elevated LA pressure or a prominent regurgitant pressure wave in the LA due to severe MR. In the eccentric MR it can be difficult to obtain a complete record, although the intensity of the signal is dense. The continuous wave Doppler of an MR jet is a qualitative parameter of MR severity.
Exercise stress echocardiography
IMR is a dynamic valvulopathy. Probably many patients show episodes of worsening dyspnoea and orthopnoea in relation to an increase in R Vol and EROA [5]. The European guidelines recommend the use of exercise stress echocardiography (ESE) to quantify the changes induced by exercise in MR, pulmonary arterial pressure and ventricular function. It is especially useful when there is a discrepancy between the symptoms and severity of valve disease [6]. In patients with asymptomatic IMR, ESE can identify patients with symptoms and subclinical ischaemic ventricular dysfunction. In symptomatic patients it can help to quantify the symptoms objectively, confirm or rule out the ischaemic aetiology and evaluate the myocardial viability to determine the most appropriate treatment [11]. It also has prognostic value, given that an increase in the EROA ≥13 mm2 with exercise is associated with greater morbidity and mortality and major cardiac events. An increase in the transtricuspid pressure gradient of exercise is associated with an increased risk of heart failure and death [5].
Gentry et al established a series of high-risk criteria in relation to the findings in the ESE based on the MR classification (moderate or severe, primary or secondary) (Table 2) [12].
Table 2. Mitral regurgitation and abnormal exercise stress echocardiography responses.
| Intensity |
Symptoms |
|---|---|
|
Severe MR |
Asymptomatic, primary - Development of symptomsa. - Exercise capacity <85% of predicted for age/gendera. - Increase in RVSP >60 mmHg with exerciseb. - Latent left ventricular dysfunction. - Onset of atrial fibrillation. - Abnormal heart rate recovery. Asymptomatic, secondary - RWMA consistent with ischaemic territory. - Development of acute pulmonary oedema without obvious cause. - Effective regurgitant orifice area increase >13. |
|
Moderate MR |
- Symptomatic. - Increase to severe MR. |
a Indication for mitral valve surgery.
b European Society of Cardiology indication for mitral valve surgery if high likelihood of durable repair and low surgical risk.
RVSP: right ventricular systolic pressure; RWMA: regional wall motion abnormality
Strain echocardiography
The role of the evaluation techniques of ventricular deformation, tissue Doppler and speckle tracking in the evaluation of valvular diseases is still under study. Longitudinal strain could be useful for the detection of subclinical LV contractility dysfunction [6]. The deterioration of ventricular function in patients with severe chronic MR can go unnoticed by traditional 2D echocardiography techniques, due to the loading conditions of the LV. The low afterload of these patients allows normal or even increased systolic function indices [13]. The identification of early contractile dysfunction and its subsequent surgical correction could prevent the development of irreversible ventricular dysfunction in the postoperative period that would worsen the short- and long-term prognosis [14]. In addition, speckle tracking analysis was shown to be superior to tissue Doppler analysis and traditional methods of LV systolic function analysis [15]. However, its use is limited by the heterogeneity of the algorithms used in different echocardiographic systems.
Transoesophageal echocardiography
Transoesophageal echocardiography (TOE) is especially useful when the quality of TTE is not optimal, since it allows a detailed evaluation of the morphology of the mitral valve and subvalvular apparatus. In 2D TOE, the diameter of the mitral annulus can be quantified, as can the height and increase of the tenting area, as well as the traction and decrease of the apposition surface [2]. Three-dimensional TOE has been shown to be superior to 2D TOE in the measurement of the area of the VC, being useful in organic and functional MR, even with several regurgitation jets [13]. It allows automatic measurement of the PISA area, avoiding geometric assumptions, and more accurate calculation of the R Vol and EROA. On the other hand, 3D TOE performs a direct planimetry of the anatomical regurgitant orifice in an easy and reproducible way [11]. In this way, both 2D and 3D TOE provide additional information in order to select the appropriate treatment strategy.
Prognosis
IMR has a great impact on the survival and development of post-AMI heart failure. Its existence is associated with a higher mortality compared to those patients who do not develop MR, being directly related to its severity [6]. Bursi et al showed a survival decrease in patients with IMR, being 40% in moderate-severe IMR, 62% in mild and 84% in patients without IMR [3]. Tcheng et al found that mortality one year after an AMI was 11% in patients without IMR, 22% in mild IMR and 52% with moderate-severe IMR [7]. Grigioni et al demonstrated that patients with an EROA ≥20 mm2 had lower survival at five years than those without MR (38±5% vs. 61±6%, p<0.001), regardless of ventricular function [8]. This group also demonstrated that the existence of IMR independently increased the risk of suffering heart failure by 3.6 times [8]. A more dramatic situation is acute primary IMR, with a mortality of 75% at 24 hours and 95% in the first 48 hours [9].
Conclusion
IMR is a frequent complication after AMI, the prevalence of which has been increasing in recent years with important prognostic implications. It is a complex and dynamic entity, where ventricular remodelling is the main inducer of the injury. Echocardiography plays a key role in the evaluation of these patients. It provides information about the mechanisms involved in its development and constitutes an excellent method for assessing the degree of severity of MR. Currently, new echocardiographic techniques are available that can provide additional information; their role in the study of IMR remains to be defined. For this reason, it is essential to carry out a complete echocardiographic study in all these patients to establish the diagnosis, the mechanism involved in its aetiology, as well as the degree of severity of the lesion. All of this will allow us to carry out a more comprehensive approach, stratifying the risk and planning the best therapeutic strategy in each case of IMR.