Keywords
calcification, mitral annulus, degenerative, rheumatic, congenital mitral stenosis
Background
Mitral stenosis (MS) is characterised by a decrease in mitral valve (MV) orifice area leading to compromised left ventricular filling. The consequence is stagnation of blood proximal to the MV that results in elevated left atrial, pulmonary venous, and pulmonary artery pressures [1, 2]. Mitral stenosis most commonly occurs because of rheumatic fever or degenerative MV disease. Although rheumatic fever remains the predominant cause of MS worldwide, it has been largely replaced by degenerative MS in the developed countries. Historically, the diagnosis of MS was made based on clinical examination findings and, because most symptoms generally occur in later stages of the disease, the diagnosis was made late in the clinical course leading to increased morbidity and mortality. However, since the advent of echocardiography and other diagnostic techniques, the disease is now diagnosed at relatively early stages hence allowing timely interventions and fewer complications. Improvements in catheter-based interventions and surgical techniques have also contributed greatly to the reduction in MS-related morbidity and mortality.
In this document we will briefly discuss the anatomy of the mitral apparatus followed by a discussion of the epidemiology and various aetiologies of MS, with an emphasis on changing trends in the incidence and prevalence of rheumatic and degenerative MS. Detailed discussion of clinical presentation, echocardiographic evaluation of MS and its complications and treatment are beyond the scope of this article and will be discussed in the subsequent articles on this topic.
Mitral valve anatomy
The mitral valve (MV) apparatus is comprised of the mitral valve annulus, anterior and posterior MV leaflets, chordae, and anteromedial and posterolateral papillary muscles. It is the most complex of the cardiac valves and is commonly affected by disease. Recent advances in imaging (cardiac magnetic resonance imaging, computed tomography and 3D and strain echocardiography) have shed light on its complex structure and function.
The anterior and posterior leaflets have roughly the same area. However, they differ significantly in shape and annular attachment. The anterior mitral leaflet is a tongue-like structure and has a length to width ratio of roughly one. The posterior leaflet on the other hand has a semi-lunar shape and has a low height to width ratio. It occupies two thirds of the annulus which reinforces its framework and makes it more conducive to surgical repair. However, it may be more susceptible to pathologies that cause fixation of the leaflet, such as mitral annular calcification (MAC) and rheumatic disease.
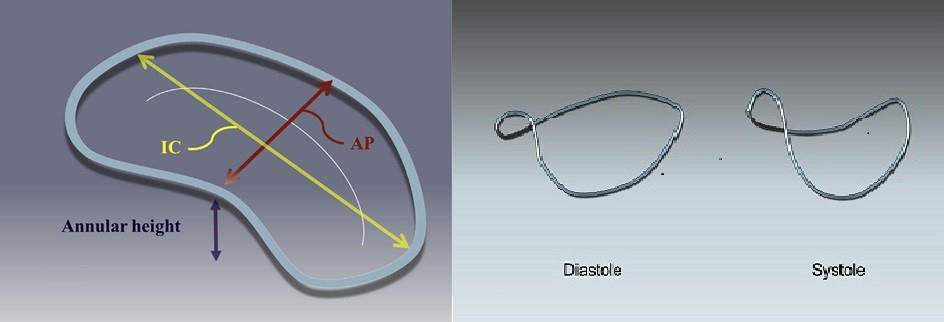
The annulus is a saddle-shaped structure which acts as a framework for attachment of the MV leaflets. It has complex mechanical properties and enables the MV to operate as an effective “one-way door” by allowing deformation along the anteroposterior diameter during each cardiac cycle (Figure 1). The mitral annulus is the site for calcific changes that lead to degenerative MS. Compared to the normal annulus, the calcified mitral annulus is larger and flatter, has an increased anteroposterior diameter, reduced saddle height and reduced contraction along the anteroposterior axis [3].
Figure 1. Schematic of the mitral annulus in diastole and systole. Note that, in systole, the saddle shape is accentuated and there is folding along the inter-commissural diameter (left). Schematic of the mitral annulus, looking down obliquely from the left atrium, illustrating its saddle shape. The high points of the mitral annulus occur anteriorly where it abuts the aortic annulus (marked “annular height”) and posteriorly. The crescent-shaped line in the middle of the Figure indicates the line of leaflet coaptation with the posterior leaflet towards the top right of the Figure and the anterior leaflet towards the bottom left (centre).
Reproduced with permission from Pressman et al [3]
The two “papillary muscles”, anteromedial and posterolateral, attach to the tips of the anterior and posterior leaflets by means of thin, frond-like avascular projections called “chordae tendineae”. One of the hallmarks of rheumatic MS is shortening and fusion of the chordal structures. This leads to restricted leaflet mobility and occasionally forms a funnel below the valve, both of which can contribute to mitral stenosis.
Epidemiology of mitral stenosis
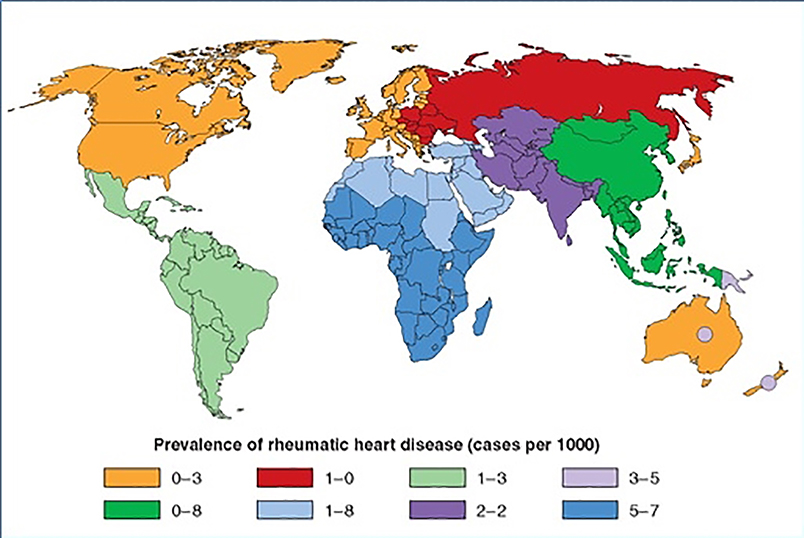
The incidence and prevalence of rheumatic heart disease (RHD) varies greatly among different age groups and regions of the world. The global prevalence of RHD is around 1 per 1,000 in children aged 5-14 years (Figure 2). However, the prevalence varies widely by region with fewer cases (0.2-0.3 per 1,000) reported from the developed than from the developing countries (5.5-5.7 per 1,000) (Figure 1) [4]. Interestingly, even with a steady global decline in its prevalence, rheumatic fever continues to be the leading cause of MV disease in the world with the majority of patients living in the developing world (79%) [5]. Once a common problem in Europe and much of the developed world, rheumatic MS now accounts for only about 10% of left-sided valve diseases [5, 6]. Nonetheless, it is often still encountered in Europe and the USA due to migration from developing countries. Failure to recognise MS not only precludes effective therapy but may result in serious complications with increased mortality and morbidity.
Relatively less is known about the true prevalence of MAC and degenerative MS. The most common reason for this is the fact that degenerative MS has until now been considered a rare cause of MS, overshadowed by interest in rheumatic MS. There have been fewer studies involving degenerative MS; most are from single centres involving small numbers of patients. Understanding its prevalence is confounded by a lack of consensus on definition and grading of MAC/degenerative MS. However, it is fair to say that, contrary to rheumatic MS, the incidence and prevalence of degenerative MS is increasing. Multiple factors have contributed to this. The improvement in life expectancy, especially in the developed world, has led to a significant increase in the geriatric population making diseases of the elderly such as degenerative MS more common in these countries. Another factor is lack of medical therapy to stabilise or reverse cardiac calcifications. Improved technology and diagnostic tools have also increased detection rates. These factors, in combination with the decreasing incidence of rheumatic MS due to improved sanitation and living standards, have made calcific MS more prevalent in the developed world [6]. Although degenerative MS is largely a disease of the elderly, it is also frequently encountered in patients with chronic kidney disease or in those who are on renal replacement therapy [6]. Here, the inciting mechanisms are thought to be abnormal calcium handling and chronic inflammation which can make the mitral annulus a nidus for pathological calcification [8, 9].
Figure 2. Prevalence of rheumatic heart disease in children aged 5-14 years.
The circles within Australia and New Zealand represent indigenous populations (and also Pacific Islanders in New Zealand).
Reproduced with permission from Carapetis et al [4]
These various aetiologies of MS have different age distributions. For example, congenital MS is a disease of the newborn and infancy, whereas rheumatic MS typically presents in the third and fourth decades of life, and degenerative MS in the seventh and eighth decades. MS appears to affect women more than men. In one study looking at 24,000 echocardiograms, rheumatic MS was approximately four times more prevalent in women than men [10]. Similarly, Pai et al reported the incidence of MAC mitral stenosis to be three times higher in women than in men in a cohort of over a thousand patients [11].
Aetiology of mitral stenosis
Rheumatic MS
Rheumatic MS is a delayed complication of acute rheumatic fever. Antibodies to streptococcal antigens cross-react with valve tissue, with damage to the valve accumulating over decades [12]. While rheumatic disease can affect any of the heart valves, it most commonly involves the mitral valve. The hallmark feature of rheumatic MS is commissural fusion which eventually leads to the classic “fish mouth” appearance of the valve orifice. Other anatomical lesions include chordal shortening and fusion, leaflet thickening and, later in the disease, superimposed calcification which may contribute to the restriction of leaflet motion. However, unlike annular involvement in degenerative MS, calcification in rheumatic MS primarily affects the leaflet tips.
Table 1. Anatomical characteristics of the different aetiological types of mitral stenosis.
Reproduced with permission from Krapfa et al [13]
| Aetiology | Commissures | Mobility | Calcification |
|---|---|---|---|
|
Rheumatic mitral stenosis Native valve Restenosis due to commissural refusion
Restenosis due to valve rigidity |
Fused At least partially fused At least one commissure completely open |
Restrictive motion of the posterior valve Restrictive motion of the posterior valve Restrictive motion of the posterior valve |
0 to +++ (Possible) 0 to +++ (Possible) 0 to +++ (Possible) |
| Degenerative mitral stenosis | Both commissures open |
Normal mobility of the tip of both leaflets |
+++ Important calcifications of the mitral annulus and the base of both leaflets |
| Post-radiation mitral stenosis | Both commissures open | Absence of restrictive motion of the posterior valve |
+ to +++ Highly suggestive calcifications of the mitral aortic membrane |
| Congenital mitral stenosis |
Not applicable (absence of commissure) |
Normal | Usually not |
Degenerative MS
MAC is frequently observed in the elderly and is associated with hypertension, atherosclerotic disease, and often aortic stenosis. Isolated calcification of the mitral annulus may have little haemodynamic importance. However, when calcification extends onto the leaflets, it can limit their mobility and produce a resting gradient across the valve. Valve thickening or calcification predominates at the base of the leaflets whereas it affects predominantly the tips in rheumatic MS. It is also important to note that, in patients with MAC, the commissures are open. This is in contrast to the rheumatic valve where commissural fusion is the norm.
The hallmark of degenerative MS is MAC. Development of MAC is a chronic process involving degenerative changes in the mitral annulus leading to its calcification. The exact mechanism of initiation and progression of MAC remains to be clearly understood although some opine that MAC may be an atherosclerotic process [14]. MAC has important prognostic and clinical implications. It has been associated with increased risk of atherosclerosis [14], coronary artery disease [15], ischaemic stroke [16], atrial fibrillation (AF) [17], conduction system disorders [18], infective endocarditis [19] and cardiovascular mortality [20].
Until recently, not much was known about the natural history of MAC. In a recent publication, Pai et al evaluated 1,004 patients with severe MAC and a transmitral gradient of ≥2 mmHg. They noted poor survival, with only 47% living five years from study enrolment [11]. In a separate study, the same group reviewed serial echocardiograms of 254 patients from the above data set and noted an increase in the mean gradient by 0.8 (+/-2.4) mmHg (range: 0-15 mmHg) per year, while stenosis grade increased by 0.18 +/-0.5 (range: 0-3) per year. The rate of progression was faster in patients with lesser degrees of stenosis and low serum albumin levels and slower in those receiving beta-blockers. Milder stenosis, diabetes mellitus and lack of beta-blocker use were independent predictors of faster DMS progression [21].
Another entity worth mentioning here is caseous MAC. It is a rare and often under-recognised variant of MAC. It has two components – a central soft core and the outer calcific shell. The soft core is comprised of calcium, cholesterol and fatty acids in a white, caseous, toothpaste-like material due to liquification necrosis. Microscopic analysis of the caseous material demonstrates amorphous eosinophils, macrophages, and lymphocytes with scattered areas of calcification and necrosis. Surrounding the “soft echolucent core” is a “hard echo-bright calcific shell”. Due to these echocardiographic findings, caseous MAC can sometimes be misinterpreted as tumour, abscess, or thrombus [22].
Congenital MS
Congenital mitral stenosis is an extremely rare condition mostly diagnosed in utero or soon after birth. The spectrum of congenital MS varies from isolated congenital MS to underdeveloped left heart structures. There are two systems of classification: anatomical, proposed by Ruckman and Van Praagh in 1978, and functional, proposed by Carpentier and Chauvaud in 1990 (Table 2) [23,24]. The clinical outcomes depend on the age at presentation, associated lesions, the degree and mechanism of MS, associated mitral regurgitation (MR) and the degree of subvalvar or papillary muscle involvement. Over the last few decades, advances in surgical techniques have led to a shift towards MV reconstruction over replacement with improved mortality and morbidity. However, unfortunately, as with most congenital surgery, the reconstruction procedure is palliative, with patients requiring further surgical intervention during the course of their lives [25,26].
Table 2. Anatomical and functional classification of congenital mitral stenosis.
Reproduced with permission from Ruckman et al [23]
| Functional classification | Anatomic/morphologic classification |
|---|---|
|
Type A (normal papillary muscles) Supravalvular ring Leaflet fusion |
Shortened chordae tendineae Parachute mitral valve Supramitral ring |
|
Type B (abnormal papillary muscles) Parachute deformity Primary papillary muscle abnormality |
Hypoplastic CMS (e.g., HLHS) Reduction in inter-chordal space and intra-papillary muscle distance |
Radiation-induced MS
Radiation-induced MV disease is a late complication of radiation to the chest. It generally presents two to three decades after radiotherapy and is related to the cumulative dose of radiation [27]. It may be difficult to differentiate radiation-induced MS from pure degenerative MS owing to some common echocardiographic findings such as the presence of annular calcification. However, the differentiation lies in the distribution of calcium. Unlike degenerative MS which mostly involves the posterior annulus, radiation-induced MS generally leads to calcification of the anterior mitral annulus [28]. Other findings specific to radiation-induced disease are involvement of other cardiac structures such as severe and progressive calcification of the aortic valve and anterior mitral leaflet, thickening of the aortomitral curtain and the pericardium, leading to constrictive cardiomyopathy in severe cases [28]. Another feature is the propensity to produce regurgitant lesions over stenotic lesions. In contrast to degenerative MS, radiation-induced MS can be easily differentiated from rheumatic MS due to absence of commissural fusion and lack of involvement of subvalvular structures [29]. A high index of suspicion and continued surveillance are key to early diagnosis and management of patients with radiation-induced valvular disease. Treatment is mostly surgical (MVR, AVR and pericardial stripping) and is often challenging, due to extensive calcification and involvement of multiple cardiac structures.
Diagnosis of MS
While auscultatory findings can identify rheumatic MS, such findings are often absent in degenerative (MAC) disease. Transthoracic echocardiography (TTE) is the single most valuable test to establish diagnosis and elucidate aetiology, severity and complications of either disease. It is invaluable in deciding the treatment approach (medical, percutaneous vs. surgical) and predicts response to therapy, and long-term morbidity and mortality. Due to its higher temporal resolution, transoesophageal echocardiography (TEE) provides excellent images of the MV and subvalvular apparatus, and has enabled us to image the entire annulus in a single frame. TEE is often utilised to perform precise 3D reconstruction of the MV and its apparatus when detailed anatomy of the valvular structure is desired for procedural planning. Cardiac computed tomography (CCT) has also emerged in recent years as a valuable tool for studying cardiac calcifications including calcific valvular lesions.
For general information on the management of valvular heart disease including MS, please refer to the “2017 ESC/EACTS Guidelines for the management of valvular heart disease” [30].