Keywords
angina pectoris, coronary artery disease, diagnosis, prognosis, stress echocardiography
Introduction
Chest pain is the main alert sign for coronary artery disease (CAD). The important thing is to define it as angina and then study its possible mechanism, but first CAD must be ruled out because it has a high mortality risk. From a clinical perspective, angina is an important symptom that is difficult to interpret, and a complex variable from a statistical point of view. Eighty-one percent of men and 52% of women with angina have significant CAD [1]. Three-vessel lesions (28%) are the most frequent significant CAD in males and one-vessel lesions (17%) in females [1]; therefore, stratifying the risk in these patients is very important. Cardiac stress imaging is a well-established method for the evaluation of CAD and predicting outcomes [2,3].
Indications for stress echocardiography in patients with angina or the ischaemic equivalent
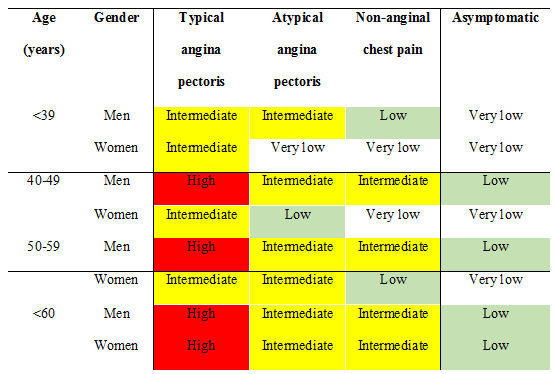
Once the physician determines that symptoms are present that may represent CAD, the pre-test probability of CAD should be assessed [4]. There are a number of risk algorithms [5] available that can be used to calculate this probability: very low pre-test probability (<5% pre-test probability of CAD), low pre-test probability (between 5% and 10% pre-test probability of CAD), intermediate pre-test probability (between 10% and 90% pre-test probability of CAD), and high pre-test-probability (>90% pre-test probability of CAD) (Figure 1) [4].
Figure 1. Pre-test probability of CAD by age, gender and symptoms.
High: >90% pre-test probability. Intermediate: between 10% and 90% pre-test probability. Low: between 5% and 10% pre-test probability. Very low: <5% pre-test probability.
From Douglas et al [4]. Appropriate use criteria for echocardiography. With permission from Elsevier.
Moreover, we have to determine the appropriate use of the test. There are three categories of indication: appropriate use, uncertain use, and inappropriate use [6].
Appropriate test for specific indication: test is generally acceptable and is a reasonable approach for the indication.
Uncertain for specific indication: test may be generally acceptable and may be a reasonable approach for the indication. Uncertainty also implies that more research and/or patient information is needed to classify the indication definitively.
Inappropriate test for that indication: test is not generally acceptable and is not a reasonable approach for the indication [6].
Appropriate uses are:
A) Low pre-test probability of CAD and ECG uninterpretable or unable to exercise.
B) Intermediate pre-test probability of CAD and ECG interpretable and able to exercise.
C) Intermediate pre-test probability of CAD and ECG uninterpretable or unable to exercise.
D) High pre-test probability of CAD and regardless of ECG interpretability and ability to exercise [4].
On the other hand, an imaging stress test is recommended as the initial test for diagnosing CAD if the left ventricular ejection fraction is <50% in patients without typical angina, and in symptomatic patients with prior revascularisation, and should also be considered to assess the functional severity of intermediate lesions on coronary arteriography [7].
Inappropriate use is:
Low pre-test probability of CAD and ECG interpretable and able to exercise [4].
Major absolute contraindications for a stress test are decompensated congestive heart failure, uncontrolled hypertension (blood pressure >200/110 mmHg), uncontrolled cardiac arrhythmias, acute pulmonary embolism, acute myocarditis or pericarditis, acute aortic dissection, acute myocardial infarction (<4 days) [8].
Imaging technique
Clear endocardial definition is crucial for optimal interpretation and it is recommended that harmonic imaging, when available, be routinely used for optimal endocardial border detection (in parasternal long- and short-axis, apical long-axis, and apical four- and two-chamber views). Contrast-enhanced endocardial border detection could be used when suboptimal imaging is present [9]. Imaging during exercise has been associated with improved sensitivity compared to post-treadmill exercise imaging; continuous imaging during stress permits more precise determination of the heart rate at which ischaemic wall motion abnormalities begin [9].
Rest and stress images are compared for left ventricular cavity size and shape, and global and regional contractility [10]. A normal response to stress occurs when all left ventricular segments become equally hypercontractile. Each segment can be scored at rest and with stress as follows: normal=1, hypokinetic=2, akinetic=3, dyskinetic=4, aneurysmal=5 [10]. The wall motion score index can be calculated at rest and with stress using a standard 17-segment left ventricular model by summing the total scores of each individual segment and dividing by the number of segments assessed. Single-vessel disease may manifest only as stress-induced wall motion dysfunction in one vascular territory, while multivessel disease may cause multi-segmental or even global wall motion impairment accompanied by a left ventricular ejection fraction decrease and/or end-systolic volume increase with stress. The wall motion score index at peak stress has been shown to be independently associated with cardiac events and mortality.
During the last decade, tissue Doppler imaging, strain imaging, and 3D imaging have been increasingly used for accurate evaluation of cardiac function, providing new ischaemic indicators. For these new techniques, the images are acquired at maximum or immediate post-stress, and then analysed in the workstation. The methodology of image acquisition depends on the type of echocardiographic equipment.
Specificity and sensitivity
In general, the sensitivity of exercise and the sensitivity of dobutamine SE for CAD detection has been estimated to be 88% and 85%, respectively, with a specificity of 82% and 83%, respectively [9]. Imaging during exercise has been associated with improved sensitivity compared to post-treadmill exercise imaging [10].
Recent studies have shown that more women die of heart disease every year than men. Early symptom recognition, risk assessment, and diagnosis of CAD are paramount in reducing cardiovascular morbidity and mortality in women [11]. In women at intermediate pre-test probability of disease, a non-invasive imaging-based test for ischaemia is preferred, whenever local expertise and availability permit [12]. Its versatility, accuracy, safety, non-invasiveness, and lack of radiation exposure make SE an attractive technique to apply to the assessment of women with known or suspected CAD [13]. In women, the sensitivity, specificity, positive-predictive value and negative-predictive value for SE are 79% (95% CI: 74%-83%), 83% (95% CI: 74%-89%), 78% and 83%, respectively, in women without a history of CAD [14]. The mean sensitivity and specificity of dobutamine SE to detect CAD are 72% and 88%, respectively [14]. The positive-predictive value for SE is lower in women than men, although the sensitivities and specificities are comparable [13]. The lower positive-predictive value is consistent with the lower prevalence of obstructive epicardial CAD in women.
Causes of false-negative and false-positive tests
Despite the excellent specificity of SE, we continue to see a subset of patients with false-positive tests (i.e., <50% diameter coronary artery stenosis on the subsequent angiogram) in the absence of left bundle branch morphology, right ventricular pacing, prior cardiac surgery, or abnormal wall tethering at baseline. These false-positive findings present a management challenge because it remains unclear whether and how to treat these patients [15].The mere presence of CAD is a poor gold standard for defining the false or true positivity of SE [16].
It is imperative to accomplish post-exercise imaging as soon as possible (≤1 min from cessation of exercise). This technique assumes that regional wall motion abnormalities will persist long enough into recovery to be detected. When abnormalities recover rapidly, false-negative results occur [9].
Finally, a subset of patients has microvascular abnormalities, a hypertensive response to exercise, vasomotor changes, endothelial dysfunction, and/or small vessel coronary disease that can lead to false-positive SE.
Pro/contra arguments of the test
The SE presents some advantages and limitations.
Advantages
The test is portable, non-invasive, and it is not associated with radiation exposure or contrast exposure. Rapid performance with immediate availability of results. Multistage imaging allows determination of ischaemic threshold. Since diagnostic ultrasound has no known adverse health effects, the risks are associated with the stress testing itself, not echocardiographic imaging. The cost of SE is low compared to alternative modalities [10,13].
Limitations
The primary limitation of SE is that interpretation remains subjective: this can reduce the reproducibility of SE and increase dependence on sonographer and interpreter skill and experience [10]. Dependence on image quality (imperfect feasibility) [13]. An additional problem is the “low volume” of SE examinations by a single operator in clinical practice [17].
Lower sensitivity for detection of mild CAD is not achieved or there is an inability to capture images near maximal stress. Subjectivity - requires an expert reader to interpret [13].
The intravenous injection of contrast agent improves the opacification of the myocardial border, but the analysis of myocardial perfusion remains problematic.
Conclusions
SE has developed into an important non-invasive imaging tool for the diagnosis, prognosis and follow-up of patients with angina pectoris. All imaging techniques have advantages and limitations. However, SE with exercise or dobutamine is an accurate, efficient, safe, and cost-effective non-invasive technique for the evaluation of myocardial ischaemia. SE should be carried out when the post-cycle ergometry test probability is intermediate, or the ECG is uninterpretable, and the dobutamine stress test should be carried out when an exercise test cannot be performed.