Keywords
angina pectoris; myocardial fractional flow reserve; myocardial ischaemia
Abbreviations
CAC: coronary artery calcium
CAD: coronary artery disease
CAD-RADS: coronary artery disease reporting and data system
CRESCENT: Computed Tomography vs. Exercise Testing in Suspected Coronary Artery Disease trial
CT: computed tomography
CTA: computed tomography angiography
ESC: European Society of Cardiology
FAME: Fractional Flow Reserve Versus Angiography for Multivessel Evaluation trial
FFR: fractional flow reserve
FFRCT: fractional flow reserve derived from computed tomography
MPI: myocardial perfusion imaging
MRI: magnetic resonance imaging
NPV: negative predictive value
PET: positron emission tomography
PROMISE: Prospective Multicenter Imaging Study for Evaluation of Chest Pain trial
PTP: pre-test probability
SPECT: single photon emission computed tomography
Introduction
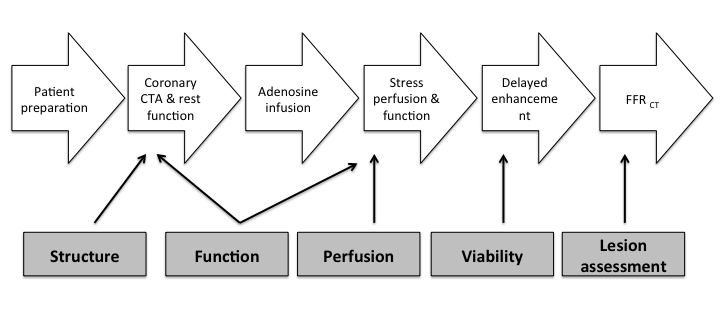
The ideal non-invasive method for the assessment of the patient with chest pain would provide information on the structure (anatomy), function (physiology), perfusion and viability of the myocardium as well as the presence and functional significance of coronary lesions (Figure 1). In addition, all of these should be available with minimal radiation exposure, at a non-prohibitive cost and, ultimately, the diagnosis or absence of CAD should be accurate. The currently available methods fulfil some, but not all, of the above criteria. Nonetheless, technological advances and hybrid techniques look promising for such a “one stop shop” diagnostic modality for chest pain in the foreseeable future.
Figure 1. Multifaceted evaluation of the coronary arteries in patients with chest pain.
CTA: computed tomography angiography; FFRCT: fractional flow reserve derived from computed tomography
Modified with permission from Williams et al [1].
Computed tomography-based modalities
Computed tomography is increasingly used to provide anatomical insights into the coronary tree. The advent of newer generations of CT scanners capable of simultaneously acquiring multiple slices (currently up to 640 slices per gantry rotation) has dramatically increased the spatial and temporal resolution of the method; as a consequence, it allows the visualisation of smaller structures, such as the coronary arteries and the content of atherosclerotic plaques, with fewer artefacts. The whole heart is scanned in less than a heartbeat and what is seen is the actual, full heart frozen at one particular time without the stitching artefacts that were evident in older scanners. Though CT-based cardiac imaging is largely anatomy-oriented, emerging evidence points to its potential to quantify perfusion and thus to provide a functional assessment of the myocardium.
Coronary artery calcium score
If no contrast agent is used, the scan will only allow quantification of the calcium burden in the coronaries. A lesion exceeding the threshold of 130 Hounsfield units that extends to at least 3 pixels is considered as coronary calcium. By multiplying the area of calcification by the maximal calcium lesion density (from 1 to 4), the coronary artery calcium (CAC) score, or “Agatston score”, is calculated; its values rise exponentially as calcifications increase. An Agatston score in excess of 400 signals the presence of heavy plaque burden. The calculated CAC is compared to those of asymptomatic people of the same age, sex and ethnic group; if it exceeds the 75% value, then the patient is considered to be at high risk for CAD [2].
According to the 2013 ESC guidelines on the management of stable coronary artery disease, coronary calcium detection by CT is not recommended to identify individuals with coronary artery stenosis (class of recommendation III, level of evidence C) [3]. Nonetheless, recent data from the multicentre, randomised CRESCENT trial have pointed to the fact that, when CAC scoring is used as part of a tiered protocol (CAC followed by computed tomography angiography [CTA] if the Agatston score is between 1 and 400), it could offer an effective and safe alternative to functional testing. Moreover, the implementation of CAC as a gatekeeper for CTA resulted in lower costs and lower exposure to radiation [4].
Advantages
- Well validated for primary prevention.
- Contrast media-free modality that can be used for the quick assessment of patients with severely impaired renal function.
- Minimum radiation exposure, comparable to mammography (<1 mSv).
- Gatekeeper to functional testing.
Disadvantages
- Not well validated for the assessment of patients with angina symptoms.
- Lack of outcome studies.
- Incidental abnormal findings not infrequent (~7.0%).
Coronary computed tomography angiography
Coronary CTA is the mainstay of CT-based modalities for the assessment of the patient with angina symptoms. Essentially, it is an anatomic reconstruction of the coronary vasculature and requires the injection of contrast medium. It provides anatomic information regarding the origin, course, vessel wall, lumen and patency of the coronary arteries, as well as the presence of atherosclerotic plaques. Advances in the spatial and temporal resolution of CT scanners have facilitated the more accurate delineation of these structures. In addition, they have negated the need for low heart rates (sinus rhythm, lower than 65 beats per minute; use of short-acting beta-blockers frequently required) and breath holding during the scan. A high coronary calcium burden (Agatston score >400) and severe obesity still pose problems to image acquisition and reconstruction and can result in uninterpretable results. Of note, image quality is heavily downgraded due to blooming artefacts if metallic stents from previous percutaneous revascularisations are in situ. In this subset of patients, coronary CTA is not recommended. The introduction of the Coronary Artery Disease Reporting and Data System (CAD-RADS) has standardised the reporting of findings: it ranges from CAD-RADS 0 for the complete absence of stenosis and plaque to CAD-RADS 5 for the presence of at least one totally occluded coronary artery.
Studies regarding the discriminatory ability of coronary CTA for CAD are consistent in reporting very high negative predictive values (in the range of 97-99%) and sensitivities (95-99%), thus solidifying its role as a rule-out modality; in practice, when no coronary stenoses are detected, the presence of CAD can be safely ruled out and no further testing is required. Rule-in metrics are markedly lower, ranging from 64-89% for specificity and 91-93% for positive predictive value. These especially hold true when image quality is optimal, in the absence of coronary calcifications and in patients with a low/intermediate PTP for CAD. Overall, coronary CTA has a diagnostic accuracy close to invasive angiography for individuals with a low PTP of CAD. Therefore, and in keeping with the 2013 ESC guidelines, coronary CTA can be an alternative to stress tests in individuals with low/intermediate PTP risk, when stress tests are contraindicated, or an additional test when the findings of a stress test are inconclusive (Class of recommendation IIb, level of evidence C) [3].
The Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) trial compared the outcomes of symptomatic patients randomised to either coronary CTA or a stress test (nuclear perfusion, stress echocardiography, or exercise ECG). The incidence of events over a median follow-up of 25 months was equally low for the two groups (3.3% for the coronary CTA group versus 3.0% for the stress test group, p=0.75). Nonetheless, the use of coronary CTA was associated with a lower incidence of invasive catheterisation, showing no obstructive CAD during the 90 days after randomisation [5]. It should be kept in mind that coronary CTA provides only anatomical insights and cannot inform on the functional significance of the detected lesions.
Advantages
- Excellent as a rule-out test in individuals with low/intermediate PTP.
- Can be part of a “triple rule-out” strategy, i.e., one scan of the thorax permits the evaluation of the pulmonary arteries, thoracic aorta and coronary arteries.
Disadvantages
- Radiation exposure.
- Contrast media required.
- Need for low heart rate and breath hold during scanning with older-generation, low temporal resolution scanners.
- Unsuitable if stents are present.
Computed tomography myocardial perfusion imaging
Computed tomography myocardial perfusion imaging (CT-MPI) provides a functional assessment of the myocardium: it uses the myocardial distribution of contrast media as a proxy of perfusion and, when combined with coronary CTA, allows a complete assessment of the coronaries with a single modality.
Following intravenous administration of a bolus of contrast media, its first pass through the myocardial tissue is assessed; hypoperfused areas appear as hypoattenuating regions. Different acquisition techniques are currently available. During a static CT-MPI exam, the myocardium is only scanned once. Therefore, the acquisition of this snapshot has to be made at the critical time point of maximum contrast concentration in the coronary arteries. To this end, the image sets obtained for coronary CTA are used, without further need for additional acquisitions (consequently less radiation). A similar snapshot can be acquired during stress conditions by administering pharmacological agents that promote vasodilation, such as adenosine, dipyridamole, regadenoson or dobutamine. Currently, static single-energy CT is the most widespread CT-MPI technique. The per-vessel sensitivity and specificity of the technique are 50-96% and 68-98%, respectively, with positive predictive value (PPV) and negative predictive value (NPV) ranges of 55-94% and 79-98% [6]. It should be emphasised that the discriminatory ability of the CT-MPI is dependent on a number of factors, including the method used (static/dynamic/dual energy), the acquisition of images at stress or not, the method against which we compare (cardiac MRI, SPECT, angiography, FFR), the per-patient or per-vessel analysis and, last but not least, on the technology of the CT scanner (number of slices, correction algorithms).
Dual energy CT-MPI techniques are emerging methods for image acquisition, where a dual-source dual-detector scanner is used. The two different X-ray sources (at low and high tube voltages) produce two data sets during the scan; these are merged and provide a more accurate distribution of the contrast media in the myocardium. The combined use of coronary CTA and dual energy CT-MPI results in improved sensitivity (91.8-93.5%) and specificity (67.7-85.5%), PPV (73.6-88.3%) and NPV (87.5-91.4%) [7].
Dynamic CT-MPI imaging refers to a novel technique where the heart is scanned multiple times, and not only once as in the static techniques. This requires newer-generation scanners with multiple detectors and high temporal resolution. Preliminary data point to sensitivity, specificity, PPV and NPV values in the range of 6-100%, 74-100%, 48-100%, and 82-100%, respectively [6]
Advantages
- For static CT-MPI, one scan allows both anatomical and functional evaluation.
- Radiation dose equivalent to contemporary nuclear medicine imaging.
Disadvantages
- Accurate timing of image acquisition during static CT-MPI exams is critical and can influence image interpretation.
- Perfusion imaging can be inaccurate in older scanners with low temporal resolution.
- High radiation exposure for dual energy and dynamic CT-MPI.
- Not widely available.
Fractional flow reserve derived from computed tomography
Fractional flow reserve (FFR) remains the standard of reference for the detection of the ischaemic potential of epicardial stenoses. FFR is the ratio of maximal, hyperaemic myocardial flow in the presence of a lesion to the normal maximal myocardial flow. This ratio of two flows can be derived from the ratio of distal (Pd) to aortic pressure (Pa) under maximal hyperaemia; these are measured invasively by using a coronary guidewire equipped with a pressure sensor, and maximal hyperaemia is achieved by administering adenosine [8,9]. On the basis of the outcomes of the Fractional Flow Reserve Versus Angiography for Multivessel Evaluation (FAME) trials, only lesions with an FFR value equal to or less than 0.80 are prognostically important and thus should be revascularised; these results were subsequently corroborated in multiple studies and meta-analyses [10-12].
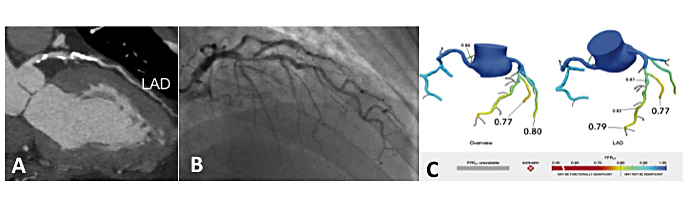
Recent advances in computational flow dynamics and image-based modelling have allowed the non-invasive calculation of FFR. The new metric, FFRCT, is calculated off-site using three-dimensional models of the coronary vasculature, which are derived from a coronary CTA scan. The computational models are capable of simulating hyperaemic conditions; therefore, there is no need to administer adenosine or other hyperaemic agents. The proprietary technique (HeartFlow®; HeartFlow, Redwood City, CA, USA) has been validated against invasively measured FFR, as well as against coronary CTA. In the NXT trial, the per-patient sensitivity and specificity (95% CI) to identify myocardial ischaemia were 86% (95% CI: 77% to 92%) and 79% (95% CI: 72% to 84%) for FFRCT [13]. Importantly, the discriminatory ability of the method is not diminished by the presence of calcium, as it performs equally well in vessels with high Agatston scores [14] (Figure 2).
Figure 2. Multimodality assessment of a left anterior descending artery.
(A) The coronary CTA demonstrates areas of hard, calcified plaque. (B) Coronary angiography shows the proximal tight coronary lesion. (C) FFRCT identifies significant disease with an FFR value of 0.79 at the distality of the vessel.
CTA: computed tomography angiography; FFR: fractional flow reserve, FFRCT: fractional flow reserve derived from computed tomography
FFRCT holds the potential to revolutionise the workup of patients with angina symptoms, offering the possibility of a complete anatomical and functional coronary evaluation without the need for catheterisation. Therapeutic decisions for patients with angina based on coronary CTA and FFRCT testing were shown to result in equivalent clinical outcomes, quality of life and lower costs compared with an invasive approach at one-year follow-up [15]. The addition of FFRCT to a coronary CTA can further refine the risk assessment of patients with angina symptomatology [16].
Advantages
- Strictly non-invasive assessment of both coronary anatomy and physiology.
- Well validated against invasive FFR, better than any other non-invasive testing.
- Simultaneous determination of FFR in all coronary vessels and segments.
- Enhanced “spatial resolution” with information on ischaemia on a per-segment basis.
Disadvantages
- Calculations are performed off-line and results are available hours/days later.
- Imaging artefacts can influence FFRCT calculations.
- Not yet validated in patients with previous CABG or PCI.
Magnetic resonance imaging-based modalities
Coronary magnetic resonance imaging angiography
At present, coronary magnetic resonance angiography (MRA) has an inferior spatial resolution and requires prolonged scan times when compared to coronary CTA. Its main uses are the imaging of aneurysmatic coronary arteries or those with an aberrant take-off; coronary artery stenoses can be reliably evaluated up to their proximal segments. Targeted or whole-heart 3D free-breathing approaches are used with gradient echo and/or steady-state free precession sequences. Nonetheless, imaging of the coronaries remains suboptimal due to coronary motion and low contrast and signal to noise ratios [17].
Advantages
- No ionising radiation.
- As part of a comprehensive MRI exam, it can detect other causes of chest pain, including inflammatory cardiac disease, pulmonary embolism and aortic dissection.
Disadvantages
- Mainly a research tool due to low spatial resolution and image quality.
Stress cardiac magnetic resonance imaging
The principle of stress imaging is that wall motion abnormalities during drug-induced stress conditions are indirect evidence of ischaemia. Cardiac MRI is the “gold standard” for the assessment of left ventricular function and myocardial viability, as this can be performed in various anatomic planes. New wall motion abnormalities (≥3 segments in the 17-segment model) induced by stress indicate a high event risk patient. Stress MRI testing is usually complemented by myocardial perfusion and late gadolinium enhancement studies during the same study and the results are considered in perspective.
Advantages
- No radiation.
- Adds complementary information as part of a comprehensive cardiac MRI exam, including myocardial perfusion and late gadolinium enhancement.
Disadvantages
- Standard MRI scanners currently examine only three slices of the left ventricle.
- ECG markers of ischaemia (e.g., ST-segment depression) are not reliably detected when in the scanner; cautious monitoring during stress is needed.
Magnetic resonance myocardial perfusion imaging
Similarly to other MPI techniques, cine imaging is performed during rest and pharmacological stress (adenosine, dipyridamole, regadenoson, dobutamine) and the ischaemic areas are those that are hypoperfused during stress. Following intravenous administration of gadolinium, its first pass perfusion of the myocardium is imaged. The advantage of the method lies in its ability for continuous acquisition of images following the infusion of the contrast agent. Reversible perfusion deficits >10% of the left ventricular myocardium imply a high risk for future events. Moreover, resting MPI (and late gadolinium enhancement) can identify regions with microvascular obstruction; this is a unique feature of the technique. Microvascular obstruction appears as a hypoenhanced area that persists for >2 min (early microvascular obstruction) and/or areas of central hypoenhancement within a hyperenhanced region in late gadolinium enhancement images (late microvascular obstruction). Both types of microvascular obstruction have an unfavourable prognosis following myocardial infarction.
Rest-stress MR MPI shows a comparable performance with other techniques for the detection of CAD (Table 1); the advent of 3T scanners may further ameliorate diagnostic performance [18].
Advantages
- No radiation exposure allows continuous imaging.
- Can detect microvascular obstruction.
Disadvantages
- Time-consuming.
- Not widely available, requires a high level of expertise from the operator and physician.
- Slow heart rate and vasodilation are prerequisites.
- Patients with non-MRI-compatible implanted devices (pacemakers, defibrillators) are excluded.
Table 1. Sensitivities and specificities of novel non-invasive modalities for diagnosing coronary artery disease.
Coronary artery calcium score
- Sensitivity: 95–99%
- Specificity: 28–66%
Coronary CT angiography
- Sensitivity: 95–99%
- Specificity: 64–86%
CT myocardial perfusion imaging
- Sensitivity: 42–94%
- Specificity: 71–98%
FFRCT
- Sensitivity: 84–90%
- Specificity: 54–79%
Coronary MR angiography
- Sensitivity: 50–98%
- Specificity: 32–100%
MRI myocardial perfusion imaging
- Sensitivity: 67–94%
- Specificity: 61–93%
PET myocardial perfusion imaging
- Sensitivity: 90–91%
- Specificity: 75–84%
CT: computed tomography; FFR: fractional flow reserve; FFRCT: fractional flow reserve derived from computed tomography; MRI: magnetic resonance imaging; PET: positron emission tomography
Positron emission tomography
Positron emission tomography (PET) imaging has a twofold role in the assessment of coronary artery disease: it quantifies myocardial blood flow (i.e., it is a perfusion modality) and, in addition, myocardial metabolism (i.e., detects viable tissue). At present, it constitutes the gold standard against which other modalities for perfusion and viability are compared.
Its use as a diagnostic tool for angina pectoris is mainly focused on myocardial blood flow quantification (mL/g per tissue mass). In a similar manner to nuclear myocardial perfusion imaging methods, a radiotracer is used; for perfusion studies Rubidium-82 (82Rb) or N-13 ammonia (13NH3) is usually used, and imaging during rest and pharmacological stress is performed. The main advantage of PET over single photon emission computed tomography (SPECT) is that two (instead of one) photons are produced when the radiotracers interact with surrounding (myocardial) tissue, therefore resulting in better spatial resolution. Moreover, PET is characterised by improved contrast resolution (contrast-to-background ratio), so milder perfusion abnormalities can be detected [19].
The quantification of absolute myocardial blood flow during rest and stress conditions facilitates the accurate calculation of coronary flow reserve (defined as the ratio of the two). Coronary flow reserve is a cumulative metric of the state of both the macrocirculation and microcirculation; both can be influenced by coronary artery disease to a different extent. As a consequence, a normal threshold for coronary flow reserve is elusive (ranging from 1.5 to 3.0 in the literature).
The assessment of myocardial metabolism, and therefore viability, capitalises on the differential use of glucose by viable and non-viable myocardial tissue. The most commonly used metabolism tracer is 18FDG (fluorodeoxyglucose), essentially a glucose molecule with a radioactive 18F atom. Uptake of 18FDG is only possible by viable myocardium, be it contracting or hibernating. Table 2 presents the possible flow-metabolism patterns for PET viability studies.
Table 2. Patterns of perfusion and glucose metabolism during 18F-fluorodeoxyglucose positron emission tomography studies.
Adapted with permission from Ghosh et al [19].
Perfusion: Preserved
- Glucose metabolism: Preserved
- Category: Viable
Perfusion: Reduced
- Glucose metabolism: Preserved
- Category: Mismatch (viable hibernation)
Perfusion: Reduced
- Glucose metabolism: Reduced
- Category: Match (non-viable)
Perfusion: Preserved
- Glucose metabolism: Reduced
- Category: Reverse mismatch (altered regional glucose metabolism)
From a practical standpoint, and due to the fact that a glucose tracer is used, patients with an impaired glucose metabolism or frank diabetes mellitus pose a challenge; strict glucose control prior to and during the exam are needed in order to assure the validity of the results.
Advantages
- Gold standard method for myocardial perfusion and viability.
- Calculated coronary flow reserve is pertinent to the state of both macrocirculation and microcirculation.
Disadvantages
- Limited availability.
- Radiation exposure.
- Elusive cut-off for coronary flow reserve.
- Special attention to diabetic patients required.
Conclusion
The newer techniques for the diagnosis and follow-up of patients with angina are based heavily on imaging modalities. Thus, their respective pros and cons are to an extent those inherent to each imaging technique. The majority of them have comparable, if not better, discriminatory ability for CAD than the traditional techniques (treadmill stress test, stress echocardiography and SPECT-MPI), and provide a wealth of information on myocardial and coronary structure and function. Not a single technique stands out as “the best”, and the choice should be dictated by patient characteristics, operator and physician expertise, local availability and costs. Hybrid SPECT/CT, PET/CT and PET/MRI imaging is now emerging. The combination of functional and anatomical insights holds much promise for future applications.
Case examples
45-year-old male with some compressing pain, mainly when exercising
There is a high suspicion of exercise-induced angina. Fractional flow reserve derived from computed tomography (FFRCT) would be a good modality for the evaluation of this patient.
53-year-old female with pain, not always when exercising
The symptoms are not clearly related to exercise. A comprehensive cardiac MRI exam with stress or myocardial perfusion imaging will provide information on chamber anatomy, wall motion, possible valve pathology and ischaemia.
80-year-old male with pain largely when not mobile or with some level of exercise
A “triple rule-out” strategy based on a CT scan of the thorax, i.e., one scan permitting the evaluation of the pulmonary arteries, thoracic aorta and coronary arteries, would be useful in this setting. This would include a coronary CT angiography.