Keywords
atrial fibrillation
bradycardia
cardiac resynchronisation therapy
leadless pacemaker
transcatheter pacemaker
Background
Electrical stimulation is today’s gold standard for the treatment of symptomatic bradycardia following major advances since the first implantable pacemaker in 1958. Pacemaker (PM) implantation improves symptoms, syncope burden, and improves survival in high-risk patients [1]. Technical improvements have resulted in improved battery longevity and device size. However, although highly reliable, complications remain a serious challenge for both patients and physicians, presenting in up to 20% of patients within five years, most frequently related to pacemaker leads and/or pulse generator pockets [1,2]. Furthermore, conventional transvenous lead placement is not feasible in all patients. It is possible that miniaturised, leadless PM might overcome some of these limitations, in addition to the cosmetic advantages [2,3]. Moreover, leadless systems have the potential to minimise implant-related post-procedural restrictions of physical activity regarding the upper extremity, just as they have in subcutaneous defibrillator implantations, where patients have no left arm movement restriction postoperatively [4]. In recent years, biological pacemakers have been under investigation but are still not available for clinical use. The first prototype of a completely endocardial implantable pacemaker was presented in 1970 [5]. Since then, different leadless systems with different energy sources and myocardial fixation systems have been developed [6], resulting in the CE certification of two right ventricular single-chamber pacemaker systems (NanostimTM; St. Jude Medical, St. Paul, MN, USA, and MicraTM; Medtronic, Minneapolis, MN, USA) [7,8]. Moreover, the feasibility of left ventricular endocardial stimulation for cardiac resynchronisation has been demonstrated [9], even in difficult to treat patients with ischaemic cardiomyopathy [10]. Here, we review the technical aspects and potential pitfalls with regard to leadless pacing.
Technical aspects of available leadless pacemakers
Devices for leadless pacing
Each of the two approved right ventricular single-chamber pacemaker systems (Figure 1) is an entirely self-contained intracardiac device that includes the pacemaker electronics, lithium battery and electrodes. They have been initially investigated in non-randomised, industry-sponsored studies, and both met their primary safety and efficacy goals. The devices have functional properties comparable with conventional VVI-R pacemakers, providing ventricular stimulation, ventricular sensing, inhibited mode and rate response for chronotropic incompetence.
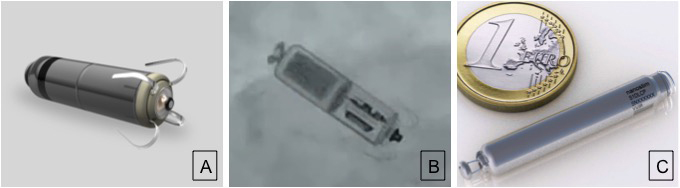
Figure 1. Transcatheter pacemakers for right ventricular pacing.A) Micra TPS (Medtronic). B) Fluoroscopic example. B) Once the tines are attached to the heart wall, a fixation test (“pull and hold”) is performed to assess how many tines are engaged in the tissue. Pulling on the tether creates tension on the tines, which change their shape only if they are embedded in the tissue. This shape change is controlled on a fluoroscopic cine.C) The Nanostim (SJM). Panels A and C are reproduced with permission of Medtronic and SJM.
The devices have similar volumes, approximately 1 cm3, while they differ in length and diameter (Table 1). Both systems are delivered through the femoral vein, via 18 and 24 Fr sheaths, respectively, and have a docking feature which allows attachment to a catheter for delivery, repositioning and retrieval. Current leadless right ventricular pacemakers only pace the right ventricle at present and therefore do not support atrioventricular synchrony. Mean battery longevity is in the range of a conventional pacemaker, between seven and 12 years. Battery longevity depends on pacing needs and pacing output more than in conventional pacemakers. To maximise the device longevity, the pacing output above the identified threshold and the pacing pulse width have been adapted.
Table 1. Characteristics of percutaneous implantable transcatheter pacemakers.
Leadless pacemaker | Micra [16] | Nanostim [15] | ||
|---|---|---|---|---|
Device features | ||||
Volume (cm3) | 0.8 | 1.0 | ||
Length (mm) | 26 | 42 | ||
Diameter (mm) | 6.7 | 5.99 | ||
Weight (gr) | 2 | 2 | ||
Introducer (Fr) | 24 | 18 | ||
Fixation | Self-expanding nitinol tines | Helical wire screw (+nylon tines) | ||
Pacing mode | VVI(R) | VVI(R) | ||
Periprocedural data | ||||
Number of patients | 725 | 526 | ||
Successful implantation (%) | 99.2 | 95.8 | ||
Final device position (%) | Apex Septum Mid-septum Outflow tract | 65. 23.8 7.8 0.6 | Apex Apical septum Outflow/septum/other Missing data | 38.1 19.0 42.7 0.2 |
Procedure duration (min) | 34.8±24.1 | 46.5±25.3 | ||
Fluoroscopy duration (min) | 8.9±16.6 | 13.9±9.1 | ||
Major complications (%) | 4.0 | 6.5 | ||
Device dislodgement (%) | 0 | 1.1 |
The most important differences between the two available systems are related to their delivery systems, fixation mechanisms, rate-response sensors and programming differences.
The Nanostim is fixated through a screw-in helix with a steroid-eluting disc plus angled nylon sutures. The rate response of the system is based on a blood temperature sensor. The programmer interacts with the pacemaker using conducted communication.
The fixation mechanism of the Micra comprises four electrically inactive expandable nitinol tines, providing appropriate fixation if at least two of them are positioned within the myocardium. Rate response is provided by an accelerometer designed to ignore the motion of the heart and detect the motion of the body using filtering and rejection of acceleration due to the heartbeat. Programming is performed using a standard pacemaker programmer.
There are a number of options in cases of battery depletion. The system can be removed, left in place but programmed off, or a new system can be implanted into the right ventricle. In the case of a system being abandoned and a new one implanted, the programmer can be configured to connect with the appropriate device.
Long-term follow-up for these devices is limited to approximately two years. Experimental findings suggest that implantation of multiple devices does not impair ventricular systolic function. However, additional clinical data are warranted. The impact of leadless pacemaker fixation at follow-up and potential explantation is under active investigation as more patients are implanted and followed up over longer periods of time.
Periprocedural patient management and potential pitfalls
There is still limited experience with the currently available leadless systems so careful patient selection is very important. Clinical diagnostics preceding device implantation must be guided by patient history.
In general, transcatheter pacemaker implantation can be considered when a single-chamber VVI system is indicated. They can also be an important option when conventional endocardial or epicardial pacemaker access is not available [11], as we found in two patients with 6 and >12 months of follow-up. Patient characteristics, especially those indicating increased frailty, must be considered when considering a leadless pacemaker compared with a conventional one. Leadless pacemakers should be used with caution in cases of pacemaker dependency or absence of escape rhythm because the follow-up data regarding device performance are limited. Relevant contraindications are summarised in Table 2.
Table 2.
Present relative and absolute contraindications for transcatheter pacemaker implantation. |
|---|
Pacemaker dependency Pacemaker, ICD, CRT, neurostimulator or any other implanted device which uses electrical current Unstable angina pectoris, recent myocardial infarction Mechanical tricuspid valve Implanted vena cava filter Left ventricular assist device Morbidly obese where telemetric programmer communication can be limited Limited or missing femoral venous access or stenosis Unable to tolerate emergency sternotomy Intolerance to titanium or nickel-titanium (nitinol) alloy |
Surgical intervention during leadles pacemaker implantation may be necessary in rare cases, just as it is occasionally during conventional pacemaker procedures. Appropriate infrastructure and availability of appropriately trained medical staff are essential. In most centres, implantation is performed in electrophysiology laboratories or hyprid operating rooms on patients under conscious sedation. Antibiotic and anticoagulation regimens are left to the operators and local practice.
An introducer is advanced using a stiff guidewire and dilator into the right atrium. The system is advanced under fluoroscopic guidance towards the right ventricle across the tricuspid annulus using the steerable delivery catheter. The use of the delivery systems can result in complications related to either the femoral access site or catheter manipulation within the heart. Contrast can be useful in some patients to assess a tortuous venous anatomy, which might challenge cardiac access with the relatively large sheath, 24 Fr for the Micra and 18 Fr for the Nanostim, in some patients, as well as to define the optimal right ventricular position for device deployment. Successful implantation in the right ventricular apex, septum, and right ventricular outflow tract has been performed. However, device embolisation needs to be considered. In general, a left anterior oblique view to ensure a septally directed positioning is recommended. The device is finally deployed after successful fixation and documentation of appropriate electrical performance characteristics.
Different techniques have been adopted for successful closure of the venous access at the end of the procedure given the sheath sizes. The technique of subcutaneous “figure of eight“ suture to achieve hemostasis after removel of the femoral venous sheath and “purse-string“ suture closure have been described and appear to create secure and cosmetically appealing closures [12]. The different closure devices which are available for arterial access sites have also been reported for venous access sites, but it must be remembered that these have not been investigated systematically for venous access sites. Whether a foreign body in a venous blood vessel could trigger thrombosis and/or embolism remains unknown [12].
Post-procedurally, patient monitoring is routinely performed until an echocardiogram and routine pacemaker interrogation have been performed. There may be some circumstances where a leadless pacemaker needs to be retrieved, e.g., high thresholds. Experimental studies in animals have demonstrated the ability to extract leadless pacemakers safely percutaneously. There are case reports [13,14] describing the successful extraction of a leadless pacemaker during short-term follow-up. The concept of leadless pacemaker implantation and subsequent retrieval has also been used as a bridge-to-reimplantation for a patient with severe lead endocarditis before device reimplantation for cardiac resynchronisation therapy [14]. Noteworthy, encapsulation of a transcatheter implantable pacemaker is not yet fully understood, and the timing of optimal device implantation and retrieval needs to be determined.
A single report on a patient who underwent orthotopic heart transplant indicated that the leadless pacemaker with nitinol tines was already almost completely endothelialised after four months [15]. An autopsy description of changes one year after implantation, from a patient who died from respiratory failure caused by progression of pre-existing severe pulmonary fibrosis, indicated that the extent of the well-known phenomenon of inflammation and fibrosis might be less around a sole intracardiac device compared with conventional pacemaker leads [16]. Microscopic analysis from another patient, who died because of an irresectable cholangiocarcinoma 19 months post implant, revealed that the leadless pacemaker fixated through a screw-in helix was ≈60% covered with a thin fibrous capsule [17]. However, no final conclusions can be drawn from these few cases and how this limited information might impact on device explantation procedures, follow-up, and patient outcome. Time from implant to explant may well play its part, just as it does with conventional leads. It is expected that at the end of service of one leadless device, implantation of a new one, adjacent to the original site, might be the therapy of choice [2]. How implantation of multiple devices will be appropriately incorporated into patient care requires investigation.
Conclusions and outlook
Percutaneous implantable transcatheter pacemakers are of increasing importance for the treatment of patients with bradycardia.
The impact of specific patient characteristics, e.g., age, gender, comorbidities, vascular access and prior device implantation, on the safety and efficacy of this treatment needs to be determined. Safety and long-term outcome in patients with leadless devices need to be evaluated in more detail, including larger patient cohorts.
Future technical developments will, hopefully, identify new avenues for electrical leadless stimulation in other cardiac chambers simultaneously. Meanwhile, communication between different devices within the heart in conjunction with long-term device fixation in various chambers and positions including the anatomically distinct right atrium needs to be established. Noteworthy, there are compelling data indicating a potentially significant clinical benefit of leadless left ventricular endocardial pacing compared with epicardial pacing. One innovative approach, currently under investigation, is a leadless left ventricular endocardial, ultrasound-based pacing system, Wireless Cardiac Stimulation (WiCS®-LV) system (EBR Systems, Sunnyvale, CA, USA) (Figure 2) [9,10]. An ultrasound transmitter and battery are implanted in an intercostal space and left midaxillary at the level of the 5th-6th intercostal space, respectively. An electrode, ultrasonic receiver and transducer, is implanted on the left ventricular free wall using a retrograde aortic approach. This electrode replaces the requirement for a coronary sinus lead and its associated problems. Ultrasound energy received by the electrode is transduced to electrical energy to cause the left ventricle to contract. This system must be implanted with a co-implant, pacemaker, ICD, with the exception of the S-ICD, or cardiac resynchronisation system. The leadless system is triggered off a right ventricular pacing pulse and the left ventricle generally contracts within 3 ms, thereby effectively delivering synchronous biventricular pacing. Battery longevity has been reported as a limitation. Although not reported to date, it is theoretically possible that long-term ultrasound energy exposure to subcutaneous or myocardial tissue in humans may have unintended adverse consequences. In addition, it is not fully understood how environmental interference and changes in the acoustic window might influence the system’s sensing or pacing performance. Misalignment requirements with the technology may result in less efficient energy use in a system with an already comparatively short battery life.
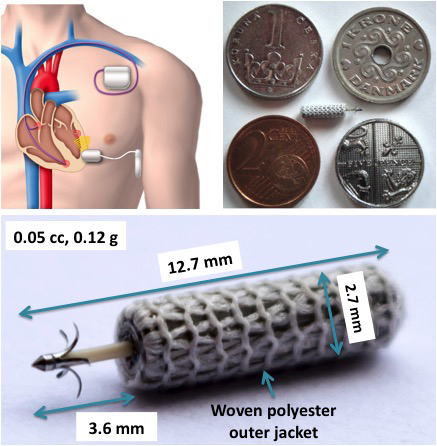
Figure 2. Hybrid device therapy including endocardial left ventricular stimulation. Bi-ventricular pacing with existing pacing systems. Upper panel: overview of the system for left ventricular endocardial leadless pacing (WiCS-LV system). The system can be co-implanted with any conventional pacemaker, ICD, or CRT device. The pulse generator (transmitter), implanted subcutaneously, generating acoustic energy at ultrasonic frequencies (ultrasound) is shown. A small receiver-electrode (electrode) implanted on the left ventricular wall, converts the acoustic energy to an electrical pacing pulse (upper right and lower panel).
Initial limited findings have shown that combining a right ventricular leadless pacemaker with other devices including subcutaneous implantable defibrillators is technically feasible [18]. An intravascular cardioverter-defibrillator might be another option for some patients [19]. A leadless right ventricular pacing system will shortly be implanted with leadless left ventricular options. The pulse widths and amplitudes available from the right ventricular leadless systems are compatible with those of the left ventricular leadless system, albeit using more energy in the process. However, more data on safety and performance in combination with additional innovations will demonstrate how leadless 1-, 2-, and 3-chamber pacemakers or defibrillators will expand the armamentarium to treat patients with heart rhythm disorders [20].















