Introduction
Constrictive pericarditis (CP) is an increasingly recognised disease with various causes characterised by a fibrotic, thickened. At times, a calcified pericardium is seen with encasement of the heart impeding diastolic filling [1]. A correct diagnosis is difficult to establish on clinical grounds alone; the tentative diagnosis needs to be confirmed by non-invasive multimodality imaging including two-dimensional (2D) and Doppler echocardiography as the first-choice technique which can be supplemented by computed tomography (CT) and magnetic resonance imaging (MRI) in selected cases. Invasive haemodynamic measurements become useful when imaging does not provide adequate diagnostic information or requires further characterisation. Restrictive cardiomyopathy (RCM) is a disease with various causes that affects myocardial function either by primary myocyte dysfunction and/or by extracellular infiltration or fibrosis. Both conditions, CP and RCM, lead to diastolic heart failure with abnormal ventricular filling and similar clinical features. The accurate differentiation of CP from RCM can be a diagnostic challenge even to the experienced clinician, but is of paramount importance, since CP is a potentially curable disease, while in RCM prognosis is poor due to limited therapeutic options. However, recent advances in echocardiography and other imaging modalities have made this previously challenging task much easier.
Pathophysiology
The fibrotic shell around the heart in CP affects cardiac haemodynamics in two different ways. First, there is dissociation between intrathoracic and intracardiac pressures. Usually, LV filling pressure gradient (the difference between pulmonary capillary wedge pressure and LV diastolic pressure) remains constant during the respiratory cycle. In CP, the inspiratory reduction in intrathoracic pressure is transmitted to the extracardiac pulmonary veins, but not fully to the encased left atrium and ventricle, leading to a reduction in LV diastolic filling with inspiration. Second, since the total blood volume of all four cardiac chambers remains relatively constant, ventricular interdependence is exaggerated in CP. With the inspiratory decrease in LV filling and diastolic volume, right ventricular filling is increased in a compensatory manner. Because the superior, but not the inferior vena cava is subject to variations in intrathoracic pressure, most flow to the high-pressure right atrium during inspiration arrives from the inferior vena cava which is also assisted by increased inspiratory transabdominal pressure. This physiologically explains the paradoxical rise in jugular venous pressure on inspiration (Kussmaul’s sign). With expiration, opposite changes occur in right and left heart filling [2]. In contrast, pericardial compliance is normal in RCM and the respiratory variation in intrathoracic pressures is transmitted normally to the cardiac chambers. With inspiration, pulmonary capillary wedge pressure and LV diastolic pressure are lowered equally, thereby leaving the pressure gradient for LV filling nearly unchanged.
Ventricular interdependence
Hatle et al [3] provided insight into the dynamic respiratory changes in ventricular filling and pressures that occur in patients with CP. The concept of ventricular interdependence and the reciprocal respiratory pressure changes in the RV and LV at cardiac catheterisation constitute a useful diagnostic parameter. In patients with CP, there is usually an increase in RV systolic pressure during peak inspiration, a time when LV systolic pressure is lowest. In contrast, there is a concordant decrease in RV and LV systolic pressures during peak inspiration in patients with RCM. Ventricular interdependence in CP can also be evaluated by Doppler echocardiography with the tricuspid regurgitation velocity curve [4]. During inspiration, RV systolic pressure increases, as does the duration of RV systole because more time is required to eject an increased RV volume.
Two-dimensional echocardiography
Normal pericardial thickness is 2 mm or less. A rigid and/or thickened pericardium is the anatomic substrate responsible for the constrictive physiology. Despite isolated reports of the utility of M-mode and 2D echocardiography in detecting thickened pericardium, the reliability of transthoracic echocardiography for this purpose is questionable due to technical limitations, such as transducer position, gain, greyscale settings, and reverberations. In addition, the CP may be predominantly localised to one region of the heart. The superior resolution achieved with transoesophageal echocardiography allows better pericardial definition [5]. MRI and CT also enable accurate measurements of pericardial thickness [6]. However, anatomical information does not necessarily reflect the pathophysiological abnormalities. Moreover, CP and thickened pericardium are not uniformly associated, because patients can have surgically proven CP despite normal pericardial thickness [7]. Conversely, thickened pericardium may be present without constrictive features, especially in patients who have had thoracic radiation therapy or open heart surgery.
Myocardial systolic function as assessed by LV ejection fraction is preserved in CP. Respirophasic interventricular septal motion seen on both M-mode and 2D echocardiography is induced by abrupt ventricular volume changes and a reflection of enhanced ventricular interdependence. With less LV filling during early inspiration, the interventricular septum moves suddenly to the left. In expiration, the LV fills better, and the septum returns to a normal position. In addition, there is frequently a discrete septal “shudder” with each beat independent of breathing due to the differential filling rates of both ventricles in diastole. Biatrial enlargement and systemic venous congestion (inferior vena cava plethora) are non-specific findings, because they are encountered in both CP and RCM.
Pulsed-wave Doppler echocardiography
Because LV diastolic pressure is elevated and virtually all LV ventricular filling occurs in early diastole, mitral E-wave velocity is increased and deceleration time shortened (usually <160 ms) with a small or absent A-wave resembling a restrictive inflow pattern which is seen in both CP as well as RCM. Hatle et al [3] first described the mitral and tricuspid Doppler flow characteristics that are used in differentiating constriction from restriction. With inspiration, the dissociation of intrathoracic and intracardiac pressures results in a decrease in the initial driving pressure for left ventricular filling. Consequently, there is a decrease in peak mitral E-wave velocity by >25% during the first beat of inspiration, as well as prolongation of the isovolumic relaxation time (usually >20%). Ventricular interdependence is responsible for reciprocal changes in the trans-tricuspid inflow pattern with an inspiratory increase in peak E-wave velocity by >40%. Reverse changes do occur with expiration in both ventricles. Other investigators reported characteristic findings for respiratory changes in the pulmonary veins and hepatic veins [8]. In simplified terms, diastolic flow to the left heart decreases with inspiration, while opposite changes are observed for the right heart. However, subsequent larger studies discovered the absence of mitral inflow respiratory variation in one third of patients with CP [8,9].
Doppler findings may be misleading in some instances. First, in patients with any irregular rhythm (e.g., atrial fibrillation), respirophasic changes may still be seen, but are easily confounded by the varying RR interval. Second, markedly elevated left atrial pressure may blunt the respiratory variation in mitral E velocity due to a persistent high-pressure gradient and venous return to the left heart. Manoeuvres that decrease preload may unmask the characteristic respiratory Doppler variation [10]. Third, considerable respiratory fluctuation in intrathoracic pressure, such as that seen in chronic obstructive pulmonary disease (COPD), may mimic the respiratory variation in mitral and tricuspid inflow velocities encountered in CP. However, E/A ratio is lower, deceleration time is more prolonged and Doppler interrogation of the superior vena cava shows a marked increase in inspiratory systolic forward flow, which is not seen in patients with CP [11].
Tissue Doppler and myocardial deformation imaging
Baseline 2D echocardiography often shows a hyperdynamic mitral annulus with exaggerated motion in patients with CP [12]. This phenomenon may be recognised with the naked eye on greyscale images, but is better appreciated by tissue Doppler imaging. In general, a mitral annular e’ velocity ³8 cm/s represents a discrete amplitude cut point to distinguish CP from RCM, possibly due to a greater contribution by the longitudinal movement of the left ventricle for diastolic filling and normal LV relaxation [13,14]. Also, due to the tethering of the adjacent fibrotic and scarred pericardium, which influences the lateral mitral annular translocation in patients with CP, the lateral e’ velocity is lower than the medial e’ velocity, a phenomenon termed annulus reversus [15], which is present in up to 75% of surgically proven CP [16].
For the same reason, the marked epicardial dysfunction in CP leads to impairment of circumferential shortening (also referred to as strain), and twist mechanics, whereas the subendocardial myocardial deformation (longitudinal strain) is well preserved in CP, but significantly reduced in RCM, predominantly affecting subendocardial fibres oriented in a longitudinal direction [17]. These two distinct patterns in longitudinal and circumferential LV mechanics are readily assessable by 2D speckle tracking, a relatively angle-independent technique that tracks unique intramyocardial features in greyscale B-mode images, referred to as speckles.
There is an inverse relation between the ratio of early transmitral to annular velocities (E/e’) and LV filling pressures (annulus paradoxus and E/e’ ratio should not be used to estimate LV filling pressures in patients with CP). The plausible explanation for this finding is the exaggerated longitudinal motion of the mitral annulus, despite high filling pressures [18]. As a secondary measure, colour M-mode flow propagation of LV filling may aid in the differential diagnosis between CP and RCM. The inflow velocity of the first aliasing is usually normal or markedly increased (usually >100 cm/s) in CP, but significantly lower in RCM [13].
Atrial fibrillation is a complication of both CP and RCM and makes the evaluation of dynamic respiratory changes by Doppler echocardiography challenging. Mitral flow velocity variation is related more to cardiac cycle length than to respiratory phase, but in the hepatic veins the diastolic flow reversals stay prominent during expiration [8,19]. Mitral annular velocities measured by tissue Doppler also remain a reliable parameter [19].
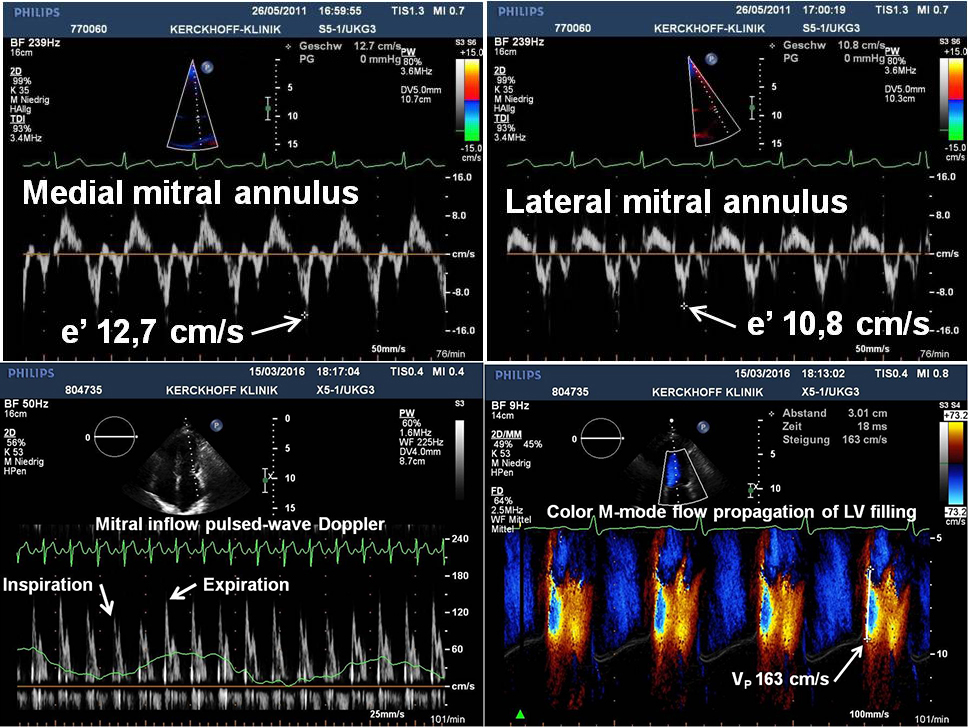
Recently, a multifaceted algorithm with five key echocardiographic findings, including respiration-related ventricular septal motion, mitral inflow pattern, medial (septal) mitral annular e’ velocity, and hepatic vein expiratory diastolic flow reversal has been proposed that is also applicable to patients in atrial fibrillation [19]. Key echocardiographic features are listed in Table 1 and typical Doppler findings are displayed in Figure 1.
Table 1. Key echocardiographic features of constrictive pericarditis.
| Key echocardiographic features of constrictive pericarditis |
|---|
|
|
|
|
|
|
|
Figure 1. Typical Doppler findings from a patient with surgically proven constrictive pericarditis. Medial (upper left) and lateral (upper right) mitral annulus early diastolic (e’) velocities by tissue Doppler show a preserved longitudinal function and reversal of the usual relationship (so-called annulus reversus). Pulsed-wave Doppler spectrum of mitral inflow velocities (lower left) demonstrates a marked respiratory variation of the peak E-wave velocity. Colour Doppler M-mode flow propagation of left ventricular (LV) filling (lower right) illustrates a steep slope (163 cm/s) of the first aliasing velocity contour (white line).
Diagnostic uncertainties: mixed constriction and restriction
After thoracic radiation therapy, CP, RCM, valvular disease, premature coronary artery disease, or a combination of them may develop. These overlapping features represent another challenge in the differential diagnosis between CP and RCM and make it necessary to determine whether abnormalities are caused by pericardial restraint, myocardial restriction, or both. If concomitant pericardial and myocardial disease is present, the decision to proceed with pericardiectomy depends on the degree to which the abnormal pericardium contributes to the increased intracardiac pressures.
Future directions
The currently available cardiac imaging techniques have the capability to generate a vast amount of cardiac structural and functional data, of which only a fraction is used by the interpreting clinician for establishing a diagnosis and clinical decision making. A potential solution to meet this challenge is to apply a cognitive machine-learning approach to aid in the differentiation of CP from RCM [20].
Conclusions
CP is characterised by the encasement of the heart by a rigid non-pliable pericardium resulting in impairment of diastolic filling. An understanding of the pathophysiological abnormalities characterised by dissociation between intrathoracic and intracardiac pressures and an exaggerated ventricular interdependence is pivotal to the accurate diagnosis and differentiation from RCM. Echocardiography would be considered the first-line diagnostic modality and respiration-related ventricular septal shift a highly sensitive starting point. A preserved or even accelerated mitral annular motion in a patient with heart failure symptoms as well as reversal of the relationship between lateral to medial annular tissue Doppler velocities (also called annulus reversus) should alert the interpreting clinician to the diagnosis of CP. Conventional pulsed-wave Doppler of early diastolic peak mitral flow velocity often demonstrates marked inspiratory decrease. Although these Doppler findings are usually diagnostic, both false-positive and false-negative results exist, and no single echocardiographic parameter should be used exclusively in favour of a multifaceted approach. In addition, multimodality imaging with CT and CMR can help to delineate the thickness of the pericardium, although they do not prove physiologic significance, and increased pericardial thickness is not an essential diagnostic feature of CP. When a comprehensive transthoracic echocardiographic study is diagnostic for constriction, no further diagnostic testing should be necessary. In equivocal cases, where non-invasive evaluation is inconclusive or discordant with clinical findings, haemodynamic assessment by cardiac catheterisation should be performed.



 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.