Cardiac involvement in Fabry Disease – clues for the cardiac imaging specialist
Cardiac involvement is one of the three major causes of morbidity and mortality in Fabry disease (FD), together with end-stage renal disease and cerebrovascular events [1]. The cardiovascular manifestations of FD include left ventricular hypertrophy (LVH) also involving the papillary muscles, rhythm and conduction abnormalities, valvular dysfunction and ischemic heart disease. The cardiovascular changes appear to be exhibited by affected women in a similar proportion to men, but at a later age [2].
The main feature of cardiac involvement in FD is LVH. Several groups have investigated the prevalence of FD in adult patients with unexplained LVH and obtained with rates between 0% and 12%, reflecting referral and gender bias as well as differences in diagnostic methodology. More recently, Palacek et al [3] performed a systematic screening in 100 men with unexplained LVH, defined as maximal wall thickness ≥13 mm, and found a prevalence of 4% of FD in this group, leading them to recommend screening, even in the absence of obvious extracardiac manifestations of FD. Due to the fact that LVH in Fabry disease can mimic hypertrophic cardiomyopathy (the non-obstructive form, but also possibly the obstructive phenotype), the differential diagnosis can be a challenge.
Another associated pathologic feature can be the localized thinning of the LV basal posterior wall which is generally related to localized fibrosis [4].
Myocardial ischemia in FD is due to endothelial dysfunction of coronary arteries and also to the increased oxygen demand of hypertrophied myocardium, being another contributor to the late development of myocardial fibrosis. There is generally no large coronary artery disease.
Over time, these cardiac complications can progress to heart failure, life-threatening arrhythmias and, rarely, myocardial infarction (MI). Published data from the Fabry Registry [5] indicate that, during the natural history of the disease (without or before enzyme replacement therapy [ERT]), 4.8% of patients had experienced a major cerebrovascular (CV) event (heart failure and myocardial infarction).
In the early 1990s, there were several reports of a form of FD confined to the heart. Patients with this cardiac variant had residual enzyme activity (approximately 1-5% of normal values) and presented in the fifth and sixth decades of life with LVH and conduction disease without classic manifestations such as angiokeratoma, acroparesthesia, hypohidrosis, and characteristic ophthalmological changes [6,7].
Imaging the heart in Fabry Disease
Echocardiographic features
The main feature of cardiac involvement in FD is left ventricular hypertrophy (Figure 1A, Figure 1B). However, as LVH can also be found in 15-20% of individuals based on the Framingham cohort [8], due to a diversity of etiologies, one of the questions for the cardiac imager is if any of the features related to the LVH pattern or particularities could lead the cardiologist towards an FD diagnosis.
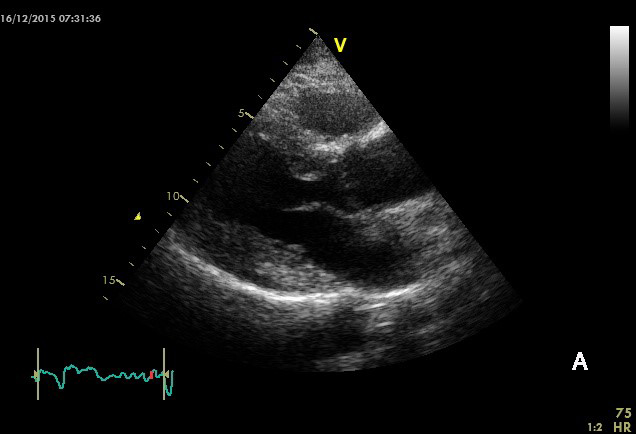
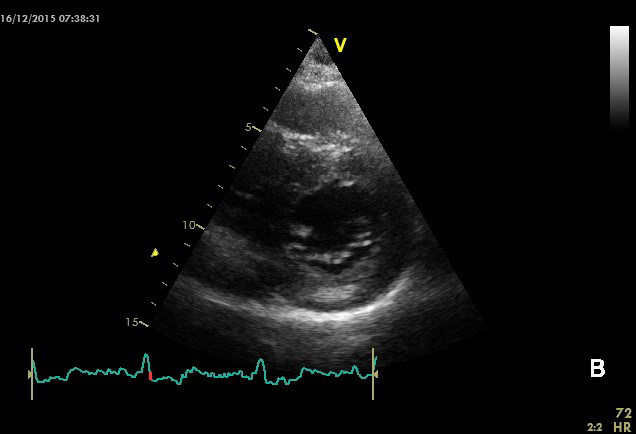
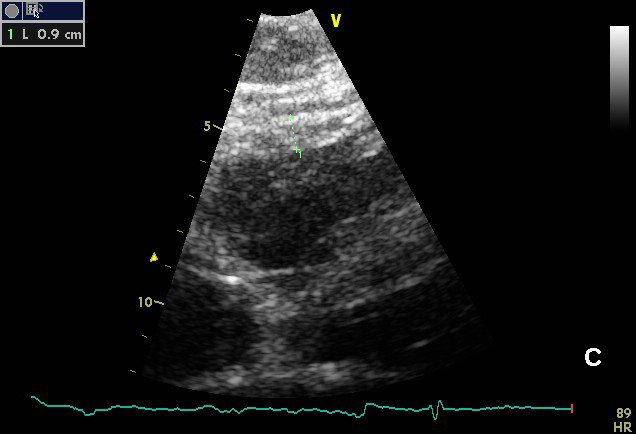
Figure 1. Cardiac hypertrophy in a patient with Fabry disease. A. and B. Concentric LV hypertrophy. Note the presence of a hyperechogenic region in the posterior wall (mid-wall level, arrow), corresponding to localized fibrosis. C. Right ventricular free wall hypertrophy from subcostal view.
In most cases of FD, the LVH is concentric and non-obstructive; however, an asymmetrical hypertrophy with septal thickening and posterior wall fibrotic thinning may present in advanced cases. There have also been rare case reports of patients with obstructive forms of hypertrophic cardiomyopathy. The LVH is progressive in nature, and is rarely severe in children or adolescents. Of note, the echocardiographically derived cardiac mass is proportional to the electrocardiographic LVH low-voltage on the ECG, presenting an argument against Fabry disease in these patients.
Right ventricular (RV) hypertrophy is also common [9] (around 70% of Fabry patients display it) and may progress to RV dilation (Figure 1C). No late gadolinium enhancement (LGE) was described in the RV wall in cardiac MRI studies, showing the absence of fibrosis at this level. Apparently, RV hypertrophy directly correlates to LV changes, suggesting that the degree of RV involvement in Fabry disease is related to the LV cardiomyopathy stage.
After first being described as an anecdotal finding in Fabry patients, the papillary muscle hypertrophy which develops together with LVH was more recently proven to be usable as an echocardiographic marker for the detection of Fabry patients with concentric LV hypertrophy [10], while this was not seen in patients with other etiologies of LVH (hypertension, amyloidosis, Friedreich ataxia).
Progressive systolic and diastolic dysfunction develops with age in FD patients. As in other infiltrative diseases, a drop in LV ejection fraction is a late event, and other modern imaging techniques are more able to identify early alterations in contractility.
Early reductions of systolic and diastolic tissue Doppler imaging indexes are detected before the onset of myocardial hypertrophy, the longitudinal performance being impaired before the radial one [11] (Figure 2A, Figure 2B). In the study by Pieroni et al comparing FD with and without LVH to normal subjects, tissue Doppler imaging values do not overlap with those of healthy subjects. Lateral and septal Sa and Ea <10 cm/s have near 100% sensitivity and specificity in identifying mutation-positive subjects without LV hypertrophy [12]. In this study, a few of the mutation-positive patients had no other sign of the disease except for decreased longitudinal myocardial function, making it a useful tool for the recognition of preclinical cardiac damage.
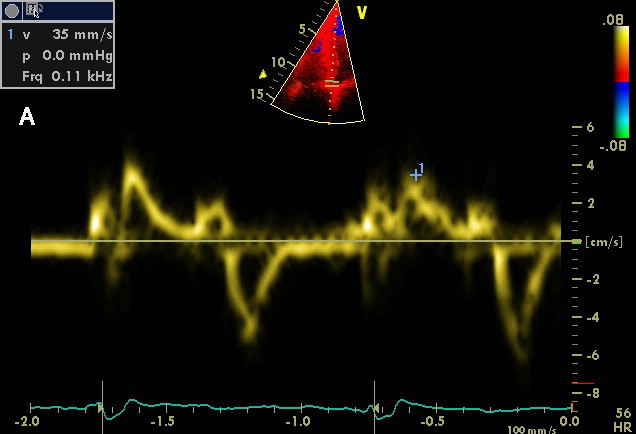
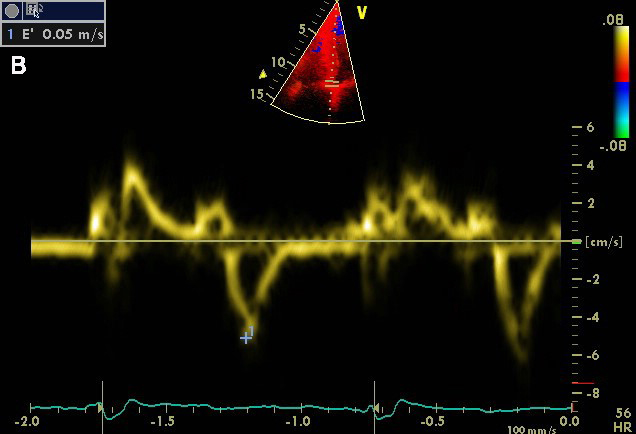
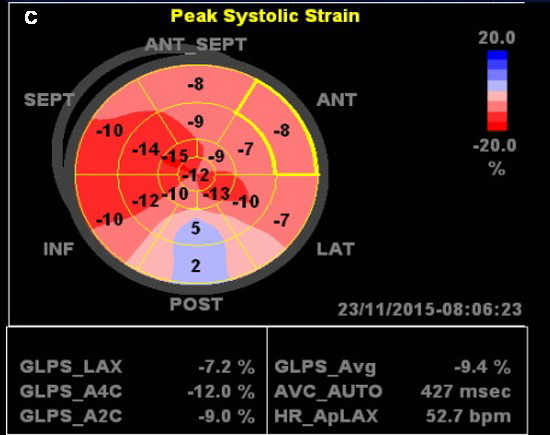
Figure 2. Left ventricular longitudinal myocardial dysfunction in a 72 year old woman with Fabry disease and LV hypertrophy. A. Decreased systolic velocity of the mitral annulus at septal site. B. Decreased early diastolic velocity in the same patient. C. Automated function imaging based on speckle tracking echocardiography shows decreased LV global longitudinal strain, with severe changes in the posterior basal segments.
Myocardial fibrosis is an important feature in Fabry cardiomyopathy and is associated with disease progression and severe prognosis. Therefore, finding a non-invasive, available method to identify this structural alteration is highly relevant.
Using LGE from cardiac MRI as the gold standard for fibrosis localization, Weidemann and co-workers evaluated by strain rate imaging regional deformation in 30 patients with hypertrophic cardiomyopathy, severe aortic valve stenosis and Fabry disease cardiomyopathy, as well as 10 healthy controls. Using the strain rate curves, all LGE positive segments displayed a characteristic pattern consisting of a first peak in early systole followed by a rapid fall in strain rate close to zero and a second peak during isovolumetric relaxation. The authors defined this as the “double peak sign” which seems to be a reliable tool for the diagnosis of regional fibrosis.
While tissue Doppler imaging-derived strain and strain rate need a longer learning curve and more expertise for the cardiologist, clinical practice has lately moved more towards using speckle tracking imaging for assessing global and regional LV longitudinal deformation. Using this technique, Krämer et al [13] showed that LV global longitudinal strain is depressed mainly in affected men, and significantly more in patients with myocardial fibrosis on cardiac MRI LGE sequences. They also demonstrated that systolic strain in basal posterior or lateral segments is the most powerful predictor for LGE, in keeping with the typical distribution of myocardial fibrosis in Fabry cardiomyopathy (Figure 2C). Interestingly, posterior wall (PW) thickness (or PW/septum ratio) did not appear to predict the presence of fibrosis. When looking for a cut-off value for systolic strain for the detection of LGE, the authors found that strain values in one of the affected segments lower than -12.5% indicated LGE with a specificity of 97% and a sensitivity of 90%, while patients with strain in those segments higher than -16.5% had no pathological LGE (100% specificity and 89% sensitivity).The authors conclude that 2D speckle tracking imaging is an easy, reliable, and reproducible echocardiographic tool for the non-invasive evaluation of LGE-related functional abnormalities in patients with FD.
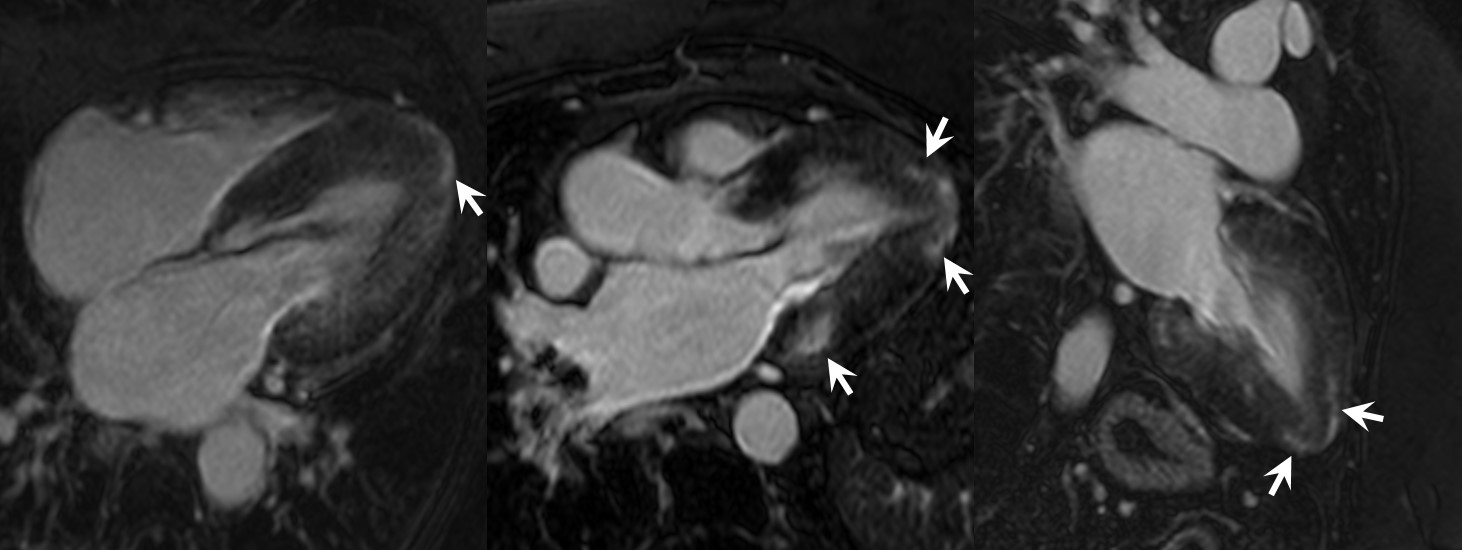
Figure 3. Cardiac MRI - Late gadolinium enhancement images in 4-, 3- and 2-chamber in a 59-year old Fabry patient showing intramural enhancement in the basal inferolateral wall (patognomonic) as well as in the apical segments (arrows). In addition, important concentric hypertrophy is noted together with the impossibility of optimally negating the suggestion of diffuse fibrosis in the rest of the segments of the myocardium. (Courtesy of Dr Anca Florian. Reproduced with permission from [2]).
No significant valvular changes were described in Fabry patients. While mild LV valve regurgitations are frequent in FD, they do not appear as major pathogenic changes in FD patients [14].
Cardiac MRI
Cardiac MRI can offer information regarding LV hypertrophy, measurements of LV mass, RV structural changes, as well as, through the LGE sequences, data on the presence of fibrosis and scarring.
The localization of LGE in Fabry cardiomyopathy has a few typical features [15]: it is characterized by the predominant involvement of the inferolateral basal or mid basal segments and a mid-wall distribution sparing the subendocardium (Figure 3).
(Insert Figure 3)
Using cardiac MRI to quantify myocardial fibrosis and following a longitudinal protocol, Krämer et al [16] showed that myocardial fibrosis relates to malignant ventricular arrhythmias (non-sustained and sustained ventricular tachycardia, sudden cardiac death), with subjects with a high annual increase in LV fibrosis being at highest risk for sudden cardiac death.
Although LGE imaging is the non-invasive gold standard for the evaluation of replacement fibrosis, there are some limitations to its use: end-stage renal disease, presence of a cardiac defibrillator or pacemaker, limited availability of the technique in many countries. Thus, in these groups of patients, echocardiography remains the only available option, and, as shown before, 2D speckle tracking imaging was proven to be an excellent option for the indirect assessment of LGE.
More recently, new cardiac MRI techniques without the use of contrast agents have been developed. Cardiac MRI T1 mapping has been developed as a non-invasive technique to estimate extracellular volume (ECV), as ECV expansion is a key feature of heart failure. Kammerlander et al showed that, in a population of patients with LV hypertrophy of various etiologies, cardiac MRI T1 mapping allows accurate non-invasive quantification of ECV and is independently associated with event-free survival among imaging parameters [17]. However, more data are necessary before using it in routine clinical practice.
Impact of treatment
Published data from the Fabry Registry [18] indicate that, in patients with baseline cardiac hypertrophy, treatment resulted in a sustained reduction in left ventricular mass (LVM) index after five years and a significant increase in mid-wall fractional shortening. However, data coming from several groups showed that this reversibility is only consistent in patients with no or mild cardiac fibrosis [19].
Moreover, in two studies, Beer et al [20] and Krämer et al [16], using cardiac MRI with LGE for longitudinal follow-up of FD patients, it appeared that, regardless of ERT, cardiac fibrosis progresses over time, with no possibility of regression. Therefore, the implication of these data is that treatment of Fabry cardiomyopathy with recombinant α-galactosidase A should best be started before myocardial fibrosis has developed in order to achieve long-term improvement in myocardial morphology and function and exercise capacity.
Conclusion
In conclusion, cardiac imaging can be of great help in raising the suspicion of Fabry disease in a patient with LVH, if the cardiologist is aware of the described echo and MRI “red flags” for this diagnosis. In this systemic disease, these features should always be combined with features of the clinical examination, laboratory tests and electrocardiogram, in order to build a comprehensive diagnostic algorithm. Also, patients with known Fabry disease should be screened early for cardiac involvement, as cardiovascular involvement is an important mortality cause, and treatment benefit may not be seen once cardiac fibrosis has developed.















